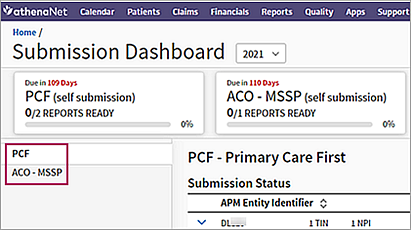
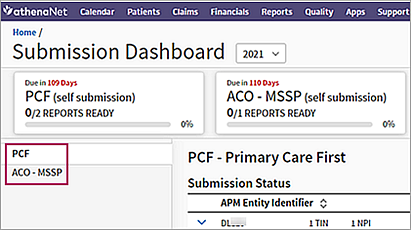
Submission Dashboard
The Submission Dashboard enables you to track data for the PCF and ACO MSSP quality programs, as well as your MIPS Value Pathways (MVP) submission status. On this dashboard, you can download your program data as QRDA III and JSON files for submission to CMS.
On the Main Menu, click Quality. Under REPORTS, click Submission Dashboard
To access the Submission Dashboard and to view and edit the attestation options, you must have the Quality Manager role.
- Display the Submission Dashboard: On the Main Menu, click Quality. Under REPORTS, click Submission Dashboard.
- On the left side of the Submission Dashboard, click the name of the quality program whose data you want to view (the PCF program is selected by default).
The Submission Status table shows information for the program you selected. - Click any row in the table to expand it and see the TINs, NPIs, and clinicians included in the APM entity identifier.
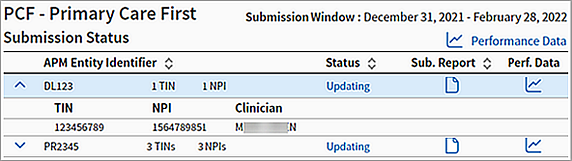
- To see performance data at the program level (that is, not specific to an APM entity ID), click the Performance Data icon
 at the top of the Submission Status table.
at the top of the Submission Status table.
The eCQM Data page opens and displays the measure performance data for the selected program. (On the eCQM Data page, the quality program is already selected in the Programs filter field.) - To see performance data at the APM entity ID level, click the Performance Data icon
 in the APM Entity Identifier row.
in the APM Entity Identifier row.
The eCQM Data page opens and displays the measure performance data specific to the APM entity — for example, the PCF practice site ID. (On the eCQM Data page, the quality program is already selected in the Programs filter field and the PCF practice site ID or ACO entity ID is already selected in the APM Entity Identifier filter field.)
You can see the submission report for the quality program when the program data is in certain statuses, such as "Export Ready" or "Updating."
Note: If you are submitting ACO MSSP or PCF data to CMS yourself but much of your quality data for the program exists outside athenaOne, you can use the eCQM Data page to export a QRDA I file that contains the athenaOne data to be aggregated with the rest of your data (see To export QRDA I or QRDA III files).
- For both the PCF and ACO MSSP programs, the default submission method is manual (Self Submission). However, if your organization is enrolled in the ACO MSSP program, you can request that athenahealth automatically submit your data if all providers who are part of the ACO are using athenaClinicals under the same practice ID.
- On the Main
Menu, click Support > Success Community > Contact Client Support Center.
The case classification page appears. - Click the Quality Management category.
The Quality Management subcategories appear. - Click Quality Management/P4P and then click Create Online Case.
The case creation page appears. - Enter the information requested in the fields and then click Create Online Case.
A case confirmation page appears with the case number.
Important: The deadline to make a decision about auto submission versus self submission for the ACO MSSP program is January 14, 2022.
- On the Main
Menu, click Support > Success Community > Contact Client Support Center.
- Display the Submission Dashboard: On the Main Menu, click Quality. Under REPORTS, click Submission Dashboard.
- On the left side of the Submission Dashboard, click the name of the quality program whose data you want to view (the PCF program is selected by default).
The Submission Status table shows information for the program you selected. - Click any row in the table to expand it and see the TINs, NPIs, and clinicians included in the entity identifier.
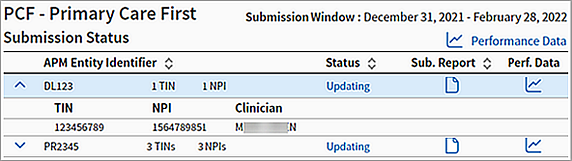
- Click the Submission Report icon
 to display page 2 of the report.
to display page 2 of the report.
The Submission Report page shows you the aggregated performance data for the program entity — that is, the PCF practice site ID or the ACO MSSP entity ID. - Click any measure row in the report to expand it and see the detailed data for the measure.
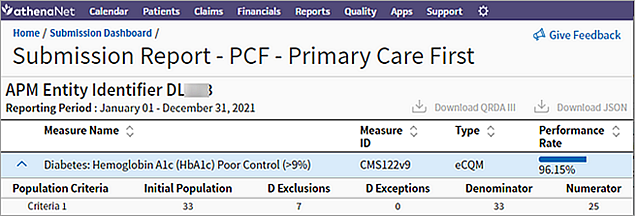
- When the submission window opens for the quality program (generally after January 15), you can download the files that you need to submit to CMS.
- For eCQM artifacts, click the Download QRDA III link.
- For CQM artifacts, click the Download JSON link.
-
Display the Submission Dashboard: On the Main Menu, click Quality > Submission Dashboard.
-
Select MIPS Value Pathways and the appropriate MVP Group or MVP Individual tile.
-
Review the category columns (Quality Status, IA Status, or PI Status) to see your MVP submission status.
The Submission Dashboard enables you to track submissions for these quality programs:
Providers and quality managers access the Submission Dashboard as follows: On the Main Menu, click Quality. Under REPORTS, click Submission Dashboard.
At the top of the Submission Dashboard, you see a tile for the PCF program if you are enrolled in PCF and a tile for the ACO MSSP program if you are enrolled in that program. The fraction below the program name indicates the number of reports that are ready for submission (the numerator) over the total number of enrollments (practice site IDs or ACO entity IDs) in each program (the denominator).
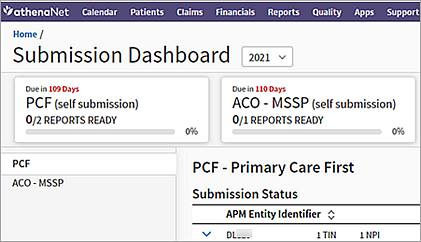
The list on the left side of the Submission Dashboard lists the quality programs. Click the program name in the list to display the dashboard for the PCF or ACO MSSP program.
In both the PCF and ACO MSSP dashboards, the Submission Status table shows the status and details of participants in the quality program. Click a column heading to re-sort the list of items.
For both the PCF and ACO MSSP programs, the default submission method is manual (Self Submission). However, if your organization is enrolled in the ACO MSSP program, you can request that athenahealth automatically submit your data (from athenaOne > Support > Success Community > Contact Client Support Center).
Important: For the ACO MSSP program, the deadline to make a decision about auto submission versus self submission is January 14, 2022.
In both the PCF and ACO MSSP dashboards, the state of your data is shown in the Status column in the Submission Status table.
| Self Submission Status (PCF and ACO MSSP programs) | |
|---|---|
| Processing |
Your data is being processed and will be available to export when ready. |
| Updating | Data is being updated and will be processed for submission during the submission time frame. |
| Export Ready | Your data is ready for export. |
| Auto Submission Statuses (ACO MSSP program only) | |
| Processing | Your data is being processed and will be automatically submitted when ready. |
| Updating | Data is being updated and will be processed for submission during the submission time frame. |
| Awaiting submission | athenahealth is prepared to submit the ACO data on your behalf. |
| Requirements Unmet | athenahealth was unable to generate your submission data because you were not enrolled in all mandatory measures for the program. |
| Submitted | athenahealth has submitted data to the program steward on your behalf. |
The Primary Care First (PCF) program is a voluntary five-year alternative payment model that is based on the underlying principles of the Comprehensive Primary Care Plus (CPC+) program (2021 is the final year for the CPC+ program). The PCF program aims to support the delivery of advanced primary care. The first year of the PCF program is 2021.
Note: For more information, see this CMS.gov information page.
You can report on PCF program performance at the provider or practice-site level for all four PCF quality measures (three eCQMs and one Care Plan CQM) on the Quality Management Reporting page.
- Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%) (CMS122v9)
- Controlling High Blood Pressure (CMS165v9)
- Colorectal Cancer Screening (CMS130v9)
- Advance Care Plan (Quality ID 47)
On the eCQM Data page, you can create a report at the practice-site level.
Note: CMS requires practice-site level reporting of all quality gateway measures for PCF via QRDA III for eCQMs and JSON for CQMs; only providers on your provider roster who have been linked to a specific practice site ID appear in the submission files. You can download the files that you need to submit to CMS on the Submission Dashboard page.
Enrollment in the Primary Care First (PCF) program
If you choose to participate in the PCF program, you are responsible for maintaining accurate enrollment during the performance year. You must both enter a practice site ID for a provider or medical group and assign a PCF practice site ID to a department. See To enroll in the Primary Care First (PCF) program.
You can enroll in PCF as follows:
- Enter your practice site ID on the Department Numbers page (see To assign a PCF practice site ID to a department). For more information about the practice site ID, see APM Entity Identifier filter (practice site ID).
- Create your provider roster for the PCF program on the NPIs and Other Numbers page (see To enter a PCF practice site ID for a provider or medical group). Providers and medical groups are enrolled in all four quality gateway measures.
To enroll a provider or medical group in the Primary Care First (PCF) quality program in athenaOne, you must associate the provider or medical group with a PCF practice site ID on the NPIs and Other Numbers page (see To enter a PCF practice site ID for a provider or medical group). A script locates providers associated with a PCF practice site ID and automatically enrolls them in the PCF program.
Note: You do not need to open a support case to enroll a provider or medical group in the Primary Care First quality program.
After a provider is enrolled in the PCF program:
- All PCF measures appear on the Quality Management tab in the patient chart for patients of enrolled providers.
- PCF data for the enrolled providers is available on the Quality Management Reporting page.
- PCF data for the entire organization is available on the eCQM Data page.
Note: After you associate a PCF practice site ID with a provider, you should see data for the provider in reports and see the PCF measures on the Quality Management tab within 48 hours.
If a provider is removed from the PCF roster at any point, the provider is unenrolled from the PCF program and is not included in any submission files.
The Medicare Shared Savings Program (MSSP) is a voluntary type of Accountable Care Organization (ACO) managed by CMS. In 2021, CMS introduced the Alternative Payment Model Performance Pathway (APP). MSSP ACOs are required to report via the APP and have two options to meet the quality reporting standard:
- 10 Web Interface measures
- 3 eCQMs/MIPS CQMs
You can report on ACO MSSP program performance at the provider or ACO entity level for all three MSSP quality measures on the Quality Management Reporting page and on the eCQM Data page.
- Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%) (CMS122v9)
- Controlling High Blood Pressure (CMS165v9)
-
Preventive Care and Screening: Screening for Depression and Follow-Up Plan (CMS2v10)
Note: CMS requires practice-site level reporting of all quality measures for ACO MSSP via QRDA III files; only providers in medical groups that have been linked to a specific ACO entity ID appear in the submission files. You can download the files that you need to submit to CMS on the Submission Dashboard page.
Enrollment in the ACO MSSP program
If you choose to participate in the ACO MSSP program and submit your data using the eCQM option, you are responsible for maintaining accurate enrollment during the performance year.
To enroll a medical group in the ACO MSSP quality program in athenaOne, you must associate the medical group with an ACO entity ID on the NPIs and Other Numbers page (see To enter an ACO entity ID for a medical group). After you add your ACO entity ID to a medical group, the corresponding TIN is enrolled in the program.
Note: A script locates providers associated with an ACO entity ID and automatically enrolls them in the ACO MSSP program. You do not need to open a support case to enroll a medical group in the ACO MSSP quality program.
After a provider is enrolled in the ACO MSSP program:
- All ACO MSSP measures appear on the Quality Management tab in the patient chart for patients of enrolled providers.
- ACO MSSP data for the enrolled providers is available on the Quality Management Reporting page and on the eCQM Data page.
Note: After you associate an ACO entity ID with a medical group, you should see data for the medical group in reports and see the ACO MSSP measures on the Quality Management tab within 48 hours.
| APM Entity Identifier |
Alternative Payment Model (APM) entity identifier, that is, the unique ID for the quality program.
|
| Status | State of your preparation for submission of the program data (see Statuses in the Submission Status table). |
| Sub. Report | Available during the submission window when the status is "Export Ready" or "Updating." When you click the Submission Report icon |
| Perf. Data | The icon in this column is a link that opens the eCQM Data page with the performance data for the selected APM entity ID displayed — that is, the PCF practice site ID or the ACO MSSP entity ID. |