Readjudication Notice Type
A Readjudication Notice record represents a notification from the payer indicating a new adjudication to a previously processed claim — that is, a determination change that results in a different level of reimbursement. Unlike Balance Forward remittance records, Readjudication Notice records are always claim specific and are not associated with a rolling balance.
The change in payment is made non-financial in the batch by the reporting of a batch exception that fully offsets the change in claim-level reimbursement.
Readjudication Notice records are often resolved when your practice sends a refund to the payer. As long as the refund is posted as a refund on the claim, athenahealth will reverse the Readjudication Notice posting process and close the record.
If a provider takeback is then received from the payer for the same claim, it indicates that they did not acknowledge the receipt of the practice refund. The Readjudication Notice remittance record is re-opened and both it and its associated Provider Takeback remittance record will be returned for your review.
Find a copy of the front and back of the refund check you sent to the payer, and call the payer from whom the remit originated. Get confirmation from the payer of the receipt and cashing of the refund check. The payer should then recognize the refund took place and send out a rebate check notice to give back the funds that were processed as a takeback.
athenahealth will work to reconcile the Rebate Check and other associated remittance records once the Rebate Check notification is received from the payer.
athenaOne puts Readjudication Notice records into PEND status for 120 days. If athenaOne does not match the record to a Provider Takeback record within the PEND period, athenaOne automatically assigns the Readjudication Notice record to the athenahealth Follow-Up team. The Follow-Up team reviews the record and contacts the payer as needed to determine the status of the recoupment. The Readjudication Notice record is set to OPEN status in PRACTICE responsibility under the following circumstances:
- The Follow-Up team confirms that your practice needs to send a refund to the payer.
- The record is determined to be for a non-athenaOne claim.
- The payer will not provide any information to the Follow-Up team.
The record is assigned to practice responsibility with an event such as "Refund Required," "Refund Required - Interest Payer," "Readjudication Notice for Non-athena Claim," "Balancing Information Not Available From Payer," "Balancing Information Not Available from Web Portal," or "Calls Not Answered by Payer."
If you are posting the readjudication remittance results in a denial on the affected claims, you are responsible for working those denials as per the normal HOLD/MGRHOLD claim workflows.
A Readjudication Notice record represents a notification from the payer indicating a new adjudication to a previously processed claim that results in a change in the level of reimbursement. The change in payment is made non-financial in the batch by reporting a batch exception that fully offsets the change in claim-level reimbursement. Readjudication Notice remittance records function as placeholders for money due to the payer (accounts receivable). They are eventually offset by a Provider Takeback remittance record issued by the payer.
A Readjudication Notice occurs at the EOB level because it allows the payer to return the new adjudication on the claim without performing the financial takeback. athenaOne posts the new adjudication to the claim and creates the Readjudication Notice record as a placeholder for the eventual offset of funds.
Note: athenahealth posts the informational takeback when we receive the Readjudication Notice because this is the only time that the payer sends the posting level detail.
athenaOne treats Readjudication Notice remittance records from Medicare the same as from other payers with one special exception: Medicare does not send individual Provider Takeback records that can be directly linked to Readjudication Notices for claim overpayments that are less than $10. Instead, Medicare sends a bulk Provider Takeback for multiple claims. In order for athenaOne to reconcile these readjudication records, we need to receive the refund request letter from Medicare that details the claims that were included in the bulk Provider Takeback.
After a Readjudication Notice is received from Medicare, athenahealth should also receive a refund request letter from Medicare if your practice's pay-to address is set up as an athenahealth P.O. box. If we receive the letter, we extract the data from it, manually enter it into athenaOne, and match it to the Readjudication Notice records. However, if we do not receive the letter, you are responsible for working any remittance records related to the letter if multiple overpayments of less than $10 are referenced.
If the Readjudication Notice record is less than $10, you will need to reference the refund request letter to locate the provider takeback.
When we receive a refund request letter, athenaOne creates a Refund Request Letter remittance record, and we add all the identifying numbers to the record for possible matching. If athenaOne is able to match the individual refund requests on the letter to Readjudication Notice records, athenaOne kicks the associated ATHENA claims with REFUND. If all the individual refund requests on the letter are able to be matched to ATHENA claims, athenaOne automatically closes the refund request letter so that the claims are worked from only the MGRHOLD bucket.
Your practice reviews the letter and the matched Readjudication Notice records, which include links to the associated claims. Your practice requests an offset from Medicare on a future remittance or processes a refund payment to Medicare. Since the claim is already readjudicated, the refund adjustment is unnecessary on the claim level.
When we receive a provider takeback remittance record, athenaOne matches it with a previously created Readjudication Notice and a refund request letter, and it automatically closes all three records.
If the provider takeback matches to a refund request letter that indicates the takeback is for an incorrectly paid HPSA incentive payment, athenaOne automatically changes the provider takeback to an incentive payment, and it sets its program to Medicare Special Incentive (HPSA, HSIP, PCIP).
Note: If the provider takeback remittance record is for multiple claims (i.e., it is a bulk provider takeback), athenaOne will need the refund request letter to reconcile. If we do not receive the refund request letter for a bulk takeback, you are responsible for working the records.
- athenahealth receives the original payment and post it against the charges on the claim.
- When athenahealth receives a charge reversal/readjudication, we post a takeback of the original payment, and we reverse all previously posted transfers and adjustments. Then we post the new adjudication and create a Readjudication Notice record to offset the claim-level takeback amount. We also add a link in the claim note to the Readjudication Notice.
- If a refund request letter arrives, athenahealth creates a Refund Request Letter remittance record. athenaOne automatically attempts to match the individual refund requests to the relevant claims via the Readjudication Notice records. When this letter arrives, you should immediately initiate an offset request or refund payment to Medicare. If Medicare does not receive your offset request or refund payment in the number of days stated on this letter, they will issue a provider takeback remittance record and interest may accrue.
- If Medicare issues a provider takeback, athenahealth creates a Provider Takeback remittance record for the takeback amount. athenaOne automatically searches the system for the matching Refund Request Letter and any related Readjudication Notice records, automatically links the provider takeback to the related claims, and closes all related remittance records. This completes the series of transactions related to the readjudication.
Note: athenaOne identifies related remittance records by the record amount and the payer's Internal Control Number (ICN/PCN), a unique numerical identifier that Medicare and other commercial payers use to track transactions in their systems. The ICN/PCN connects the provider takeback to the refund request letter and the Readjudication Notice. - If Medicare has collected interest as a result of the takeback, athenahealth creates a separate Interest Payment remittance record for the interest amount (see Interest remittance record type for more information).
Note: athenaOne does not allow posting of negative interest (interest related to a recoupment) at the claim level; you must create a remittance record for this situation.
Your responsibility
- If athenaOne cannot automatically close a provider takeback remittance record and athenahealth cannot identify its matching records, athenaOne forwards the remittance record to our follow-up team to request identifying information from the payer. If the payer does not provide identifying information, we will forward it to you for your review. If you identify the record, you return it to us for processing.
- You are responsible for requesting an offset from the payer or refunding the overpayment if the payer cannot issue an offset (provider takeback remittance record).
- You are responsible for working any holds on the claim from posting the readjudication remittance.
A Readjudication Notice is generated when the readjudication payment is less than the original payment that the payer is reversing.
For example, assume the following scenario (denial readjudication by Medicare):
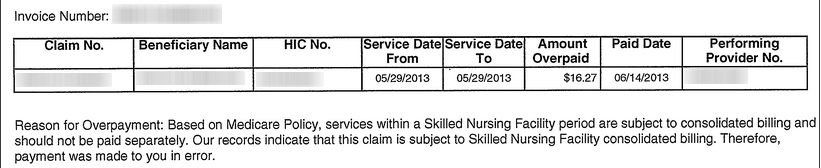
Medicare has reversed their original adjudication of $16.27 payment and denied the claim as covered by another payer.
First Remittance
Reversal of original adjudication
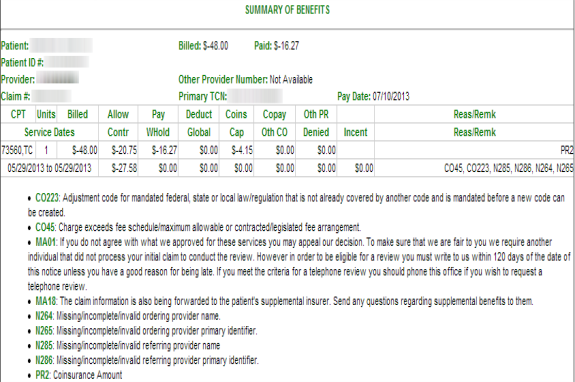
New adjudication
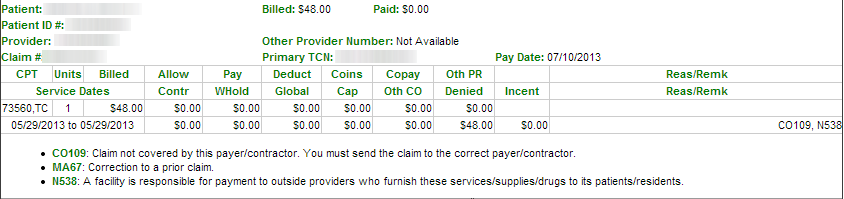
The payer, however, has not recouped the $16.27 overpayment in this remittance/check. They have sent a provider-level adjustment to offset the claim-level takeback.
Provider-Level Adjustment and claim payment summary
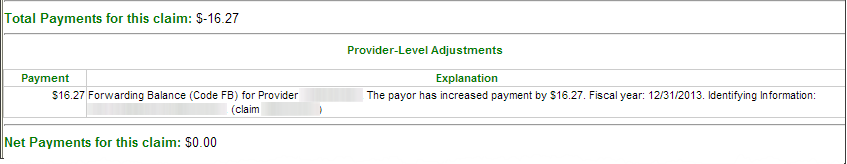
In this first remittance, Medicare reversed its original adjudication and denied the claim. The information on the provider-level record provides useful information for identifying the claim it is related to.
Our process for posting this remittance
- athenaOne posts the $16.27 takeback to the claim, voids the original transfers and adjustments, and applies the readjudication kicks, placing the claim in Hold status for "Bill another carrier/Carveout."
- athenaOne discards the provider-level record into a Readjudication Notice remittance record for $16.27 and links it to the claim. We pend the Readjudication Notice record for 120 days to await the future offset (provider takeback) from the payer.
- A summary of the readjudication recoupment process appears in the middle of the Claim Edit page, just above the "Charges" section, under Remittance Records.
Refund Request Letter (Medicare only)
Medicare issues a Refund Request Letter (RRL) around the same time they issue the Readjudication Notice. The RRL contains information about the individual claim overpayment requests that athenaOne may need to locate matching Readjudication Notice and Provider Takeback remittance records.
Note: Due to the delay in sending and processing paper through the mail, the Refund Request Letter is almost always received after we have posted the readjudication remittance.
Our process for posting this remittance
- athenahealth data enters the pertinent information from the letter.
- athenaOne creates a Refund Request Letter remittance record for each "Invoice Number" on the letter.
A summary of all overpayment requests for each "Invoice Number" is shown in the "Refund Requests" section of the remittance record.- athenaOne attempts to auto-match each overpayment request to a Readjudication Notice remittance record.
If a matching Readjudication Notice record is found, athenaOne kicks the associated claims with the legacy kick code "REFUND" or with one of these kick codes: "SENDREFUND" or "SENDREFUNDREQUEST"; all these kick codes place the claim in MRGHOLD.
- SENDREFUND indicates that the payer will not take back the amount, so a refund should be issued.
- SENDREFUNDREQUEST indicates that interest will be charged if the amount requested is not refunded in a timely manner.
- athenaOne automatically closes the Refund Request Letter remittance record when all overpayment requests have been matched to an athena claim.
athenahealth sends the Refund Request Letter remittance record to the practice with the event "Refund Request Letter for non-athena claim" if any of the overpayment requests are found to be for a non-athena claim.
Second Remittance
On a future remittance, Medicare sends a provider-level adjustment to recoup (offset) the Readjudication Notice and assesses interest on the overpayment.
Provider-level adjustment
"Overpayment recovery (CodeWO) for Provider [nnn]. The payer has reduced payment by $16.41. Fiscal Year 12/31/2013. Identifying information: [nnnn]."
Our process for posting this remittance
- athenaOne discards the $16.41 provider-level adjustment into a Provider Takeback remittance record.
- athenaOne finds the matching Readjudication Notice and Refund Request Letter remittance records, displays this under Possible Matching Records and:
- Matches the remittance records to each other, determines that $0.14 is the amount of Interest assessed, and shifts $0.14 out of the Provider Takeback record into a new Interest remittance record.
- Closes the Readjudication Notice and Provider Takeback remittance records, leaving claim notes that reference each other.
- athenaOne leaves a claim note, if associated with an athena claim, indicating that the readjudication process is complete:
"The readjudication process by [payer] has been completed. Please see records [nnn] RN, [nnn] (PT, and [nnn], (INT)."- athenaOne updates the "readjudication records summary" on the Claim Edit page to reflect recoupment of the overpayment.
Note: athenaOne does most of this matching and reconciling automatically via intelligent rules configured for each payer. However, there are times when athenaOne is unable to do this automatically, such as when the payer does not return useful identifying information, or if there is not yet a rule to automate the steps. In this case, athenaOne displays the Possible Matching Records table on the Remittance Record page to help locate records that might match but were unable to be automated.
Do not change a Readjudication Notice record to any other remittance record type. Changing a Readjudication Notice record to another record type removes the record from the normal athenaOne workflow; this record type includes events that move the record appropriately through the workflow.
When reconciling offsetting remittance records, leave a note in each record referencing all record IDs included.
- Display the Remittance Record page: Follow your remittance record resolution workflow, for example, via the Unpostables Worklist or the Manage Remittance page.
- Locate the Provider Takeback remittance records that fully or partially offset the Readjudication Notice.
- If you find a matching record in the Possible Matching Records table, select the record and click Submit. athenaOne closes both records with a note referencing the match.
- If no matching records are found in the Possible Matching Records table, but the practice locates a matching takeback record, manually reference and close each record.
Matching records found
- Under Update status and reassign record, select the event on the record that best describes the current situation, to apply with your update.
For example, if the matching record is a Provider Takeback and it fully offsets the matching Readjudication Notice, select event "Resolved Provider Takeback — Balancing Record Identified," which will close the record. - Enter a note describing why you are making the update, and make a note of the IDs of any matching records.
- Click Save to record your actions.
No matching records found
- Review the record for a possible refund. If you choose to refund the payer for this amount, post the refund to the claim; follow-up automation reverses the informational "takeback" previously posted, zeroing out and closing the Readjudication Notice.
- If you decide to wait for recoupment, choose the event on the record to apply with your update that best describes the current situation.
For example, if the balancing record has not yet been returned by the payer, select the event "Balance Record Not Yet Received."
If you have additional information, use the event "Additional information provider." - Enter a note describing why you are making the update, and make a note of the IDs of any matching records.
- Click Submit to record your actions.