 Service Overview — athenaCollector
Service Overview — athenaCollector
athenaCollector is an industry-leading billing and practice management solution — delivering faster payment, increased revenues, and improved control over practice operations.
Tip: You can see your athenaCollector service level at the very top of your screen, on the leftmost tab of the Web browser. You can also pause your cursor over the tab to view your practice name and practice ID number. 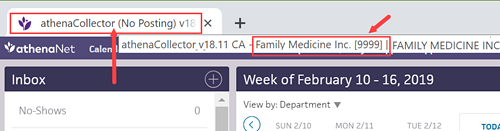
Practices face an array of operational challenges. Constantly changing payer rules make it time-consuming for your staff to keep up. Lost and denied claims significantly affect your practice's income. Lack of accurate data leaves you at a disadvantage during planning and payer negotiations.
athenaCollector helps you solve these challenges. athenahealth offers an industry-leading approach to billing and practice management, combining award-winning software, the nation's largest database of payer rules, and state-of-the-art billing and collection operations.
The result? Significantly improved financial and operational performance for your practice.
With athenaCollector, you can realize immediate and measurable results:
- Get paid more and faster
- Decrease the rate of lost and denied claims
- Benefit from the most up-to-date payer intelligence
- Increase staff productivity
- Delegate the most time-consuming work to us
- Get full visibility into your practice to make better decisions
And you can achieve all of this with a minimal investment. You do not need to buy new server hardware, and there are no upfront licensing fees.
Neither software nor traditional outsourcing services provide everything you need to manage your billing and claims processes effectively and efficiently. athenahealth offers a unique approach that incorporates cloud-based software, extensive industry knowledge, and dedicated, experienced support staff, all integrated into a single service that delivers consistent, dependable results.
With unprecedented visibility into your operations, you can gain greater financial control and realize significant performance improvements.
athenaCollector includes our highly intuitive, cloud-based practice management software that simplifies every step of the process: patient registration, scheduling, check-in, charge entry, referral management, checkout, follow-up, collections, accounting, and reporting.
athenaCollector relieves your staff of many time-consuming activities by:
- Automatically checking patient eligibility prior to appointments and flagging ineligible patients to help reduce denials
- Tracking practice activity in real time, helping to ensure that charges are captured and claims are generated for each patient encounter
- Providing a workflow dashboard that enables you to see the up-to-the-minute status of all claims, revealing which claims have been paid and which claims have not been paid and why
- Maintaining compliance with billing and claims management standards, including HIPAA, EDI, ERA, and NPI
At the heart of athenaCollector is the industry's largest database of payer-specific reimbursement requirements. This proprietary billing "Rules Engine" delivers the in-depth insight and knowledge you need to get paid—and get paid accurately—by health insurers.
Our Rules Engine is updated daily based on athenahealth research and the collective experience of thousands of clients. It tracks the evolving requirements of hundreds of payers and thousands of benefit plans, so you don't have to, and includes everything from coding observations to procedure documentation rules, from situation-specific claim data requirements to insurance identification number formatting protocols. And that's just the beginning.
As data is entered into our practice management application at key points in the patient workflow, our Rules Engine verifies the information and alerts staff when a claim needs to be corrected or when additional data is required on a claim. As a result, our clients are typically reimbursed correctly for their services the first time around.
After you enter charges, our athenahealth service team takes care of much of the rest of the billing process, including:
- Generating and submitting electronic and paper claims
- Confirming receipt of claims and resubmitting lost claims
- Posting remittance advice received from payers, including scanning paper remittance advice into our practice management application for online reference
- Following up on unpaid and denied claims and working to get them paid
- Updating the Rules Engine to help prevent denial recurrences
- Reviewing key performance metrics and notifying you if performance is not consistent with target
Finally, our committed billing and collections experts work in partnership with you to maximize revenue. Our Customer Success Management staff is specially trained to seek opportunities to help you improve your practice's performance.
With athenaCollector, you have the information you need, whenever you need it. It's all available through our cloud-based practice management application, which provides you with up-to-the-minute information posted by your staff and our billing and collections team.
Through our powerful dashboards and reports, you can quickly and easily view key practice performance data: accounts receivable, practice activity, schedule utilization, collections, denials, payer mix, and more. You can analyze individual payers, providers, offices, claims, and patients.
With the ability to see what's happening in your practice—in real time and in detail—you gain an enormous edge in everything from optimizing practice operations to negotiating payer contracts.
And through our unique "Live Benchmarking" capability, you can even see how your practice measures up against other athenaCollector practices in your state or specialty—or even across the nation. Our unique Live Benchmarking gives you insight about which areas of your practice could be improved.