 User Guide — Remittance Posting After Voiding Charges
User Guide — Remittance Posting After Voiding Charges
athenahealth recommends that you wait until the initial payer adjudication has been completed and remittance has been received and posted to a claim before you void any charges. When the action of voiding a charge occurs before remittance has been posted, the corrective process depends on timing. athenahealth will post remittance depending on when the charge was voided.
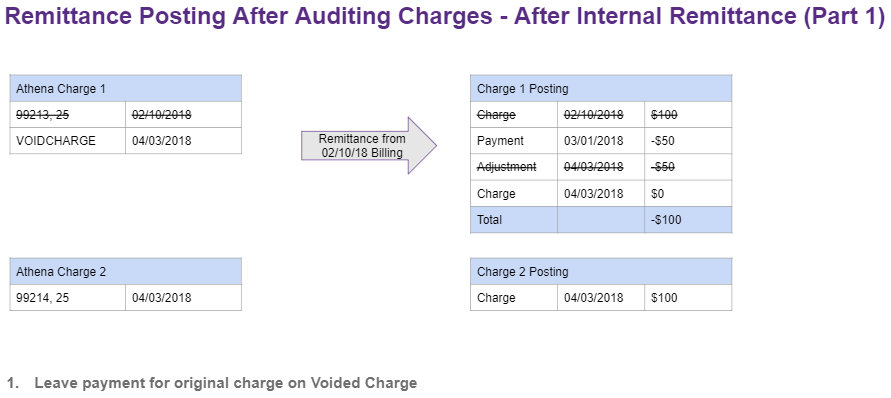
- As athenahealth has already received and posted the remittance which includes the original payment, contractual adjustments, and transfers should currently be posted to the charge you are voiding.
- For additional guidance on how to void a charge, or add a new corrected charge, and resubmit a corrected claim to the payer, please reference section [To add the VOIDCHARGE Procedure Code].
- If there was previously payment on the voided charge, that charge will now be in an overpaid state [see above].
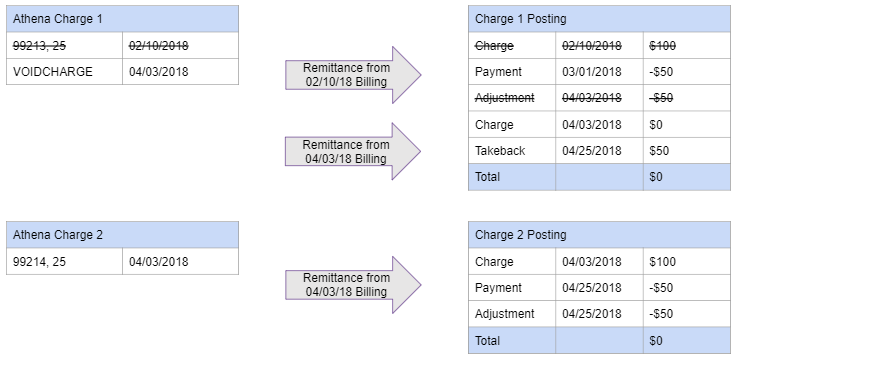
- When remittance with the corrected claim information is received, there should be a reversal for the payment on the voided charge. athenahealth will post the reversal to the VOIDCHARGE line [see below] closing the charge.
- The payment for the corrected charge, as well as any contractual adjustments or transfers, will be posted to the corrected charge line closing the corrected charge.
- If you have determined a charge needs to be voided before the initial remittance is received, please follow the below steps. For additional guidance on how to void a charge or add a corrected charge please reference section [To add the VOIDCHARGE Procedure Code].
- Do not resubmit a corrected claim until after remittance has been received. Submitting additional information to the payer before we have received initial remittance can lead to inaccurate tracking and the possibility for duplicate denials.
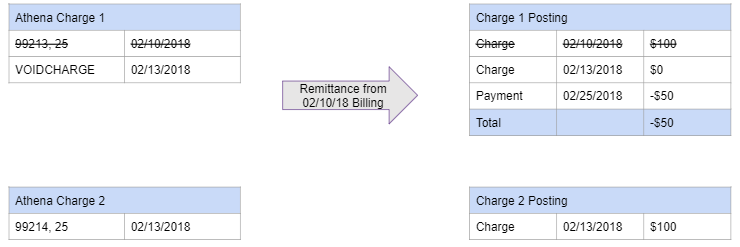
- Remittance is received with old information. Payment for the voided charge will be posted to the voided charge but any contractual adjustments or transfers returned will not be applied. If payment was returned on the voided charge that charge will now be in an overpaid state [see above].
- Once all of the remittance has been posted you will need to verify the claim has been updated accurately and send out a corrected claim. If you need information on how to send out a corrected claim, please reference [To void a charge and resubmit a corrected claim to a payer].
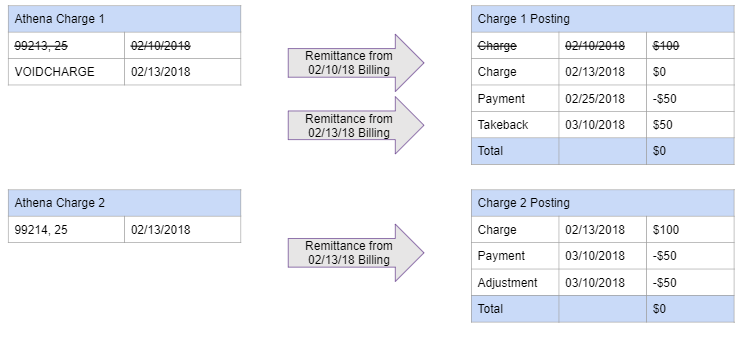
- After athenahealth receives updated remittance, the new adjudication should contain a reversal for the voided charge payment as well as new payment, contractual adjustments, and transfers for the corrected charge [see below]. The reversal should be posted to the voided charge while all new remittance should be posted to the corrected charges.
athenahealth assumes that a denial received on a voided charge requires no further action by the practice. Once you void the charge you should then resolve any other denials, make any further corrections to the claim, and resubmit to the payer for corrected adjudication.
When a charge has a global adjustment posted to it prior to voiding you should follow the guidance on how to void a charge and treat the global adjustment as a contractual adjustment [To add the VOIDCHARGE Procedure Code]. You should re-submit the claim with any additional corrections in order to receive updated remittance from the payer.
If athenahealth receives a global adjustment on a voided charge, it will not be posted. Our recommendation is to resubmit the claim with any additional corrections in order to receive updated remittance from the payer.
athenahealth recommends that you resubmit the claim after making changes to the claim in order to provide the payer with the most up-to-date information. This will result in the most accurate adjudication for the services provided. Once the payer has received the corrected information, they will initiate a takeback or request a refund for the payment on the voided charge.
Note: In order for the procedure code to be valid at charge entry, it must be listed in the allowable and fee schedule for the payer.
- Display the Fee Schedules page: On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Fee and Allowable Schedules, click Fee
Schedules.
>Billing. In the left menu, under Practice Links — Fee and Allowable Schedules, click Fee
Schedules. - Click edit procedures fees for the schedule to update. The Procedure Fees page appears.
- Look at the heading to verify the payer for this schedule. (If you are viewing the wrong schedule, click Fee Schedules on the left side of the page).
- Click Add New. The Add Procedure Code view appears.
- CPT/HCPCS code — Enter the name of the procedure code, in this case VOIDCHARGE.
- Description — Enter a description for the new procedure code.
- Patient-facing description — When this field is populated, this description overrides the regular procedure code description on patient statements.
- Amount — Enter the fee for the procedure, in this case, $0.00.
- Click Save.
- Review all procedure codes listed to identify the charge to be voided.
- Actions — Select Update Codes.
- Under the appropriate Diagnosis Charge, locate the procedure code to be voided.
- Enter the VOIDCHARGE procedure code.
If there is a modifier listed, delete the modifier. - Claim Note — Enter a claim note to describe the changes you made and why.
- Click Submit Claim.
Claim Rule 16787 will fire, adding a claim note stating that VOIDCHARGE is not a valid code, this charge will be suppressed upon claim submission. - Return to the Claim Action page and select Add Kick Reason from the menu at the top of the page.
- Kick Reason — Enter DRPBILLING.
- Claim Note — Enter a claim note to describe the changes you made, and why.
- Click Submit.
athenaOne Net applies the DRPBILLING kick code to the claim and moves the claim to athenahealth to review for payer-specific requirements.