 User Guide — ATHENAHOLD Status and Claim Submission
User Guide — ATHENAHOLD Status and Claim Submission
ATHENAHOLD is a claim status for claims that require action by athenahealth. When an error or rejection is posted to a claim in athenaOne and the error requires internal review to fix the issue, athenahealth will research and take the necessary corrective action to ensure that the claims are submitted on your behalf.
For assistance with claims in ATHENAHOLD, please create a support case.
The "expected turnaround time" for claims assigned to an ATHENAHOLD status is the time between when a claim is placed in ATHENAHOLD status and when it is resubmitted to the appropriate payer.
The expected turnaround time is effective beginning in the last quarter of 2018.
Most claims that have received a front-end rejection from an insurance payer or clearinghouse are addressed by athenahealth. Rejections can range from ANSI formatting concerns, claims not on file with the payer, and incorrect claim routing.
Error: The Payer or Clearinghouse has rejected the entire billing batch of electronic claims due to formatting issues.
Resolution: Research is completed by athenahealth.
Affected claims are resubmitted to the payer by athenahealth.
Expected turnaround time: Resolved by the end of the third business day.
Error: The claims have been routed to athenahealth to research a harder-to-classify root cause of a front-end rejection from a payer or clearinghouse.
Resolution: After the root cause is identified, the error is corrected and affected claims are then resubmitted by athenahealth.
Expected turnaround time: Resolved by the end of the seventh business day.
Error: After review, the claims are not on file with the payer.
Resolution: athenahealth corrects any errors. Affected claims are then resubmitted by athenahealth.
Expected turnaround time: Resolved by the end of the 10th business day.
Error: A new rule affecting the claim is pending.
Resolution: When the rule is approved and active, affected claims are then resubmitted by athenahealth.
Expected turnaround time: Resolved by the end of the 14th business day.
Error: Due to the complexity of provider credentialing, claims are reviewed manually to ensure that the claim is being sent to the correct payer.
Resolution: athenahealth verifies that the routing is correct for the noted payers, and claims are resubmitted by athenahealth.
Expected turnaround time: Resolved by the end of the 20th business day.
Error: Claims submitted to the secondary payer have errors related to charge/claim balances or the provider primary payment information provided.
Resolution: athenahealth confirms the requirements for the payers involved.
Affected claims are then resubmitted by athenahealth.
Expected turnaround time: Resolved by the end of the 20th business day.
Error: The claims have been rejected due to an incorrect payer ID for the payer or clearinghouse.
Resolution: athenahealth updates the payer ID or receiver.
Affected claims are then resubmitted by athenahealth.
Expected turnaround time: Resolved by the end of the second business day.
Error: The claims have been rejected by the clearinghouse for an unknown reason.
Resolution: athenahealth works with the clearinghouse to determine the root cause of the issue and make necessary updates.
Affected claims are then resubmitted by athenahealth.
Expected turnaround time: Resolved by the end of the seventh business day.
If enrollment for ERA remittance with a payer is near completion, claims for that payer move to ATHENAHOLD status if the estimated completion date of the ERA tasks is fewer days than the turnaround time for claims dropped to paper. A claim note alerts you to the hold.
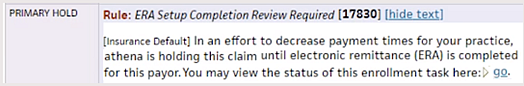
Click go in the claim note to open the associated ERA task. You do not need to complete additional work on the ERA task for these claims. When enrollment is complete, the hold is released and the claims drops to the payer.
Note: If the timely filing deadline approaches and your enrollment is still incomplete, athenahealth submits the claim on paper to ensure payment.
If you want to override the hold for specific ERA tasks, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.