 Service Overview — Population Health
Service Overview — Population Health
athenahealth Population Health
The athenahealth Population Health service is a comprehensive population health management service that helps you achieve your quality goals for value-based reimbursement models while reducing total medical expenses.
The transition to value-based payments is under way, with CMS planning to tie as much as 90% of reimbursement to quality by 2018. Other payers are following suit and introducing their own value-based reimbursement models.
As more and more payers introduce value-based reimbursement models, many healthcare professionals find themselves straddling both the fee-for-service world and the more complex fee-for-value world. Some of the challenges of this new world are:
- How does one define "quality" and measure it in a meaningful, standardized (and reproducible) way?
- How do you keep track of a patient's care outside your office and network?
- How can you influence a patient's behavior to increase the likelihood of disease prevention and early detection? And how can you do this in a systematic way across your organization?
The athenahealth Population Health service is a complete solution that:
- Collects data from disparate EMRs and payers
- Analyzes and stratifies your patient population to:
- Identify and close gaps in care
- Identify patients who may benefit from a care management program
- Predict and lower costs
- Ensure that you meet quality goals
- Provides tools to meet quality measures and achieve care plan goals
- Provides the option to add the athenahealth comprehensive care coordination service to improve care transitions
We have a proven track record of helping some of the nation's most successful Accountable Care Organizations (ACOs) receive ACO MSSP shared savings payments. With our population health services, you can take on risk without the risk.
Effective population health management — achieving quality goals while controlling the cost of care — requires a focused, end-to-end approach to succeed. Still, many health systems are patching together disparate solutions with no guarantee of success. athenahealth manages population health like no other offering by combining cloud-based software, network intelligence, and our expert service teams to address every aspect of the population health cycle.
At the center of your population health success is our network data. We aggregate this data across disparate EMRs and systems through custom-built interfaces and our established relationships with various payers and clinical system vendors. The result? A comprehensive, 360-degree view of your patient population, regardless of location.
We stratify your patient population using continually refreshed clinical and claims data, identifying gaps in care, and using Milliman scoring to rate risk severity (which predicts total claim cost in terms of inpatient services, outpatient services, physician and other services, and prescription drug services). Our services then pinpoint optimal high-yield interventions for patients at risk of developing chronic conditions.
Central to managing your population is the seamless coordination of care. And that's what our care management platform delivers. Care managers get a clear dashboard and workflow that make it easy to create, execute, and track patient care plans. And, when integrated with other athenahealth products, the benefits to patient care are even greater:
- Providers can schedule appointments directly across your network, before the patient leaves the office.
- Clean, closed-loop order management.
- athenahealth experts manage precertification, prior authorization, and referral management.
Our population health services drive results in ways static analytics tools simply can't. Based on your outcomes, we display information directly in the workflow to guide order and referral decisions and help you optimize care and cost. We take on the administrative burden of reporting MSSP measures. And we keep your financial health front and center with our unique partnership model.
The athenahealth Population Health service includes these features:
If a patient has or is at high risk of developing a disease or clinical issue that requires monitoring, you can use the Care Management Workflow to enroll the patient in a care management program. Care management programs help patients and their care teams set goals and take actions to prevent or manage a disease or chronic clinical issue and, in doing so, may improve clinical outcomes and prevent complications and costly medical care.
The Care Manager page provides access to a care manager's schedule as well as care management referral and workflow tools. You can use this page to:
- View and filter all patients associated with care management programs
- Analyze statistics related to these patients
- Manage activities, such as scheduling care management events and changing a patient's status in a care management program
You can also access in-depth clinical data and the care plan on a patient's Person Center.
The Quality Manager provides insight into patient compliance against risk-based contract performance measures. You can:
- Track performance on quality measures
- Identify which measures need attention
- Enter manual results when automated sources are not available
For an in-depth view of each test within a program, you can use the Quality Manager Details page to view and manage patient test results and other information related to quality programs.
The Report List offers an extensive variety of customizable reports. You can sort, filter, and analyze your data across dimensions, including Financial, Membership, Quality, and Pharmacy. These reports help you to:
- Understand costs and total medical expenses
- Reduce out-of-network utilization
- Identify opportunities for utilization reduction
- Support chronic care and disease management
- Identify which patients are at risk for developing a medical issue
athenahealth continues to work on creating a seamless care coordination experience for organizations that use both athenahealth Population Health and athenaClinicals services. The following points of integration between athenaClinicals and athenahealth Population Health address some of the overlap between these products.
If a patient is part of a payer risk contract, such as an accountable care organization (ACO), the patient banner displays a Risk Contract flag in the patient chart and during all stages of the clinical workflow, including scheduling, Intake, and Exam.
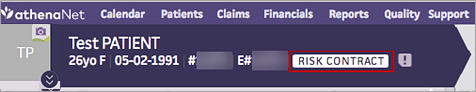
athenaOne retrieves this information from athenahealth Population Health and displays it in athenaClinicals. This information helps alert clinicians when additional care management resources may be available to the patient. The status is updated on a monthly basis to display any risk attribution changes.
The Risk Contract flag appears only for patients who have records in both athenaClinicals and athenahealth Population Health. Your organization must use both athenaClinicals and athenahealth Population Health or an affiliate's practice must use athenahealth Population Health. An EMR feed from athenaClinicals must be implemented in athenahealth Population Health for patients to match across systems.
Note: To use this feature, please contact a member of your athenahealth Population Health Customer Success Management team.
For information about HCC/RAF and patient risk adjustment in athenaClinicals, see
If your organization uses athenaClinicals and athenahealth Population Health, data from both products can be used in athenaClinicals to provide more accurate and timely information about a patient's potential diagnoses and risk adjustment factor (RAF).
- athenaClinicals uses preadjudicated claims data from orders placed during encounters.
- athenahealth Population Health uses three years of historical post-adjudicated claims data provided by payers, including claims from outside the network.
The additional information from athenahealth Population Health can improve the diagnosis and treatment of chronic conditions, reduce manual coordination between ACO administrators and providers, and increase revenue for payment models that are calibrated to the RAF score of the at-risk population.
Because the post-adjudicated claims data from athenahealth Population Health is included, the Patient Risk dashboard in athenaClinicals shows you a more complete accounting of the following:
- Potential and suspected diagnoses
- Risk adjustment factors
- Risk scores
- Gap scores
To benefit from this integration, your organization must use:
- athenaClinicals
- athenahealth Population Health
Note: You can use this integration if your organization is part of an accountable care organization (ACO) that uses athenahealth Population Health. - Data warehouse feed v1.1
The data warehouse feed v1.1 allows athenaOne to match patients in athenaClinicals with patients in athenahealth Population Health and allows preadjudicated claims data from athenaClinicals to flow to athenahealth Population Health.
If you are interested in this integrated functionality, please contact your athenahealth Population Health team to ensure that the appropriate waivers are completed.
If your organization uses both athenahealth Population Health and athenaClinicals, providers can refer patients to a Population Health care management program by creating an order in athenaClinicals. The Population Health care manager can send summary reports of patient care to the referring provider in athenaOne.
You can also bill Medicare for chronic care management services based on referrals from athenaClinicals to care management services in athenahealth Population Health. By sharing information between athenaClinicals and athenahealth Population Health, providers, care managers, and billing staff can coordinate and bill CMS for a patient's chronic care management.
For more information, see Care Management Referrals from athenaClinicals to Population Health.