Capitation Wizard
This page allows you to create, update, and delete capitation policies. A "capitation policy" is the athenaOne term for a set of components that defines the capitation contract to the system. Capitation policies are used by the Capitation Wizard to apply adjustments to charges covered by capitation contracts. Define one capitation policy for each capitation contract in your practice. If you need to bill for ICD-9 and ICD-10 codes under the same contract, create two policies: one using ICD-9 codes and one using ICD-10 codes.
On the Main Menu, click Settings![]() >Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard
>Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard
- Display
the Capitation Wizard page: On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard.
>Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard. - Name — Enter the name of the capitation policy. The name should be unique and appropriate for reference purposes. To ensure that athenahealth can properly post payments, include the payer's name as it appears on its remittance.
- Effective date — Enter the date that the capitation contract becomes effective.
- Expiration date — If applicable, enter the date that the capitation contract expires. Leave this field blank to allow the contract to continue indefinitely.
- Provider group — Select the provider group covered by the capitation contract.
- Insurance
packages — Enter the insurance packages
covered under the capitation contract. You can click the Select
all insurance packages option, or you can enter package numbers in the fields. If you do not click the Select
all insurance packages option, you must enter at least one insurance package number (type a period to access the Insurance
Package Lookup tool). To enter more package numbers after you fill a row, click the plus
 icon to the right of the row.
icon to the right of the row. - Procedure
codes
— Enter the set of CPT codes covered under the capitation contract. You can click the Select
all procedure codes option, or you can enter CPT codes in the fields under Include these codes. If you do not click the Select
all procedure codes option, you must enter at least one CPT code.
Note: MISC procedure codes do not work with the Capitation Wizard functionality.
When you enter codes in the fields, - You can type a period to use the lookup tool.
- You can use the asterisk (*) wildcard character. For example, enter "9*" to indicate that all CPT codes beginning with "9" should be capped.
- You can enter a range of CPT codes in one field. For example, enter 99213-99222 to include all codes from 99213 to 99222, including both 99213 and 99222.
- To enter more codes after you fill a row, click the plus
 icon to the right of the row.
icon to the right of the row. - Diagnosis
codes — Select ICD-9 or ICD-10. You can enter ICD-9 or ICD-10 codes in a policy, but you cannot enter both ICD-9 and ICD-10 codes
in one policy. However, if you have capitation contracts that span the October 1, 2015, transition date for ICD-10, you can create two capitation policies for the same contract: one with ICD-9 codes and one with ICD-10 codes.
Leave this field blank to include all ICD-9 or ICD-10 codes. When you enter ICD-9 or ICD-10 codes in the fields, - You can type a period to use the lookup tool. You can search for ICD-10 diagnosis codes using ICD-9 codes, ICD-10 codes, or SNOMED terms.
- You can use the asterisk (*) wildcard character. For example, enter "T67*" to indicate that all ICD-10 codes beginning with "T67" should be capped.
- To enter more codes after you fill a row, click the plus
 icon to the right of the row.
icon to the right of the row. - Providers — Select the individual providers covered under the capitation contract.
- Departments — Select the departments associated with this capitation contract.
- Click Save. The capitation policy name appears in the list of capitation policies at the bottom of the page. If the data you enter contains any errors, you receive an error message after you click Save; the data is not saved.
In the Exclude these codes
fields, enter the set of CPT codes NOT covered under the capitation contract. Any codes entered in these fields override the codes listed under Include these codes. You can use the lookup tool, the wildcard character, and code ranges in the Exclude these codes
fields, just as you can for codes in the Include these codes fields.
In the Exclude these codes fields, enter the set of ICD-9 or ICD-10 codes NOT covered under the capitation contract. Any codes entered in these fields override the codes listed under Include these codes. You can use the lookup tool and the wildcard character in the Exclude these codes fields, just as you can for codes in the Include these codes fields.
Wildcards and procedure codes
You can use wildcards to enter procedure codes and diagnosis codes. A procedure code wildcard is a truncated procedure code, ending with an asterisk (for example, 992* includes all procedure codes beginning with 992). Wildcard asterisks can appear only at the end of a code or with no other characters in a field. For example:
- Set up a capitation policy for insurance package 1234, using an asterisk (*) alone in the first (required) procedure code field. This policy applies this rule: "For insurance package 1234, adjust off all charges."
- Set up a capitation policy for insurance packages 1355 and 3424 for procedure codes 992* and 993*. This policy applies this rule: "For insurance packages 1355 and 3424, adjust off all charges for procedure codes beginning with 992 and 993."
Modified procedure codes are included under the CPT code (for example, 99213,25 is treated the same as 99213). To exclude a modified CPT code, list it under the Exclude these codes fields.
- Display the Capitation
Wizard page: On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard.
>Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard. - Locate the capitation policy name in the Capitation Policies list at the bottom of the page.
- Click the update
link. The policy details appear in the fields under "Update Capitation Policy" at the top of the page.
Note: To display the change history of the capitation policy, click the Audit history link below the Save and Cancel buttons. - Update the fields as described in "To create a capitation policy" (above).
- Click Save. The updated capitation policy appears in the Capitation Policies list.
- Display
the Capitation Wizard page: On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard.
>Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard. - Locate the capitation policy name in the Capitation Policies list at the bottom of the page.
- Click the delete link.
- Click OK to confirm the deletion.
- The capitation policy name appears "disabled" in the Capitation Policies list at the bottom of the page, and an undelete link becomes available to restore the capitation policy.
- Display
the Capitation Wizard page: On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard.
>Billing. In the left menu, under Practice Links — Insurance Packages, click Capitation
Wizard. - Click the Test
capitation policies
link above the list of policies.
The Capitation Wizard Test Harness window appears. - Enter "dummy" charges, including a specific procedure code, two diagnosis codes, an insurance package, and so forth. (A dummy charge must have at least a procedure code, a primary diagnosis, and an insurance package to receive an answer from the test.)
- Click Check to see whether the dummy charge would be capped.
You can reconcile the charges included in your monthly service invoice with the capitation payments posted in athenaOne using the Capitation Payments report:
- Display the Capitation Payments page: From the Main menu, click Financials > Capitation Payments.
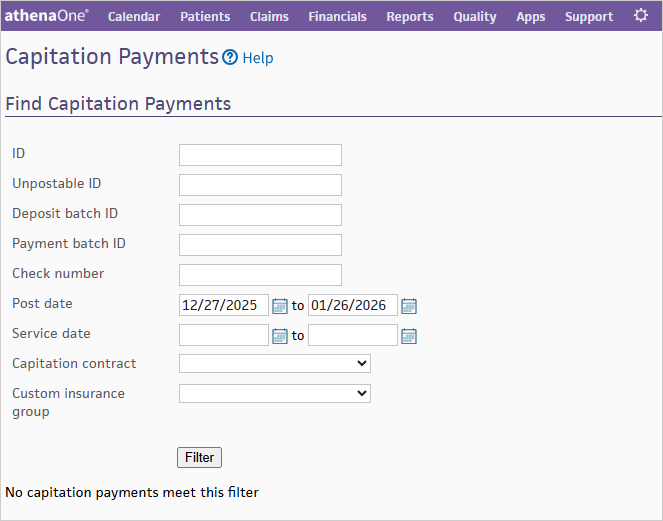
- Enter your filter criteria to search for specific Capitation Payment matching results.
- Click Run Report.
| Unpostable ID |
Click the linked unpostable ID to display the Remittance Record page for the capitation payment. |
|---|---|
| Payment Batch ID |
Click the linked payment batch ID to display the Edit Payment Batch page for the payment batch associated with the capitation payment. |
| Provider Group Name |
Name of the provider group associated with the capitation payment. |
| Provider Group ID |
ID of the provider group associated with the capitation payment. |
| Provider Name |
Name of the provider associated with the capitation payment. |
| Unpostable Post Date |
Date that the capitation payment was posted. |
| Unpostable Amount |
Amount of the capitation payment. |
The Capitation Wizard is an athenaOne utility that runs nightly. It identifies any BILLED charges covered by a capitation policy and creates automatic adjustments to write off the charges.
Important: For the Capitation Wizard to work correctly, you must create a capitation policy for each capitation contract in effect for your practice. (Use the Capitation Wizard page to define capitation policies.)
- If the claim contains only capitated charges, the wizard should create the capitation adjustments and then transfer the expected copay amounts to the next responsible party.
- If the claim contains both capitated charges and non-capitated (fee-for-service) charges, the Capitation Wizard creates the capitation adjustment only for charges that are covered under the capitation contract. The Capitation Wizard suppresses the immediate transfer of the copay to the secondary, so that when the primary payer adjudicates the fee-for-service charges and submits the remittance advice, the secondary claim is processed normally.
For primary claims, when you create a capitation policy, any matching charges that are still in BILLED status are "capped" according to the new capitation policy, regardless of the age of the charge. Any new matching charges are also capped.
Are capped procedures billed with full charges, or do they show a $0 charge?
They are billed at the full charge amount. The Capitation Wizard then applies the capitation adjustments, leaving a $0 balance.
If a capped charge is resubmitted for some reason, what happens?
If the claim is resubmitted, the charges covered by a capitation policy do not appear unless another transaction voided the capitation adjustment. For example, acknowledgment kicks and EOB denials both void the capitation adjustment. But if there is no void, the charges are not included on the claim when it is resubmitted.
If you edit or delete a capitation policy, the changes to the capitation policy apply only to future charges — BILLED status charges are not affected by the capitation policy edits. athenaOne does not re-evaluate BILLED status charges after they are capped.
Allowable schedules and capitation contracts
If an allowable schedule has been created for the payer, the Capitation Wizard:
- Creates a contractual adjustment equal to the difference between the charge amount and the allowable amount (from the allowable schedule)
- Creates a transfer in the amount of the expected copay (if a copay is expected for this charge)
- Creates a capitated adjustment equal to the remaining charge balance
If an allowable schedule has not been created for the payer, the Capitation Wizard:
- Creates a capitation adjustment — the copay amount is deducted, then the capitation adjustment is created to cover the remainder of the charge amount
- Creates a transfer in the amount of the expected copay (if a copay is expected for this charge)
Note: You are required to report to us your capitation payments and link them to the services they cover using the Capitation Wizard in athenaOne.
| Name |
Name of the capitation policy. To ensure that athenahealth can properly post payments, ensure that this name includes the payer's name as it appears on its remittance. |
|---|---|
| Effective date |
The date that the capitation contract becomes effective. |
| Expiration date |
The date that the capitation contract expires. |
| Provider group |
Limit this capitation policy to a particular provider group. If no provider group is selected, the contract is applied universally. |
| Insurance packages |
List the insurance packages that have capped procedure codes for this policy. Press "." to search for insurance packages. |
| Procedure codes |
List the procedure codes that are capped for this item. Press "." to search for procedure codes. Note: MISC procedure codes do not work with the Capitation Wizard functionality. |
| Exclude these codes |
Enter a set of procedure codes that should be excluded from the above list. For example, enter 9* in the Procedure codes field to indicate that all codes beginning with "9" should be capped; then enter 9921* in the Exclude these codes field to indicate that those CPT codes should not be capped.
Exception codes can be used even if the Select all procedure codes option is not selected.
Note: MISC procedure codes do not work with the Capitation Wizard functionality. |
| Diagnosis codes |
Select ICD-9 or ICD-10, then enter a set of diagnosis codes (if necessary, leave blank to apply to all diagnosis codes). The diagnosis codes that you enter will apply to either the primary or secondary diagnosis for the charge. |
| Exclude these codes |
Enter a set of diagnosis codes that should not be capped. These codes override any diagnosis codes that you entered above. |
| Providers |
Select the individual providers covered under the capitation contract. |
| Departments |
Select the departments associated with this capitation contract. |