 Quick Reference — To correct ADNPATIENT claims
Quick Reference — To correct ADNPATIENT claims
Worklist: HOLD
Issue: The payer has indicated that additional information from the patient is needed to complete the adjudication process. athenahealth attempts to address this error on your behalf. If athenahealth is not able to correct this error, the claim resolution becomes your responsibility.
Next Steps: Please contact the patient to correct insurance and/or coordination of benefits information OR transfer the remaining balance on the claim to patient responsibility.
- Contact the patient.
- Make necessary corrections and resubmit the claim.
- Transfer the balance.
Note: If after acting on this error, the claim remains in a hold status (HOLD or MGRHOLD), the claim requires additional review or work.
athenahealth offers a feature that can help reduce the number of ADNPATIENT denials that are routed to your worklists by automatically sending statements to patients instead.
When this feature is enabled, athenaOne automatically transfers the outstanding balance to the patient. After the balance is transferred, athenaOne generates a statement that is sent to the patient; this statement indicates that the patient should contact the insurer to provide the necessary information to determine coverage.
This feature applies only to claims that meet the following criteria. These criteria are designed to prevent inappropriate patient billing, such as billing patients with Medicaid balances.
- ADNPATIENT is the only driving denial on the claim (that is, there are no other denial codes with a next claim status, no adjustments, and no transfers).
- ADNPATIENT is received on the EOB/ERA and was not manually kicked by a user.
- ADNPATIENT is received on a primary claim and no other insurance is registered for the patient.
- The billed insurance package is not government-funded (that is, not Medicare or Medicaid).
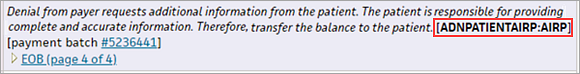
You can identify claims that were moved to the patient because of this feature as follows: an automatic patient balance transfer occurs immediately after receipt of an ADNPATIENT denial, and this action is indicated with the kick code AIRP in the claim note.
To enable this feature, please open a support case from athenaOne > Support > Success Community > Contact Client Support Center.
- Display the Claim Action page: Select a claim from the Workflow Dashboard, Claim Worklist, or click the Claim Action Page link on the Claim Edit page
- Review the claim notes.
- Ask the patient to contact the insurance carrier to update/carrier coordination of benefits.
Note: At least one change must be made to the claim before it can be resubmitted. It is not compliant to resubmit a claim without changes only to see whether the claim will be paid if you resubmit it to the payer.
- Display the Claim Action page: Select a claim from the Workflow Dashboard, Claim Worklist, or click the Claim Action Page link on the Claim Edit page.
- Review the claim information.
- Actions — If the claim needs to be resubmitted to the payer, select Add Kick Reason.
- Make any necessary changes to the claim details.
- Kick reason — Enter DRPBILLING.
- Claim note — Enter a clear, detailed note for athenaOne users, describing what actions have just been taken.
- Click Submit.
- Display the Claim Action page: Select a claim from the Workflow Dashboard, Claim Worklist, or click the Claim Action Page link on the Claim Edit page.
- Review the claim information.
- Actions — Select Transfer Balance.
- Select the charges that you want to adjust.
- Transfer to — Select Patient or Next Payer.
Note: Both options map to kick reasons, so reporting is unaffected. - Claim note — Enter a claim note to indicate why the balance is being transferred.
- Click Submit. Claims with a balance transferred to Patient are kicked with PTRESP; claims with a balance transferred to Next Payer are kicked with NEXTPAYOR.
- On the Claim Edit page, scroll down to the Claim Notes section at the bottom of the page
- Review the claim notes.
In the notes, the payer is requesting additional information from the patient/insured, or the patient needs to update coordination of benefits with the payer - After reviewing the notes, ask the patient to contact the insurance carrier to resolve the issue.
Note: At least one change must be made to the claim before it can be resubmitted. It is not compliant to resubmit a claim without changes only to see whether the claim will be paid if you resubmit it to the payer.
- On the Claim Edit page, scroll down to the Claim Notes section at the bottom of the page
- Review the claim notes.
- If athenahealth has researched the denial with the payer, a detailed description will be included.
- If there is an EOB or letter from the payer, click the link to review.
- If further clarification is needed, contact the payer directly.
- Applies to — Select the correct insurance type
- Status — Select DROP
- Kick reason — Enter DRPBILLING
- Claim Note — Enter a clear, detailed note that tells future viewers of this claim what actions have just been taken
- Click Save.
- On the Claim Edit page, scroll down to the Claim Notes section at the bottom of the page.
- Review the claim notes.
- Action Taken/Note Source — Select Generic Note/From Other Source.
- Kick Reason — Select PTRESP.
- Claim Note — Enter a note to indicate why the balance is being transferred to the patient.
- Click Save. A statement will be sent to the patient.