Quick Reference — To perform a custom eligibility check for a patient's insurance policy
Quick Reference — To perform a custom eligibility check for a patient's insurance policy
-
Display the Quickview page for a patient.
-
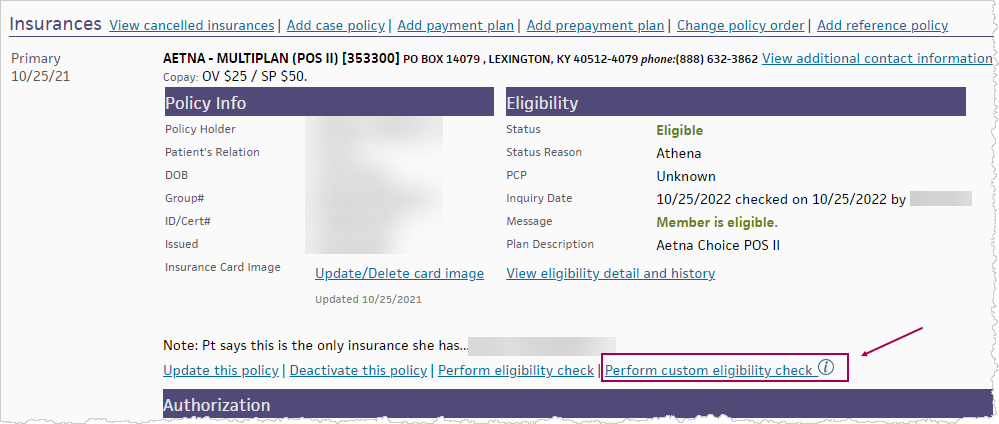
In the Insurances section, for a specific policy, click the Perform custom eligibility check link.
- This link is only available if you're using the enhanced Payer-Provided Eligibility Details page (released in Summer 2023).
- If you were using the enhanced page and then chose Go to: Old eligibility page, this link will not be visible.
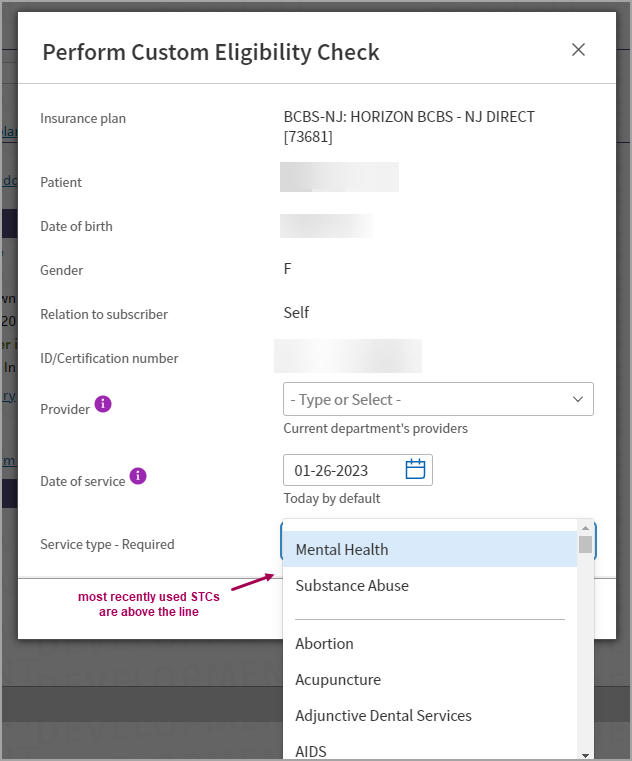
The Perform Custom Eligibility Check window appears.
-
Select the details for the custom eligibility check:
- Provider — (optional) - Select a Provider.
- This list only shows the Providers within the department that you're currently logged into.
- To select a provider from another department, log into that department. If you don't select a provider, the system will choose one based on the patient's previous appointment and claims.
- Date of Service — (Today's date defaults) Select a Date of Service.
- Most payers will accept a prior or future date, but payer rules vary. Some payers may not return benefit details for dates before the current year or in the future.
- Service Type — Select a Service Type Code (STC) from the list. The most recently used STCs appear above the line in the menu.
STCs are industry standard codes that payers and clearinghouses use to specify what eligibility is being requested.
- Provider — (optional) - Select a Provider.
-
Click Check Eligibility.
-
If the STC requested does not match the STC returned:
- A message appears: "Payer Returned Different Benefits", with details of the STC(s) requested and the STC(s) returned.
-
Click View Benefits to see the returned benefits
or
-
Click Perform New Check to run a new custom check
- The Payer-Provided Eligibility Details page appears, displaying the Service Types tab with the payer's response for the STC(s) you requested.
Important: When you manually check eligibility, wait 20 seconds for a response from the payer (or an error message) before you attempt to check eligibility again.