Medicare Allowable Variance – Best Practices
The purpose of the Medicare Allowable Variance report is to identify charges that Medicare allowed below or above the expected amount. This document outlines best practice workflows to support follow up with Medicare for any claims with variance.
See Identify Medicare Allowable Variance — Medicare Only tab on Payment Mismatch Tracking for more information.
Medicare Allowable Variance – Payment Mismatch Tracking Report Best Practice Variance Recovery Workflow
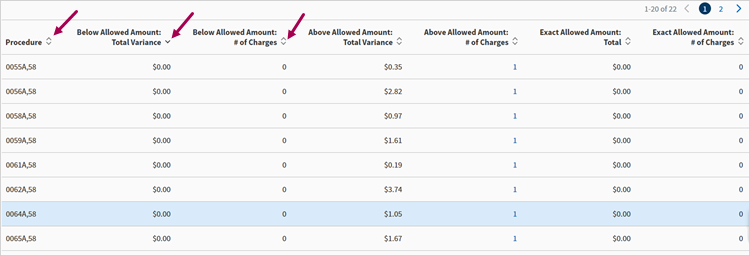
After producing the Payment Mismatch Tracking data, there may be various columns populated with Below, Above and Exact totals based on # of Charges and/or Variance. The Procedure Code header may be the driver of the potential reimbursement recovery area in which Medicare Appeals will be initiated. Users can sort any column both ascending and descending and have the option to download to CSV file.
The sample screen shot shown below provides the data output once the Payment Mismatch data is produced.
Prior to initiating a claim appeal process, utilize the data output from the Payment Mismatch report to determine root causes, identify trends and determine next steps with appeals and/or potentially adjusting fee schedules. One potential identifier of a trend is rows with the same variance percentage. Some common variance root cause trends are:
- Credentialing – Provider processed as non-participating
- Coding – Modifiers affecting Allowable, Multiple service reduction; Mid-Level Providers
- Charges less than Allowed Amount
- Identify Procedure Code and Column Value in which additional A/R review is required. This may include isolating contributing factors such as Modifiers and date range of either Payment Posting or Service Date.
- Download CSV file for easy sorting for additional A/R resolutions steps.
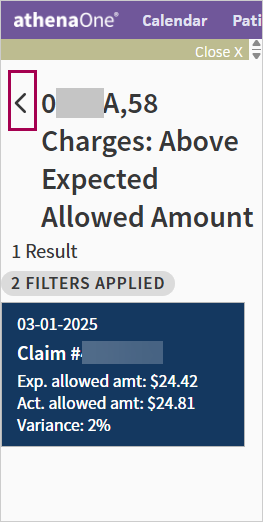
- Leverage both CSV files and results in athenaOne to review individual Claim Visit results. The Claim ID hyperlink within the report will provide direct review of each claim and ease of returning to the original Medicare report results by clicking the Back button in the upper left panel of the Visit n Claim page.
Prepare to build your conversation with the payer regarding your Medicare Allowable variance claims that are within the appeal time. It is important to know how the payer processed the claim, the explicit reason for the below allowed amounts and to be able to explain the reason clearly, whether you are submitting the reconsideration online or via telephone. In cases where a root cause may impact a significant number of claims, there may be opportunity to submit a bulk appeal instead of individual appeals.
Telephone claim reconsideration submission:
- Provide detailed information to the representative about why the claim was not processed according to the contract. This should include the expected amount allowed based on the Medicare Fee Schedule.
- When the claim is sent back for adjustment make sure to request the call reference number for the call.
- Let the payer representative know you have multiple claim submissions and request the most effective way to submit for adjustment.
- Ask for contact information for the Provider Relations Manager/Network Manager if you need to escalate the below allowed amount issue.
- If your hold time is too long you should check to see if a claim adjustment request can be done online.
Once a claim reconsideration project has been submitted to the payer, it is imperative that you perform consistent follow-up. As previously mentioned, most payers take 30-45 business days for initial claim determination. Once this initial time has passed, you should follow up with the payer at least once every 1-2 weeks. Whether working with a claims project analyst or provider representative, an email or phone call should be placed to request status update for the project.
- Due to these claims payments previously posted, the monitoring of the appeal statuses will be potentially tracked via excel spreadsheet.
- Provide the details of the below allowable issue and original submission date.
- Each time contact is made with the payer, document within tracking document & set the next follow-up due date.
- Build a working relationship with the payer.
- Once the payer agrees to reprocess the claim reconsideration project and provides a completion date of claim adjustment, request the final reprocessed dollar amount. Payers will often provide a spreadsheet of the adjusted claims that will include the claim information (patient name, DOS, charge amount, adjusted allowed amount, etc.). This information will be used to compare against received payments on athenaOne and confirm the total dollar amount recovered for the underpayment issue that will be reported back to the client.