MIPS Dashboard
To help maximize your MIPS incentive payments, quality managers and providers can access this page to check clinician eligibility and enrollment, and to track measure-level performance at the individual or group level.
The MIPS Dashboard is also where you notify athenahealth if you are approved for a MIPS exception or to take advantage of an automatically applied exception. See the How to Guide: MIPS Exceptions for additional information.
On the Main Menu, click Quality. Then click MIPS Dashboard.
-
Use the eCQM Data page to preview your organization's quality data for the current year, as calculated from quality results for your athenaOne data and from imported QRDA I files. You can then export your quality report results in both QRDA I and QRDA III report formats.
-
Use the Program Attestations page to complete manual attestations and sign offs for Promoting Interoperability (PI) measures and Improvement Activities (IA) measures within both MIPS and MVP programs.
To access this page, your practice must have at least one MIPS eligible clinician (EC).
To track and submit MIPS measure performance as a group, open a support case to request that the MIPS group reporting option be enabled for your practice.
Note: Your practice must have at least two MIPS-eligible clinicians.
- On the Main
Menu, click Support > Success Community > Contact Client Support Center to enter your quality management case.
- Include the following information in your case.
- TIN
- Set of measures
- Request group reporting or both group and individual reporting
- Click Create Online Case.
A case confirmation page appears with the case number.
athenahealth automatically enrolls eligible clinicians in MIPS on your behalf (see Eligible clinicians (ECs) for MIPS). You can create a support case to unenroll a provider.
Note: Any eligible clinician that you unenrolled for the MIPS program appears on the dashboard as Not enrolled.
Eligibility is updated the first Saturday of the month.
To check the eligibility, enrollment, and composite performance score (CPS) of providers in your practice:
- Display the MIPS Dashboard: On the Main
Menu, click Quality. Then click MIPS Dashboard.
Providers are listed from lowest scores to highest scores.
Note: If you are an eligible provider, your own information appears at the top of the list. - Review the list of MIPS-eligible clinicians.
Note: MIPS data is submitted for each TIN/NPI combination. Providers who practice under multiple tax IDs have more than one row and more than one set of data. - Check the MIPS eligibility of each clinician in the Eligibility column.
Note: The eligibility status shown on the MIPS Dashboard is determined based on an interface (API) with the CMS Quality Payment Program (QPP) website. If the eligibility status includes the alert icon , click the icon to display information about any mismatch between the QPP and athenaOne data.
, click the icon to display information about any mismatch between the QPP and athenaOne data. - Check the enrollment status of each clinician in the Status column.
- To view measure-level details for a specific provider, click the provider's row (see To view a Provider Report Card and sign off on data).
- If an eligible clinician is shown as not enrolled, you can use the Program Enrollment page to enroll the clinician.
Enrolled providers can sign off on their data after the reporting period is over. If you have a National Provider Identifier (NPI) number and are eligible for athenaOne to submit MIPS CQMs on your behalf, you must sign off on your measures before we can submit them to CMS. Only usernames associated with the NPI can sign off on provider measures.
Note: The designated point person in your organization can sign off on group submissions.
- Display the MIPS Dashboard: On the Main Menu, click Quality. Then click MIPS Dashboard.
- Click a provider row.
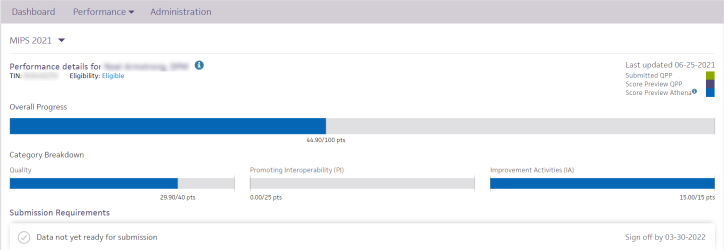
The report card includes an overall progress bar, category breakdown, submission requirements, and objective status.
Note: MIPS data is submitted for each TIN/NPI combination. Providers who practice under multiple tax IDs have more than one row and more than one set of data. - Review performance data and any remaining MIPS objectives.
Note: You can sort data in the Objective Status section by clicking the arrows next to a column name. - If an alert appears, the provider must sign off on MIPS data before athenahealth can submit the data to CMS.
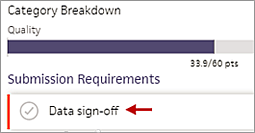
Note: Sign-off is required for the electronic submission of MIPS CQMs. For MIPS PI and IA measure data, sign-off is required only if you requested that athenahealth change the submission method for PI and IA measure data to the Registry method (see athenahealth is a qualified registry). - Click Data sign-off.
- Enter your first and last name and then click Sign off.
Per the requirements of the MIPS program, the MIPS Dashboard tracks measure data for each eligible clinician and tax identification number (TIN) combination (that is, at the TIN/NPI level).
Note: Providers who practice under multiple tax IDs have more than one row in the Practice Performance view and more than one set of data.
To review or compare the measure-level performance of providers in your practice:
- Display the MIPS Dashboard: On the Main Menu, click Quality. Then click MIPS Dashboard.
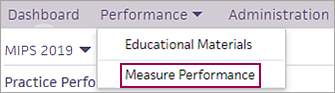
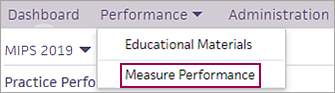
- Click the Performance menu and select Measure Performance.
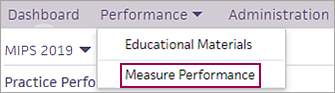
- Review or compare the measure-level performance of providers in your practice. You can review the following information for each provider or TIN:
- Measure — Measure name as it appears on the Quality tab of the patient chart.
- Category — Relevant MIPS category name.
- Num/Den — Numerator and denominator (for numeric measures).
- Satisfied — Non-benchmarked measure performance, calculated as numerator/denominator, less excluded patients.
- athenaOne Average — Average performance for this measure of all participating providers across athenaOne. This column allows you to see how you're performing on the measure compared to other clinicians in our network.
Note: For an athenaOne performance average to appear for a measure, at least 20 individuals or groups must be enrolled in the measure, and each individual or group must have at least 20 patients in the denominator. If the minimum threshold for enrollments (20) or the minimum number of patients in the denominator (20) is not met, the message "Insufficient Data" appears in the athenaOne Average column. - Points — Number of points achieved for each measure, as received from CMS.
- To sort data in the Measure Performance view by any column, click the arrows next to the column name.
- Sort by Measure to compare performance, by measure, across providers.
- Sort by Category to review measures by category (for example, all Improvement Activity (IA) measures), across your practice.
- Sort by Satisfied to identify the highest and lowest performing measures, by provider, across your practice.
- Click the arrow next to the column name again to display the list in ascending or descending order.
You can filter data in the Measure Performance view by provider, TIN, and category.
- Display the MIPS Dashboard: On the Main Menu, click Quality. Then click MIPS Dashboard.
- Click the Performance menu and select Measure Performance.
- To filter data by provider or TIN, click
 Select next to Filter on the left side of the page.
Select next to Filter on the left side of the page.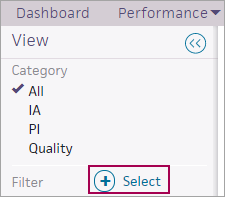
The Filter window opens. - Click Provider or TIN on the left side of the Filter window, and then select the filter options on the right side of the window (for example, provider names).
- Click Apply to view the filtered measure data.
- To filter data by a category, select an option in the Category filter on the left side of the Measure Performance view.
![]() For a demonstration, see this video: MIPS 2020 quality data reporting exemption.
For a demonstration, see this video: MIPS 2020 quality data reporting exemption.
If a MIPS-eligible clinician has experienced extreme and uncontrollable circumstances that affect the MIPS Quality, Cost, Improvement Activities, or Promoting Interoperability performance categories, the clinician can submit an application to CMS for re-weighting of any or all MIPS performance categories. An exception allows an eligible clinician's performance categories to be re-weighted to 0% and flags the clinician as exempt from the requirement to submit MIPS 2021 reporting data for the exempted categories.
Note: For more information about the Extreme and Uncontrollable Circumstances Application, see Quality Payment Program — COVID-19 Response from CMS. For information about how to apply for an exception, see About QPP Exceptions on the QPP website.
If you submitted an application to CMS and received an approved exception, you should record your exception status on the MIPS Dashboard to prevent the submission of data for the exempted quality performance categories (Quality, Improvement Activities (IA), or Promoting Interoperability (PI)).
Important: The deadline to notify athenahealth of your exception status for any performance categories is January 14, 2022. MIPS submissions for providers and groups begin after January 14, 2022. After January 14, the option to record a MIPS exception status will be disabled.
- Display the MIPS Dashboard: On the Main Menu, click Quality. Then click MIPS Dashboard.
- Click Administration at the top of the page to display the Administration view.
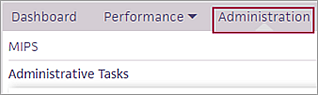
- Click Update Exception Status.
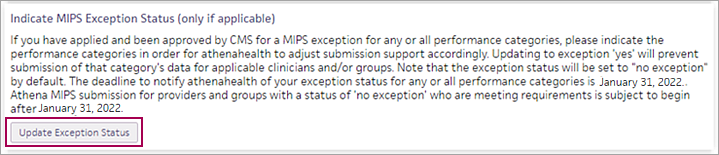
The Indicate MIPS Exception status (only if applicable) page appears. You can record a MIPS exception for an individual provider or for all providers. - To record an exception status for an individual provider:
- Click edit next to the provider's name in the list.
The Edit Exception view appears. - Exception Status — Click the menu and select the exceptions you obtained from CMS.
- Quality, PI and IA exception obtained
- Quality and PI reporting exception obtained
- Quality and IA reporting exception obtained
- IA and PI reporting exception obtained
- Quality reporting exception obtained
- PI reporting exception obtained
- IA reporting exception obtained
- Click Save.
The exception statuses now appear in the Exceptions table.
- Click edit next to the provider's name in the list.
- To record exception statuses for multiple providers:
- Click Batch edit above the list of providers.
The Add Exception view appears. - Providers/TINs — Select provider TINs from the list or click Select all.
- Exception Status — Click the menu and select the exceptions you obtained from CMS.
- Quality, PI and IA exception obtained
- Quality and PI reporting exception obtained
- Quality and IA reporting exception obtained
- IA and PI reporting exception obtained
- Quality reporting exception obtained
- PI reporting exception obtained
- IA reporting exception obtained
- Click Save.
A prompt appears for you to confirm the updates. - Click OK.
The exception statuses now appear in the Exceptions table.
- Click Batch edit above the list of providers.
- Click Return to the MIPS Dashboard.
The Merit-based Incentive Payment System (MIPS) was introduced in 2017 and is a track under the Quality Payment Program (QPP). MIPS focuses on these categories of work: Quality, Promoting Interoperability (PI), Improvement Activities (IA), and Cost. For more information, see About the Merit-Based Incentive Payment System (MIPS) on the Success Community.
Note: Cost data does not appear on the MIPS Dashboard. For information about the Cost category, see Overview: MIPS Cost Category Measures on the Success Community.
MIPS allows clinicians to choose the activities and measures that are most meaningful to their practice to demonstrate performance. Eligible clinicians can meet the six-measure Quality category reporting requirement through any combination of eCQMs or MIPS CQMs (formerly known as Registry measures).
athenahealth may identify providers and TINs that could improve their performance in the MIPS Quality category by enrolling in additional quality measures (athenahealth will not unenroll providers or TINs from any existing measures). Based on our analysis, athenahealth may automatically enroll some providers/TINs in additional quality measures. You can find the list of providers/TINs and the additional measures we are enrolling them in on the Practice Files page.
Note: If providers/TINs are enrolled in more than six quality measures, CMS selects the top performing measures submitted.
Under MIPS, clinicians can report individually or as a group. athenahealth reviews both sets of data to see which set has the better performance, after which we report data to CMS on your behalf.
Note: You must use athenaOne and the MIPS Dashboard for at least 90 days before the end of a reporting period in order for athenaOne to record and then submit your data.
athenahealth is a qualified registry for the MIPS program (a qualified registry collects MIPS data from MIPS eligible clinicians and submits the data to CMS on their behalf). As a qualified registry, athenahealth offers two submission methods for organizations that attest for the MIPS PI and IA categories: EHR and Registry submission methods.
By default, athenahealth submits MIPS PI and IA measure data for eligible clinicians and groups via the EHR method, but you can request that we submit PI and IA measure data via the Registry method instead (we always submit MIPS CQMs via the Registry method). The Registry submission method requires you to review the performance data and sign off on that data electronically before athenahealth can submit your MIPS PI and IA measure data.
Important: There is no benefit to switching to the Registry submission method.
To request a switch to the Registry submission method for your MIPS PI and IA category data, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center. After athenahealth completes the switch on your behalf, you'll need to complete the electronic sign-off from the Provider Report Card of the MIPS dashboard when the data becomes available (see To view a Provider Report Card and sign off on data).
By default, individual clinicians and groups are enrolled in the year-long MIPS Promoting Interoperability (PI) program for submission, but you can instead submit data for any quarter of the year (90 consecutive days). You can see performance and submission support for these quarterly MIPS PI programs on the Quality Management Reporting (QMR) and MIPS Dashboard pages.
Quarterly reporting for MIPS captures PI performance for 90 consecutive days of 2021 to support your success in the Public Health Registries (PHR) objective.
Note: If you already performed any attestations for this reporting year — for example, the Security Risk Analysis (SRA) or the Information Blocking attestation — these attestations are carried over automatically when you move from the default one-year program to a quarterly program.
To request a 90-day program for a specified quarter, submit a case as follows.
- On the Main
Menu, click Support > Success Community > Contact Client Support Center.
The case classification page appears. - Click the Quality Management category.
The Quality Management subcategories appear. - Click Quality Program Enrollment and then click Create Online Case.
The case creation page appears. - Enter the required information (for example, the clinicians or groups to enroll in the quarterly MIPS PI program and the quarter for the submission).
Note: If you prefer a custom 90-day date range that is not based on quarter, request the MIPS PI Not for Attestation Program (no submission support). - Click Create Online Case.
A case confirmation page appears with the case number.
Custom 90-day MIPS PI programs not based on a quarter
If you prefer a custom 90-day date range that is not based on a calendar quarter, request the MIPS PI Not for Attestation Program (no submission support). Your performance in this custom program will be available on the Quality Management Reporting page, but not on the MIPS Dashboard page. You are responsible for submission of the data to CMS.
Note: If you already performed any attestations for this reporting year — for example, the Security Risk Analysis (SRA) or the Information Blocking attestation — these attestations are not carried over and you will need to reattest.
If providers in your practice are billing Medicare in athenaOne and are eligible provider types as defined by CMS, we automatically enroll them in MIPS measures in athenaClinicals. Eligible clinicians are assigned a composite score based on their performance across all four threads of work (see MIPS Scoring). This score ultimately serves as a modifier on their Medicare Part B reimbursements.
Note: MIPS scores apply only to Medicare Part B.
athenaOne runs a script daily to enroll individual providers in MIPS. This script uses the CMS Quality Payment Program (QPP) status to retrieve eligibility. Individual providers with an "Eligible Individual Clinician" status are automatically enrolled in MIPS.
Note: This script works on individual providers only. To enroll a group in the MIPS program, see To track and submit measure performance as a group.
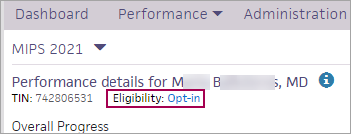
MIPS eligibility information for each clinician and TIN appears in these views of the MIPS Dashboard:
- Practice Performance view — Eligibility column
- Provider Report Card view — Eligibility field at the top of the report card
The eligibility status shown on the MIPS Dashboard is determined based on an interface (API) with the CMS Quality Payment Program (QPP) website. In some cases, athenaOne cannot match provider data with QPP — for example, an NPI may not be recognized as a valid NPI, or we may be unable to match the medical group in QPP with a TIN address in athenaOne. In cases where the eligibility status needs attention, click the alert icon ![]() to display information about any mismatch between QPP and athenaOne data and how to address the issue.
to display information about any mismatch between QPP and athenaOne data and how to address the issue.
Note: The QPP site is the ultimate source of truth about provider MIPS eligibility. If you notice an issue in athenaOne, open a support case so that we can investigate an incorrect match or status (see To view MIPS eligibility, enrollment, and practice performance).
Providers not required to participate in MIPS include:
- Eligible clinicians newly enrolled in Medicare for the reporting year.
- Providers participating in an Advanced APM who are meeting the required thresholds.
- Providers with less than $90,000 in Medicare Part B charges.
- Providers who care for fewer than 200 Medicare Part B patients.
Note: If a provider is not required to participate in MIPS, you can still enroll the provider to gain experience in the program (request that the provider be enrolled in the MIPS Quality "Not for Attestation" program).
To unenroll from the MIPS program, please submit a support case from athenaOne > Support > Success Community > Contact Client Support Center and indicate one of these reasons for unenrolling in the program:
- You are a participating provider in an Advanced APM and you are meeting the required thresholds.
- You care for fewer than 200 Medicare patients.
- The current year is the first year that you're participating in Medicare.
To confirm your status in any of these categories, please contact CMS (CMS makes the final determination).
Note: If you previously requested that a specific provider be unenrolled from the MIPS program, we will not re-enroll that provider, even if their eligibility status with QPP has changed.
If a provider is enrolled in MIPS but does not yet have a full year of eCQM data, a prompt on the MIPS Dashboard encourages the provider to import eCQM data from another EHR.

For MIPS Quality Program category submission, CMS advises using the EHR that meets data completeness requirements for at least 70% of the reporting year.
If you determine that your eCQM data in athenaOne will not meet the data completeness threshold and you would like athenahealth to submit a full year of MIPS Quality data, you must aggregate your non-athenaOne eCQM quality data using the QRDA I import process (see To import QRDA I files).
Note: athenahealth does not support data aggregation for MIPS CQMs (formerly known as Registry measures) in athenaOne.
If you do not want athenahealth to submit your MIPS Quality Program data but would still like to use the Quality Management Reporting page to monitor your performance in athenaOne:
- Create a support case (from athenaOne > Support > Success Community > Contact Client Support Center).
- Request that you be unenrolled from the MIPS Quality program and instead be enrolled in the MIPS Quality "Not for Attestation" program.
You can then aggregate your athenaOne quality data with non-athenaOne data outside athenaOne for submission on your own.
To help maximize your MIPS incentive payments, quality managers and providers can access the MIPS Dashboard, where you can:
- Check clinician eligibility and enrollment.
- Track and submit measure performance individually or as a group (if you have two or more MIPS-eligible clinicians).
Note: CMS will accept both individual and group submissions, and then take the best score of those submissions for each provider. - View your CMS preview scores for these categories: Quality, Promoting Interoperability (PI), and Improvement Activities (IA). The preview scores are calculated by CMS based on your enrollment in athenaOne.
Note: Cost category data does not appear on the MIPS Dashboard. For information about the Cost category, see Overview: MIPS Cost Category Measures on the Success Community. - View Provider Report Cards.
- Record an approved exception to one or more MIPS quality performance categories to prevent the submission of data for the exempted performance categories.
- Identify opportunities to improve performance.
Note: Custom MIPS programs and MIPS programs that are labeled as "Not for Attestation" do not appear on the MIPS Dashboard. To track the performance of providers enrolled in these MIPS programs, use the Quality Management Reporting page.
The MIPS Dashboard includes these views:
- Practice Performance — List of eligible providers and medical groups that shows enrollment and MIPS composite performance scores.
- Provider Report Card — Overall progress and measure-level performance, as well as any submission requirements, for the selected provider or medical group.
- Measure Performance — Measure-level performance for all providers and medical groups.
- Educational Materials — Core and nuanced aspects of MIPS.
- Administration — Update Security Risk Analysis status, attest to the prevention of information blocking, attest manually for the HIE Bi-Directional Exchange measure, attest for the SAFER Guides measure, or record an approved exception for one or more performance categories.
When you display the MIPS Dashboard, you see the Practice Performance view.
Tip: From other views of the dashboard, click Dashboard at the top left of the page to return to the Practice Performance view.
You can use the Practice Performance view to:
- Review a list of MIPS-eligible clinicians at your practice. Providers are listed from lowest scores to highest scores.
Note: If you are an eligible provider, your own information appears at the top of the list. - Confirm that your eligible clinicians are correctly enrolled in the program to help ensure you avoid penalties. We require eligible clinicians to be enrolled in our programs and meet submission requirements in order to submit your data to CMS.
-
Click on an individual eligible clinician's name to see their performance.
-
Review prior year’s performance.
- View the composite performance score (CPS) of all enrolled providers.
Note: The CPS on the Practice Performance view reflects the athenahealth official Submitted data score, not the CMS anticipated Score preview data. - Access Provider Report Cards.
Note: Providers who practice under multiple tax IDs have more than one row and more than one set of data because MIPS data is submitted for each TIN/NPI combination.
This page includes clinicians who are an eligible provider type based on the CMS definition of eligible clinician and who has billed at least one Medicare part B claim in athenaOne in the last 365 days. Clinicians who are enrolled in MIPS in athenaOne but do not meet these conditions still appear in the Measure Performance view but not in the Practice Performance view. If an eligible provider is not showing up on the dashboard, submit a case to request enrollment.
To access a Provider Report Card, click a provider row on the Practice Performance view of the MIPS Dashboard.
The Provider Report Card is a provider-centric view that lets providers and practice managers:
- Review performance data (composite performance scores and measure performance). This performance data helps providers and practice managers understand how their measure performance will translate into overall success in the MIPS program. This helps you identify specific measures or eligible clinicians to focus on to maximize performance. Use this view in tandem with the patient-level data available in the Quality Management Report (QMR) to gain a detailed understanding of measure performance.
- See any remaining MIPS objectives.
- See whether public health registry (PHR) measures are satisfied or not satisfied.
- See whether these Promoting Interoperability category requirements are satisfied or not satisfied: Security Risk Analysis (SRA), Prevention of Information Blocking attestation, and SAFER Guides measure attestation.
-
Tracking the overall progress you are making on your total score.
- Complete submission: See Submission status.
If sign-off is required, the provider report card displays an alert and a space for the provider to electronically sign. Only usernames associated with the provider NPI can sign off on provider measures.
athenaOne displays category scores received from CMS for these categories:
- Quality
- Promoting Interoperability (PI)
- Improvement Activities (IA)
Your MIPS preview scores are updated daily, typically by noon Eastern time.
The Provider Report Card CPS and category scores reflect the athenahealth official Submitted data score (when it exists) and the CMS anticipated Score preview for data not submitted by athenahealth.
- Green bars represent the CMS-returned score associated with data officially submitted on your behalf by athenahealth. These final scores consider all data submitted by athenahealth on your behalf.
- Purple bars represent the CMS-returned anticipated score for data in athenaOne.
- Blue bars represent the athenaOne score preview that appears during the reporting year, before CMS returns its official score preview in the fall of the reporting year (see Score Preview Athena).
The athenaOne Average score will display for all measures on the MIPS Dashboard. This shows the average performance of all participating providers across athenaOne on these measures. It allows you to compare how you are performing to other clinicians on our network who are tracking the same measures. See the section highlighted in yellow below.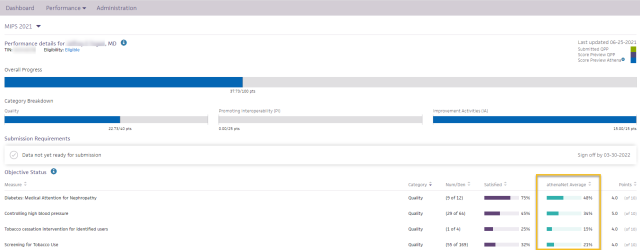
All measure-level scoring details come directly from CMS.
You can sort the data in the Objective Status section by clicking any column title.
Before CMS publishes its official score preview in the fall of the current reporting year, an internal score — Score Preview Athena — is shown on the Provider Report Card view of the MIPS Dashboard in blue. The internal algorithm that generates the athenaOne score preview is a close approximation of the CMS scoring logic and includes these categories:
- Quality
- Promoting Interoperability (PI)
- Improvement Activities (IA)
These scores provide an approximation of your performance on MIPS measures throughout the year prior to the official score preview that is released by CMS later in the calendar year.
Note: Small practice bonus, Improvement Scoring, and Cost Category performance are not included in the internal scoring algorithm; therefore, you may see discrepancies between the scores from CMS and the score preview from athenahealth.
The category scores — shown as a fraction under each progress bar in the Category Breakdown section — reflect the weighted scores for each category. As a result, you may see different category values for each year, but your overall scores remain the same.
Your MIPS final, category and measure scores may be be impacted by actions or inactions by the user including:
-
Sign-off status
-
If sign-off is not completed for CQMs, the Quality score will only reflect eCQM performance.
-
If sign-off is not completed for SRA, Complete Actions to Limit or Restrict Interoperability of CEHRT Attestation and SAFER Guides, your PI score will be 0.
-
-
EUC Exceptions
-
You can apply for an EUC Exceptions or it may be automatic. Learn more about EUCs here
-
If you indicate an exception in the Administration section of athena's MIPS dashboard for one or more categories, your category and composite scores will update based on EUC reweighting (applies to individuals and groups). As a reminder, submitting two or more categories will negate the EUC.
-
Note: You must be enrolled in a category for EUC reweighting to factor into your score apart from Cost for individual clinicians.
-
Greater visibility into your submission status to help clinicians and groups identify actions to enable submission. There are a variety of checks that calculate into the Score Preview athena to indicate whether your MIPS data is ready for submission. The following table describes the various Submission Statuses and the actions if any that may be required in order to proceed with submissions. The submission statuses are: Processing, Pending Action, Submitted, Submission Failed, Requirement unmet.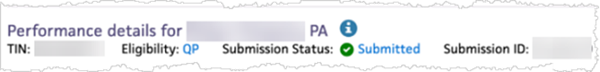
| Eligibility Status | Composite Score Passed | Submission Status | Action |
|---|---|---|---|
| Eligible/Opted-in/QP/MIPS APM/Ineligible | N/A | Pending Action | If enrolled in MIPS PI, SRA, Complete Actions to Limit or Restrict Interoperability of CEHRT Attestation and SAFER Guides attestations are mandatory.
If enrolled in CQM measures, data sign-off is mandatory. To enable submission, please complete signoffs or raise a support ticket on the Success Community |
| Unknown | N/A | Pending Action |
We are unable to match your athenaOne information with the QPP participation data.
Submission is not enabled for Registry / CQM, PI or IA. Submission is enabled for Quality eCQMs. |
| Opt-in and Not opted in the QPP tool | N/A | Pending Action | You need to make an opt-in election on the QPP portal for us to enable submission. |
| Eligible/Opted-in/QP/MIPS APM/Ineligible | Yes | Processing |
Data is being updated and will be processed for submission during the submission time frame.
|
| Error in NPI | No | Submission Failed | Submission was attempted but failed due to TIN/NPI mismatch. Please raise a support ticket on the Success Community with the correct TIN/NPI information. |
The Submission Status field on the Provider Report Card indicates whether athenahealth will submit your data based on the composite score and eligibility status. This field also allows you to review any pending actions required for submission (click Pending Action for more information about the actions you need to take).
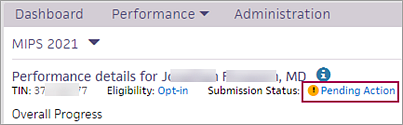
Examples of pending actions include a required SRA sign-off, the information blocking attestation, or data sign-off for CQM measures.
Note: For more information about submission requirements, see the MIPS Submission Guide on the Success Community.
Using the CMS API to connect with QPP, athenahealth retrieves your eligibility status as it relates to submission. If your eligibility check passes and your composite score check passes, athenahealth can submit your MIPS data for you. Your submission status would be Processing.

The submission statuses are: Processing, Pending Action, Submitted, Submission Failed, and Requirements Unmet.
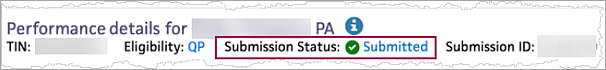
Note: The Submission ID field is the QPP submission ID number generated by CMS when your data was submitted.
The Provider Report Card shows you the tax identification number (TIN) used to submit your data. If a TIN override was applied, the report card indicates that the TIN override rules set up for Medicare on the Payer Enrollment page were used.
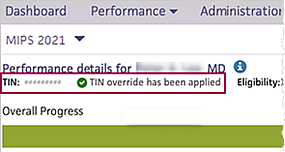
Providers and TINs sometimes bill under different TINs, depending on the payer, provider, and department on a claim (an individual provider may bill under their SSN). A TIN override means that a claim is submitted using a TIN other than the one specified for the medical group on the Medical Groups page (Federal ID field). TIN overrides are set up on the Payer Enrollment page.
The MIPS quality program looks for TIN overrides established when the payer is Medicare. You can set different types of overrides by adding various parameters. For example, you can create an override for TIN X with a Medicare payer override, so that any time a claim originating from TIN X is billed to Medicare, the overriding TIN is used on the claim instead.
Note: If you have any questions about TIN associations with providers attesting for MIPS, contact your Customer Success Manager.
To access the Measure Performance view, click the Performance menu on the MIPS Dashboard and then select Measure Performance.
The MIPS performance data helps providers and practice managers understand how their measure performance translates into overall success in the MIPS program. You can use the Measure Performance view to:
- View a complete list of your eligible clinicians' enrolled measures by MIPS measure category.
- Review and track your practice's measure-level performance.
- Compare your data against the average performance data of all providers in athenaOne who participate in the MIPS measure.
- For each provider, verify whether the security risk analysis (SRA) is satisfied or not satisfied.
- For each provider, verify whether public health registry (PHR) measures are satisfied or not satisfied. If a PHR measure is met by an exclusion, the measure name displays the specific exclusion with a status of "Satisfied." If more than one registry of the same type is included, the measure name is appended with "Multi."
You can sort data by any column title (click the arrow next to the column name). You can also filter data by category, provider, and TIN.
Test patients are patient records created strictly for testing purposes and do not represent a real person's chart. To remain compliant with government regulations for quality programs, make sure that you report and submit data for real patients only.
Note: In accordance with CMS and other quality program sponsors, inactive patients are included in athenahealth certified eCQMs and in quality program submission data on the MIPS Dashboard, the Pay for Performance Dashboard, the eCQM Data page, the Quality Management Reporting page, and in UDS reports.
You can use the Test Patients Identification page to find test patients and mark dummy patients as test patients. Use this page to make sure that test patients are not included in quality reporting when you create test claims, encounters, problems, or diagnoses within the test patient chart.
Note: Patients marked as test patients on the Test Patients Identification page are not included in quality program submission data on the MIPS Dashboard, the Pay for Performance Dashboard, the eCQM Data page, the Quality Management Reporting page, or in UDS reports. (Quality measures appear on the Quality tab of the test patient's chart for testing purposes only.)