User Guide — Patient Risk Adjustment and the Diagnosis Gaps Dashboard
User Guide — Patient Risk Adjustment and the Diagnosis Gaps Dashboard
This user guide provides a comprehensive overview of patient risk adjustment and reimbursement in athenaClinicals and includes instructions on how to use the Diagnosis Gaps dashboard to view and address a patient's diagnosis gaps.
You can also refer to this user guide for details on:
- The data included in the Diagnosis Gaps dashboard.
- Reporting on diagnosis gaps.
- Display and reconciliation logic for diagnosis gaps.
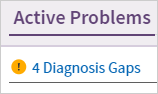
In the patient chart, click the Problems tab on the left side of the page. The Patient Risk score or x Diagnosis Gaps appears at the top of the list. Click this link to view the Diagnosis Gaps dashboard.
To update the Diagnosis Gaps dashboard, you must have the Clinicals: Edit Chart permission.
As the healthcare industry moves toward value-based reimbursement, payments are increasingly tied to the type of care provided and the associated clinical outcomes. Financial success depends on proper assessment of your patient population's risk level based on their diagnosed conditions.
Hierarchical Condition Category (HCC) Risk Adjustment is a formula used by insurance companies to predict a patient's healthcare costs. An HCC risk score is calculated annually for each patient based on a combination of demographic information and the risk adjustment factor (RAF) for the diagnosis codes submitted on claims. Payers use these scores to determine reimbursement under a variety of risk-based contracts.
In addition to the CMS-HCC risk adjustment model, athenahealth also supports the ingestion of diagnosis gaps from other risk models, including Chronic Illness and Disability Payment System (CDPS) and Health and Human Services Hierarchical Condition Categories (HHS-HCC).
Diagnosing chronic conditions regularly and with the appropriate specificity, such as adding the amputation status to a diabetic patient’s diagnosis, more accurately captures your patients’ disease burden, which enables the appropriate reimbursement for your patients' care.
Even if your organization is not in a risk contract, accurately capturing all your patients’ diagnoses on claims to the highest level of specificity is valuable for a few reasons:
-
Improved insight for both you and your payers into your population's disease burden, as well as patients who are potentially eligible for care management or reduced out-of-pocket costs
-
Improved performance on quality metrics that are adjusted for patient acuity or rely on diagnoses documented on claims to determine eligible cases
-
Reduced administrative burden by avoiding chart audits from payers to identify clinically inferred diagnosis gaps
athenahealth has developed functionality within athenaOne to help organizations document and bill appropriately for chronic conditions tied to risk adjustment.
In athenaClinicals, the Diagnosis Gaps dashboard displays gaps in documentation for high-volume, high impact chronic conditions, such as diabetes, during the point-of-care workflow. In just a few clicks, a provider can move a clinically verified diagnosis surfaced in the Diagnosis Gaps dashboard into the Assessment & Plan (A/P) section of the encounter. athenahealth pulls diagnosis gaps from third party external sources, athenahealth claims, and claims added manually by coders.
In athenaOne, reports are available in the Report Library to provide real-time, actionable insight into how your organization is performing related to several metrics that athenahealth has developed specifically for risk adjustment. For more details, see Reporting on diagnosis gaps.
Both the features in athenaClinicals and the reports available in the Report Library run on a calendar-year basis because most risk contracts reset at the beginning of the calendar year.
As the industry moves toward a value-based healthcare system, an increasing portion of your revenue will be tied to how effectively your organization can control costs for complex patients. However, you're compensated properly only if payers know how complex your patients are.
There are a few reasons why organizations aren't always compensated properly:
-
Diagnoses are not documented to the highest level of specificity
-
Comorbidities of the primary disease (which impact risk scores) are not captured
-
Risk scores reset annually and chronic conditions are not consistently recaptured on claims
It takes buy-in from an entire organization to ensure that diagnoses are documented properly for risk adjustment:
-
Billing providers or clinical staff should review the Patient Risk Adjustment (HCC/RAF): Diagnosis Gaps Report before patients come in so that they have a sense of the patients' chronic conditions and where any gaps may exist in documentation or care.
-
Billing providers should review the Diagnosis Gaps dashboard as part of pre-visit planning and/or during an exam to ensure that patients' chronic conditions are addressed and documented appropriately.
-
Practice managers and leaders should review the Patient Risk Adjustment reports to assess how well providers and departments are documenting diagnoses and using the patient risk adjustment features in athenaClinicals.
-
Coding staff should use the Diagnosis Gaps dashboard to add suggested diagnoses based on chart review when clinically appropriate, if this is part of their workflow.
The Diagnosis Gaps dashboard in the Problems tab of the patient chart displays patient risk adjustment information for high-volume, high-impact chronic conditions, such as diabetes. Providers and clinical staff can use the dashboard to identify gaps in documentation of chronic conditions within the calendar year and move those gaps directly into the Assessment & Plan.
The Diagnosis Gaps dashboard uses claims from the past 3 years to identify potential opportunities for rediagnosis. In order for a patient to be considered "rediagnosed" for the purposes of the Diagnosis Gaps dashboard, the HCC diagnosis code must be included on a claim in the current calendar year.
For more information about the HCC risk adjustment model, see HCC model.
Providers and clinical staff can use the Diagnosis Gaps dashboard (accessible from the Problems tab of the patient chart) to review and capture diagnosis gaps. Both the patient's Problems list and the Assessment & Plan (A/P) section of the encounter display an alert if there are diagnosis gaps to be addressed:

The Diagnosis Gaps dashboard displays a patient's open, addressed, and dismissed diagnosis gaps:
- Open — This tab displays clinically verified and clinically inferred gaps that haven't been acted upon in the current risk cycle. Gaps are sorted numerically by the HCC category, and each gap includes the source and additional supporting details. The tab displays gaps in two sections:
- Previously Diagnosed — This section displays clinically verified diagnoses. These include diagnoses from the patient's claim history, diagnoses suggested by billing staff based on chart audits, and prior diagnoses shared through third parties.
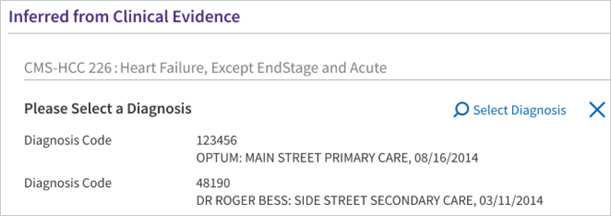
- Inferred from Clinical Evidence — This section displays clinically inferred diagnoses. These diagnoses are suggested based on clinical evidence shared by third parties, such as payers.
Note: For more details on the difference between clinically verified and inferred diagnoses, see Clinically verified and inferred diagnoses.
- Addressed — This tab displays diagnosis gaps that were addressed in an encounter and appeared on a claim in the current year. Any addressed diagnosis in the previous year resurfaces in the Previously Diagnosed section of the dashboard for re-diagnosis at the start of the new calendar year (January 1st).
- Dismissed — This tab displays gaps that the provider dismissed as not clinically relevant to the patient. Each dismissed gap includes the dismissal justification (if provided) and can be reinstated to the Open tab if needed.
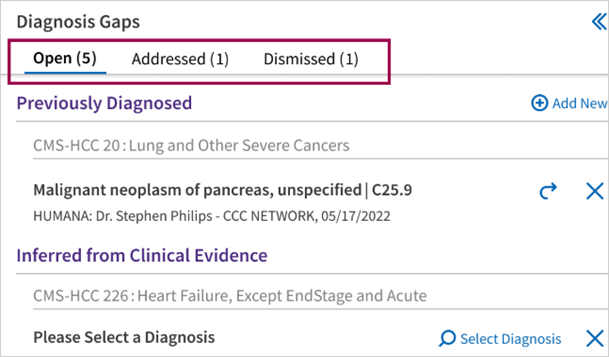
Providers can use the dashboard to identify potential risk-weighted diagnoses that have not been recorded in the current year and to view the overall risk of the patient. Providers can either accept a diagnosis to add it to the Assessment & Plan section of the encounter or dismiss the diagnosis to remove it from the dashboard.
The Diagnosis Gaps dashboard supports rules and workflows to ensure proper documentation of buddy codes. Buddy codes are secondary billing codes that are required for certain ICD-10 codes to fully justify the associated HCC.
Clinically verified diagnoses
Clinically verified diagnoses have previously appeared on a claim for a patient and are eligible for recapture in the current calendar year. The Diagnosis Gap dashboard displays clinically verified diagnoses in the Previously Diagnosed section.
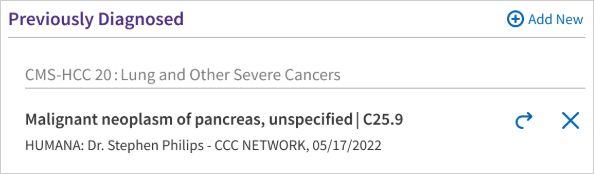
Clinically verified gaps:
-
Have associated ICD-10 codes that have previously appeared on a claim for a patient.
-
Are identified natively from athenahealth claims.
-
Can be manually added.
-
Are surfaced from third-party integrations via API (for more details, see Understanding the data in the Diagnosis Gaps dashboard).
Billing staff and others can manually add clinically verified diagnoses to the Diagnosis Gaps dashboard, based on gaps that they find on claims, by clicking ![]() Add New next to Previously Diagnosed.
Add New next to Previously Diagnosed.
Note: Currently, only clinically verified CMS-HCC diagnosis gaps can be added manually.
The clinically verified diagnosis appears on the Diagnosis Gaps dashboard and the patient's gap risk score increases to accommodate the new diagnosis. During this patient's next visit, the provider can view the clinically verified diagnosis on the Diagnosis Gaps dashboard and, if applicable, add it to the Assessment & Plan section of the encounter.
Each clinically verified diagnosis includes the source (for example, MANUAL or CLAIM), which identifies the information that supports the suggestion (for example, details on a historical claim or a note from the billing staff).
See the following step-by-step instructions for addressing diagnoses in the Diagnosis Gaps dashboard:
- To add a clinically verified diagnosis to the Diagnosis Gaps dashboard
- To accept a clinically verified diagnosis during an encounter
- To accept a clinically inferred diagnosis during an encounter
- To update an ICD-10 code
Clinically inferred diagnoses
Clinically inferred diagnoses are inferred from clinical evidence. The dashboard displays clinically inferred diagnoses in the Previously Diagnosed section.
A clinically inferred diagnosis is one that is likely to be present for a patient but is not supported by a documented condition in the patient’s chart or on a claim. This should not be confused with a previously dismissed condition. Supporting clinical facts are provided to help you decide if you should dismiss a diagnosis, clean up the patient chart, or document an HCC-related problem or diagnosis for the patient.
The clinical evidence surfaces with the clinically inferred diagnosis gap in the Diagnosis Gaps dashboard. Clinically inferred diagnoses may be based on the following: Medications, Procedures, Measurements and Results, Previous Diagnoses, and Notes.
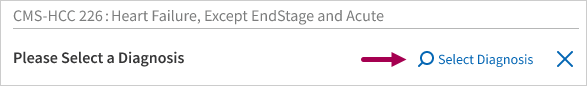
Clinically inferred diagnoses are based on the condition category. The provider must determine the ICD-10 code. In addition, the Diagnosis Gaps dashboard displays only clinically inferred diagnosis gaps from third-party external sources received via API.
For step-by-step instructions on addressing clinically inferred diagnoses in the Diagnosis Gaps dashboard, see To accept a clinically inferred diagnosis during an encounter.
The Diagnosis Gaps dashboard displays clinically verified and inferred diagnosis gaps added into the patient's record from payers. Provider feedback is sent to payers on the day following any action taken on external diagnosis gaps received from payers.
Note: Payer diagnosis gaps appear if your organization uses both athenaClinicals and athenaCollector. They also appear if you use athenaClinicals only and are enrolled in HEDIS or MIPS quality programs or have payer data enabled. If you want to opt-out of payer data appearing in athenaClinicals, contact the CSC.
-
You'll notice that the data from the partners includes the ICD-10 code (for clinically verified gaps only) and the relevant source information.
-
Additional supporting details related to the external diagnosis gaps, such as provider or hospital names and payer names, are also shown when received by payers. The name of the health insurance plan appears as the source of the gap, in lieu of the payer name, when that information is provided by the payer.
-
The risk score displayed in the dashboard is adjusted to include the external CMS-HCC diagnosis gaps received. These diagnosis gaps are actionable and providers can dismiss, reinstate a dismissed diagnosis, or choose a diagnosis during the encounter workflow.
Patient diagnosis gaps received from payers are reconciled against the gaps in the patient's chart from other sources (manual/past year claims). This ensures duplicate codes only appear once.
For more details on the reconciliation and display logic, see How diagnosis gaps are reconciled and displayed.
If a clinically verified or inferred diagnosis is not clinically relevant to the patient, the provider can dismiss the diagnosis to remove it from the Open tab of the Diagnosis Gaps dashboard. Dismissed diagnosis gaps appear in the Dismissed tab of the dashboard.
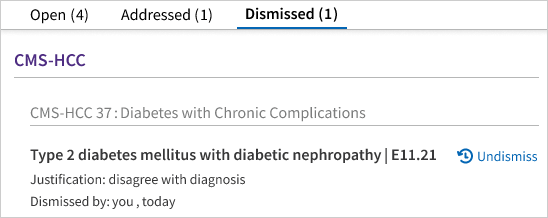
Providers can select a reason for dismissal or enter a justification when dismissing the gap. For example, if a patient no longer has a skin cancer that was diagnosed and treated in the previous year, the provider can select condition resolved as the reason for dismissal.
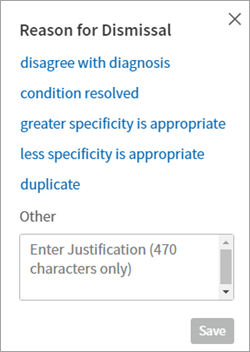
Providers are encouraged to use this feature to dismiss diagnoses that are no longer clinically relevant. athenahealth monitors the dismissal rates across the network and adjusts the diagnoses that surface in the Diagnosis Gaps dashboard based on how often providers dismiss diagnoses.
Note: Diagnosis gaps are dismissed at the ICD-10 code level. This means that if a provider dismisses an ICD-10 code, all instances of the same ICD-10 code received from various sources are also considered dismissed in the Diagnosis Gaps dashboard. If an ICD-10 code is captured from a claim, and a provider has previously dismissed that same ICD-10 code, the Diagnosis Gaps dashboard displays the diagnosis as dismissed.
For step-by-step instructions, see To dismiss a diagnosis.
See more:
-
If you dismiss a diagnosis from the Diagnosis dashboard in error, or the diagnosis is later found to be relevant for the patient, you can reinstate the diagnosis and return it to the list as an open gap. For step-by-step directions, see To reinstate a dismissed diagnosis.
-
For details on the retention period for dismissed gaps, see Retention period for dismissed diagnosis gaps.
-
For details on the system behavior in various scenarios for dismissing and reinstating diagnosis gaps, see Dismissing and reinstating diagnosis gaps.
Tip: Administrators can set this preference at the practice level so the same preference is applied to all users. See To update practice-wide user preferences.
- Display the User Preferences page: On the Main Menu, click Settings
 > User Preferences.
> User Preferences. - Select the Show patient risk score instead of potential diagnosis count in Problem List option.
- Click Submit.
Billing staff and others can manually add clinically verified diagnoses to the Diagnosis Gaps dashboard. Manually added diagnoses appear with the source MANUAL and identify the information that supports the suggestion (for example, a note from the billing staff).
- In the patient chart, click the Problems tab on the left side of the page. The Patient Risk score or x Diagnosis Gaps appears at the top of the list. Click this link to view the Diagnosis Gaps dashboard.
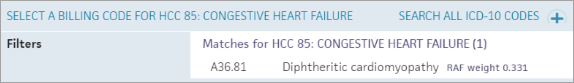
- In the Open tab, click
 Add New next to Previously Diagnosed. The diagnosis selector opens.
Add New next to Previously Diagnosed. The diagnosis selector opens. - Search for and select the most appropriate diagnosis. Each diagnosis includes an associated RAF weight.
- Reason — Add a reason for the suggestion and then click Add.
The diagnosis appears in the Previously Diagnosed section of the Diagnosis Gaps dashboard.
During this patient's next visit, the provider can review the diagnosis and, if applicable, add it to the Assessment & Plan section.
During an encounter, you can accept a clinically verified diagnosis from the Diagnosis Gaps dashboard and add it directly to the Assessment & Plan section of the encounter.
- In the patient chart, click the Problems tab on the left side of the page. The Patient Risk score or x Diagnosis Gaps appears at the top of the list. Click this link to view the Diagnosis Gaps dashboard.
- Select the Open tab. The Diagnosis Gaps dashboard displays clinically verified diagnoses in the Previously Diagnosed section.
- If the ICD-10 code requires a manifestation, click SPECIFY MANIFESTATION and make a selection from the list.
Note: Buddy codes are secondary billing codes that are required for certain ICD-10 codes to fully justify the associated HCC. The Diagnosis Gaps dashboard supports rules and workflows to ensure proper documentation of buddy codes. - Click
 to add the ICD-10 code to the Assessment & Plan section of the encounter. athenaOne automatically maps the ICD-10 code to the primary IMO diagnosis when you add the gap to the A&P.
to add the ICD-10 code to the Assessment & Plan section of the encounter. athenaOne automatically maps the ICD-10 code to the primary IMO diagnosis when you add the gap to the A&P.
Note: The addressed gap does not appear as closed in the Addressed tab of the dashboard until the diagnosis is seen on a claim. In addition, only CMS-HCC diagnosis gaps show as closed. For non-CMS-HCC gaps, if you select an ICD-10 code and that code is seen on a claim, the condition category is marked as appearing on the claim ("APPEAREDONCLAIM" status) and the non-CMS-HCC gap no longer appears in the Diagnosis Gaps dashboard.
During an encounter, you can accept a clinically inferred diagnosis from the Diagnosis Gaps dashboard and add it directly to the Assessment & Plan section of the encounter.
- In the patient chart, click the Problems tab on the left side of the page. The Patient Risk score or x Diagnosis Gaps appears at the top of the list. Click this link to view the Diagnosis Gaps dashboard.
- Select the Open tab. The Diagnosis Gaps dashboard displays clinically verified diagnoses in the Inferred from Clinical Evidence section .
- Click Select Diagnosis to search for and select an ICD-10 code.
- If the ICD-10 code requires a manifestation, click SPECIFY MANIFESTATION and make a selection from the list.
Note: Buddy codes are secondary billing codes that are required for certain ICD-10 codes to fully justify the associated HCC. The Diagnosis Gaps dashboard supports rules and workflows to ensure proper documentation of buddy codes. - Click
 to add the ICD-10 code to the Assessment & Plan section of the encounter. athenaOne automatically maps the ICD-10 code to the primary IMO diagnosis when you add the gap to the A&P.
to add the ICD-10 code to the Assessment & Plan section of the encounter. athenaOne automatically maps the ICD-10 code to the primary IMO diagnosis when you add the gap to the A&P.
Note: The addressed gap does not appear as closed in the Addressed tab of the dashboard until the diagnosis is seen on a claim. In addition, only CMS-HCC diagnosis gaps show as closed. For non-CMS-HCC gaps, if you select an ICD-10 code and that code is seen on a claim, the condition category is marked as appearing on the claim ("APPEAREDONCLAIM" status) and the non-CMS-HCC gap no longer appears in the Diagnosis Gaps dashboard.
If a diagnosis is not clinically relevant to the patient, you can dismiss the diagnosis to remove it from the Open tab of the Diagnosis Gaps dashboard.
-
In the patient chart, click the Problems tab on the left side of the page. The Patient Risk score or x Diagnosis Gaps appears at the top of the list. Click this link to view the Diagnosis Gaps dashboard.
-
Hover over the diagnosis and click the Delete icon
 that appears.
that appears.
The Reason for Dismissal menu appears.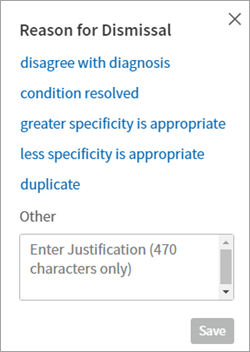
-
To record a reason for dismissing this diagnosis, select one of the reasons displayed. If none of the reasons apply, enter the reason in the Other field (up to 470 characters) and click Save.
-
If you do not want to record a reason for dismissing the diagnosis, click Save
-
-
To view the list of dismissed diagnoses, display the Dismissed tab. Each dismissed diagnosis displays the dismissal justification and the user who dismissed the diagnosis.
Note: Diagnosis gaps are dismissed at the ICD-10 code level. This means that if a provider dismisses an ICD-10 code, all instances of the same ICD-10 code received from various sources are also considered dismissed in the Diagnosis Gaps dashboard. If an ICD-10 code is captured from a claim, and a provider has previously dismissed that same ICD-10 code, the Diagnosis Gaps dashboard displays the diagnosis as dismissed. If you remove a diagnosis from the patient chart by mistake, you can reinstate it (see To reinstate a dismissed diagnosis).
If you dismiss a diagnosis in error, or the diagnosis is later found to be relevant for the patient, you can return the diagnosis to the list.
- In the patient chart, click the Problems tab on the left side of the page. The Patient Risk score or x Diagnosis Gaps appears at the top of the list. Click this link to view the Diagnosis Gaps dashboard.
- Select the Dismissed tab. The number of dismissed diagnoses appears next to the Dismissed tab in the dashboard.
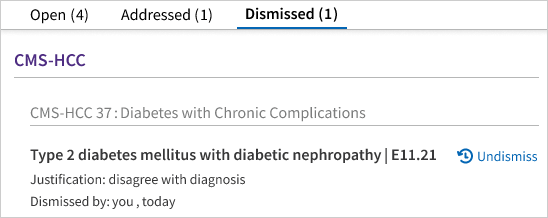
- Click
 Undismiss next to the dismissed diagnosis that you want to reactivate.
Undismiss next to the dismissed diagnosis that you want to reactivate.
The diagnosis reappears in the Open tab.
Follow this procedure during an encounter to update an existing ICD-10 code in the Diagnosis Gaps dashboard.
- In the patient chart, click the Problems tab on the left side of the page. The Patient Risk score or x Diagnosis Gaps appears at the top of the list. Click this link to view the Diagnosis Gaps dashboard.
-
Click Update ICD next to the diagnosis to change the current ICD-10 code to another code.
-
In the ICD-10 code search window, select the appropriate ICD-10 code:
The new code now appears in the Diagnosis Gaps dashboard.
The diagnosis gaps functionality in athenaClinicals sources gaps both natively and externally.
Manual
Providers and billing staff can manually add clinically verified CMS-HCC diagnosis gaps to the Diagnosis Gaps dashboard. athenaOne automatically maps the ICD-10 code to the primary IMO diagnosis when you add the gap to the Assessment & Plan.
Claims
Previous claims within athenaOne are scrubbed and CMS-HCC eligible ICD-10 codes are used to create clinically verified CMS-HCC diagnosis gaps.
athenahealth Population Health
Clinically verified CMS-HCC diagnosis gaps that have been identified as open or closed from athenahealth Population Health are integrated into athenaClinicals.
Third parties
Payers and other third parties share clinically verified and inferred diagnosis gaps via the third party Risk Gaps API, and these gaps surface in athenaClinicals. Risk adjustment workflows can support other risk adjustment models beyond the CMS-HCC model, including CDPS and HHS-HCC.
In addition, customers can share open diagnosis gaps for any risk adjustment model via the third party Risk Gaps API. The Risk Gaps third-party API facilitates publishing patients' diagnosis gaps periodically from external partners and customers. Ingested diagnosis gaps are reconciled and deduplicated before the gaps surface in the risk adjustment workflow.
Payer integrations are enabled by default. If you want to opt-out of payer data appearing in athenaClinicals, contact the CSC. For a comprehensive list of payer partners, see Overview: Moment of Care Connections (MoCC) Participating payers for care gaps and diagnosis gaps.
For more details on the API integrations, see Risk Adjustment on the Developer Portal.
If your organization would like to receive and manage diagnosis gaps from additional risk models, contact the CSC: On the Main Menu, click Support > Success Community > Contact Client Support Center.
If your organization uses athenaClinicals and athenahealth Population Health, data from both products can be used in athenaClinicals to provide more accurate and timely information about a patient's clinically verified diagnoses and risk adjustment factor.
athenahealth Population Health uses three years of historical post-adjudicated claims data provided by payers, including claims from outside the network.
The additional information from athenahealth Population Health can improve the diagnosis and treatment of chronic conditions, reduce manual coordination between ACO administrators and providers, and increase revenue for payment models that are calibrated to the RAF score of the at-risk population.
Because the post-adjudicated claims data from athenahealth Population Health is included, the Diagnosis Gaps dashboard in athenaClinicals shows you a more complete accounting of the following:
- Clinically verified and clinically inferred diagnoses
- Risk adjustment factors
- Risk scores
For more details, see the following Population Health resources:
CMS-HCC risk adjustment model
athenaClinicals has full support of the CMS-HCC risk adjustment model through an HCC engine. Each year, athenahealth updates this engine with CMS-HCC specifications.
Full support of the CMS-HCC model means that athenaClinicals can:
-
Natively identify CMS-HCC diagnosis gaps from all claims for all patients
-
Allow users to manually add clinically verified CMS-HCC diagnosis gaps in the Diagnosis Gaps dashboard
-
Surface a risk score for closed CMS-HCC diagnosis gaps
-
Close CMS-HCC diagnosis gaps based on the ICD-10 codes billed on an eligible claim for an HCC category
For details on the latest HCC to ICD-10 mappings from CMS, see the Risk Adjustment resource from CMS.
Model agnostic approach
Practices that manage diagnosis gaps from risk adjustment models other than the CMS-HCC model, such as CDPS and HHS-HCC, can view and address these clinically verified diagnosis gaps in the Diagnosis Gaps dashboard.
athenaClinicals has limited support for other risk models besides CMS-HCC. athenaClinicals can accept diagnosis gaps from non-CMS-HCC models via the Risk Gaps API and surface those gaps in the Diagnosis Gaps dashboard.
Limited support for non-CMS-HCC gaps means:
-
athenaClinicals can ingest non-CMS-HCC diagnosis gaps received from payers and other third parties via the Risk Gaps API.
-
athenaClinicals cannot calculate risk scores for non-CMS-HCC diagnosis gaps.
-
Non-CMS-HCC diagnosis gaps are not marked as closed in the Addressed tab of the Diagnosis Gaps dashboard; instead, when an ICD-10 code for a non-CMS-HCC gap is seen on a claim, the condition category is marked as appearing on the claim ("APPEAREDONCLAIM" status) and the non-CMS-HCC gap no longer appears in the Diagnosis Gaps dashboard.
Note: Payers and third-party partners can submit non-CMS-HCC diagnosis gaps with flexible risk cycles that are not tied to the calendar year start and end dates, such as for state-specific Medicaid risk adjustment models. For example, payers may submit diagnosis gaps aligned with their preferred risk cycles, such as:
-
Fiscal year (for example, July 1 to June 30)
-
Multi-year risk cycles
-
Multiple risk cycles per year (for example, half-yearly, quarterly)
The CMS-HCC risk adjustment model is used to predict a patient's healthcare costs. A risk score is calculated annually for each patient based on a combination of demographic, interaction and condition count variables and the risk adjustment factor for the diagnosis codes submitted on claims. Payers use these scores to determine reimbursement under a variety of risk-based contracts.
The Diagnosis Gaps dashboard excludes diagnoses from claims with noncompliant procedure codes and places of service per CMS guidelines. For more information on the CMS-HCC model, see the Risk Adjustment resource from CMS.
As of January 1, 2025, 100% of risk scores are calculated using CMS-HCC model version 28 (v28). As a result, the Diagnosis Gaps dashboard accepts and displays only v28 CMS-HCC diagnosis gaps.
There are several reports that you can use to assess your organization's performance against these metrics and assist with pre-visit planning.
You can find the reports in the Clinicals tab of the Report Library. You can use the Activate Reports page to activate these reports for your organization.
The following table outlines the goals and purpose of each report and the metric the report is designed to help track. You can filter these reports by payer, provider, department, and HCC (when applicable). We recommend running these reports on a regular basis to gain a better understanding of how well your organization is utilizing the features in athenaClinicals and documenting diagnoses on claims.
Note: The data in the Diagnosis Gaps dashboard is calculated in real time, whereas the data in the report is 1 day old. In some cases, the data in the dashboard and report may not match.
| Report name | Report output | Goal of report |
|---|---|---|
| Patient Risk Adjustment (HCC/RAF): Diagnosis Gaps report | List of patients and diagnosis gaps, by appointment date, department, and provider. | Assist with pre-visit planning by identifying documentation gaps prior to the patient being seen. |
| Patient Risk Adjustment (HCC/RAF): Open Diagnosis Gaps Report | List of patients with CMS-HCC diagnosis gaps in 'open' status. This report includes gaps both previously diagnosed and inferred from clinical evidence. | Identify open diagnosis gaps for patients with upcoming appointments to help your clinicians and staff prepare to address and document conditions that have not been addressed. |
| Patient Risk Adjustment (HCC/RAF): Addressed/Closed Diagnosis Gaps Report | List of patients with CMS-HCC diagnosis gaps in 'closed' status. This report includes gaps both previously diagnosed and inferred from clinical evidence. | Identify addressed diagnosis gaps for patients with upcoming appointments. |
| Patient Risk Adjustment (HCC/RAF): Dismissed Diagnosis Gaps Report | List of patients with CMS-HCC diagnosis gaps in 'dismissed' status. This report includes gaps both previously diagnosed and inferred from clinical evidence. | Identify dismissed diagnosis gaps for patients with upcoming appointments. Track gap dismissal actions to monitor progress of re-capturing CMS-HCC chronic conditions. |
| Patient Risk Adjustment (HCC/RAF): Re-diagnosis Progress report | Aggregates the total patients seen with a previous diagnosis of a chronic condition and the number of times the condition was successfully recaptured by provider, department, and HCC | Assess which chronic conditions are most successfully re-captured, as well as how successfully providers and/or departments are recapturing chronic conditions. |
| HCC Diagnosis Dismissal Report | List of diagnosis gaps that have been dismissed and by whom. | Track dismissals of diagnosis gaps across the organization. |
| HCC RAF GAP report | RAF and gap scores by patient. | Monitor trends of RAF and gap scores. |
Diagnosis gap data is also available for in-depth analysis via Data View.
For more details on Data View, see the Data View Documentation on the Success Community.
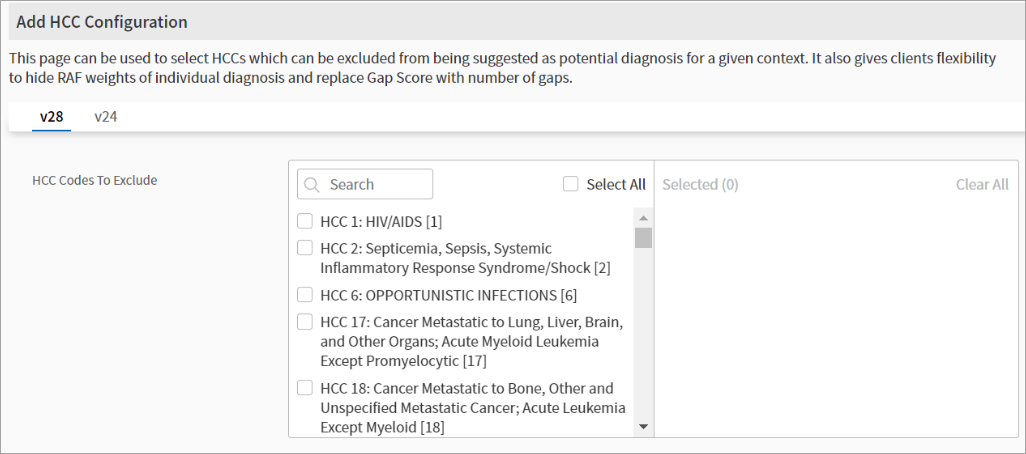
From the HCC Configuration page, your practice can manage and customize HCC-related configurations.
-
On the Main Menu, click Settings
 > Clinicals.
> Clinicals. -
In the left menu, under Practice Links — Other, click HCC Configuration.
From the v28 tab, you can view the v28 HCCs. From the HCC Codes to Exclude field, select the HCCs from the list that you want to exclude:
Tip: Hover over the image to see an expanded view.
When you’re finished with your selections, click Save.
The HCC Configuration page also supports the following configurations:
- Remove RAF weight from UI — This setting allows you to control whether the RAF weights for diagnoses are visible in athenaOne. Select this setting to remove RAF weights throughout the clinical workflow, including in the Diagnosis Gaps dashboard, A&P, Diagnoses & Orders cart, and Intake.
- CMS-HCC risk adjustment eligible diagnosis filtering for the past year claims — Select this setting to display only those diagnoses from the past year’s claims that are eligible for CMS-HCC risk adjustment.
For diagnoses from athenaOne claims to be considered for risk adjustment, the claim must meet the following criteria:
- Have at least one eligible CPT/HCPCS code. For more information, see the following CMS resource: Medicare Risk Adjustment Eligible CPT/HCPCS Codes).
- Have a supported place of service. For more details, see Supported places of service for HCC diagnosis gaps.
Note: Self-pay claims are not considered for risk adjustment.
As of April 2024, athenahealth's HCC engine supports claims from the following places of service:
| Place of service code | Place of service name |
|---|---|
|
01 |
PHARMACY |
|
02 |
TELEHEALTH – OTHER |
|
05 |
INDIAN HEALTH SERVICE FREE-STANDING FACILITY |
|
06 |
INDIAN HEALTH SERVICE PROVIDER-BASED FACILITY |
|
07 |
TRIBAL 638 FREE-STANDING FACILITY |
|
08 |
TRIBAL 638 PROVIDER-BASED FACILITY |
|
09 |
PRISON - CORRECTIONAL FACILITY |
|
10 |
TELEHEALTH - PATIENTS HOME |
|
11 |
OFFICE |
|
12 |
PATIENTS HOME |
|
13 |
ASSISTED LIVING |
|
14 |
GROUP HOME |
|
16 |
TEMPORARY LODGING |
|
17 |
WALK-IN RETAIL HEALTH CLINIC |
|
19 |
OFF CAMPUS-OUTPATIENT HOSPITAL |
|
20 |
URGENT CARE FACILITY |
|
21 |
INPATIENT HOSPITAL |
|
22 |
ON CAMPUS-OUTPATIENT HOSPITAL |
|
23 |
EMERGENCY ROOM |
|
24 |
AMBULATORY SURGICAL CENTER |
|
25 |
BIRTHING CENTER |
|
26 |
MILITARY TREATMENT FACILITY |
|
31 |
SKILLED NURSING FACILITY |
|
32 |
NURSING FACILITY |
|
50 |
FEDERALLY QUALIFIED HEALTH CENTER |
|
51 |
PSYCHIATRIC FACILITY - INPATIENT |
|
52 |
PSYCHIATRIC FACILITY - OUTPATIENT |
|
53 |
COMMUNITY MENTAL HEALTH CENTER |
|
58 |
NON-RESIDENTIAL OPIOID TREATMENT FACILITY |
|
61 |
COMPREHENSIVE INPATIENT REHABILITATION FACILITY |
|
62 |
COMPREHENSIVE OUTPATIENT REHABILITATION FACILITY |
|
71 |
STATE OR LOCAL PUBLIC HEALTH CLINIC |
|
72 |
RURAL HEALTH CLINIC |
Our reconciliation logic appropriately surfaces CMS-HCC gaps and non-CMS-HCC gaps to ensure the Diagnosis Gaps dashboard does not display previously closed diagnosis gaps or duplicate diagnoses from different sources or models.
See the following reconciliation logic details:
-
When athenaOne receives the same diagnosis attributed to different risk models, the diagnosis gap displays based on the following logic in the Diagnosis Gaps dashboard: CMS-HCC > HHS-HCC > CDPS.
-
When athenaOne receives the same diagnosis gap in different states (for example, closed and open), the displayed state in the Diagnosis Gaps dashboard is based on the following logic: CLOSED > DISMISSED > OPEN.
-
When athenaOne receives the same diagnosis as a clinically verified and inferred gap, the diagnosis displays as a clinically verified gap in the Previously Diagnosed section in the Diagnosis Gaps dashboard.
-
When athenaOne receives the same diagnosis from multiple sources, the displayed source in the Diagnosis Gaps dashboard is based on the following logic: MANUAL > CLAIM > EXTERNAL (payers and other third parties).
-
The Diagnosis Gaps dashboard also applies CMS-HCC Disease Hierarchy trumping logic. Within an HCC, we only display the higher specific HCC and one ICD-10 code. ICD-10 codes in two HCCs in the CMS-HCC model display the HCC with the higher RAF weight.
See the following table for various scenarios and the logic rules and details:
| Scenario | Display logic rules | Display logic details |
|---|---|---|
| Multiple diagnoses | Diagnoses in multiple states | When athenaOne receives the same diagnosis in different states (for example, closed and open), the displayed state in the Diagnosis Gaps dashboard is based on the following logic: CLOSED > DISMISSED > OPEN. |
| Different types of gaps | When athenaOne receives the same diagnosis as a clinically verified and clinically inferred diagnosis gap, the diagnosis displays in the Previously Diagnosed section in the Diagnosis Gaps dashboard. | |
| Diagnoses from different sources | When athenaOne receives the same diagnosis from multiple sources, the displayed source in the Diagnosis Gaps dashboard is based on the following logic: MANUAL > CLAIM > EXTERNAL (payers and other third parties). | |
| Diagnoses from multiple models | When athenaOne receives the same diagnosis attributed to different risk models, the diagnosis gap will display model details using the following hierarchy logic in the Diagnosis Gaps dashboard: CMS-HCC > HHS-HCC > CDPS. | |
| Multiple diagnoses within the same HCC | When athenaOne receives two different ICD-10 codes within the same HCC category, the Diagnosis Gaps dashboard lists each ICD-10 code as a separate gap in the Previously Diagnosed section. | |
| Multiple diagnoses from the same source |
When athenaOne receives the same diagnosis multiple times from the same sources, the displayed source in the Diagnosis Gaps dashboard is based on the following logic:
|
|
| ICD-10 codes that map to multiple HCCs | Display a single HCC for an ICD-10 code |
The Diagnosis Gaps dashboard displays the higher specific HCC for a diagnosis. ICD-10 codes associated with two HCCs in the CMS-HCC model display the HCC with the higher RAF weight. For example, for the E13.3411 ICD-10 code, the Diagnosis Gaps dashboard will display only HCC 298 – Severe Diabetic Eye Disease, Retinal Vein Occlusion, and Vitreous Hemorrhage (RAF weight 0.336), even though the code also maps to HCC 37 – Diabetes with Chronic Complications (RAF weight 0.166).
Note: In 2025, we plan to display all relevant HCCs for an ICD-10 code within the Diagnosis Gaps dashboard (meaning we would display both HCC 298 and HCC 37 for E13.3411 in the Previously Diagnosed section). However, we will continue to follow the CMS-HCC model and show only the higher HCC as closed. |
| CMS-HCC hierarchy rules | Disease hierarchy logic |
We follow the CMS-HCC hierarchy/trumping logic where the Diagnosis Gaps dashboard displays only the ICD-10 codes for the higher severity HCC within a disease hierarchy and model version. For example, the Diagnosis Gaps dashboard displays the ICD-10 code for HCC 138 v28 over an ICD-10 code for HCC 137 v28
We consider the HCC as closed for the year if one ICD-10 code within the category is submitted on a claim. |
| HCC configuration rules | HCC exclusions | If an HCC is excluded on the HCC Configuration clinicals admin page (Settings  > Clinicals > HCC Configuration), any diagnoses associated with that HCC do not display for recapture in the Diagnosis Gaps dashboard. > Clinicals > HCC Configuration), any diagnoses associated with that HCC do not display for recapture in the Diagnosis Gaps dashboard. |
Providers can reinstate dismissed diagnosis gaps as open gaps. If no action is taken to reinstate a dismissed diagnosis gap, the gap remains in the dismissed state for various periods of time depending on the source of the gap.
See the following table for more details:
| Source of the gap | Retention period in dismissed state | Post-retention period |
|---|---|---|
| Claim | 3 calendar years (until December 31 of the third year) |
|
| Manual | 2 calendar years (until December 31 of the second year) |
|
| External (payers or any gaps that come in through the Risk Gaps API) | 1 calendar year (until December 31 of the first year) |
|
A provider can dismiss a diagnosis gap if that clinical condition is found to be irrelevant for the patient. Dismissed diagnosis gaps appear in the Dismissed tab of the Diagnosis Gaps dashboard. If the dismissed condition is later found to be relevant for the patient, the provider can reinstate the diagnosis gap as an open gap by clicking ![]() Undismiss or by manually adding that diagnosis in the Diagnosis Gaps dashboard.
Undismiss or by manually adding that diagnosis in the Diagnosis Gaps dashboard.
While a diagnosis gap (clinically verified or inferred) is considered dismissed, the Diagnosis Gaps dashboard can receive the same gap from multiple sources. The system behavior in each of these scenarios is detailed in the following table:
| Current gap state | Action | System behavior |
|---|---|---|
| A clinically verified diagnosis gap (ICD-10 code of v28) is dismissed | A user adds the same ICD-10 code (v28) manually | The diagnosis gap (ICD-10 code of v28) is reinstated as a clinically verified gap |
| A clinically verified diagnosis gap (ICD-10 code of v28) is dismissed | The same ICD-10 is received on a past year claim that is updated now or received from athenahealth Population Health | The clinically verified diagnosis gap (ICD-10 code of v28) remains dismissed |
| A clinically verified diagnosis gap (ICD-10 code of v28) is dismissed | An external source (payer) sends the same ICD-10 code (v28) through the Risk Gaps API | The clinically verified diagnosis gap (ICD-10 code of v28) remains dismissed |
| A clinically verified diagnosis gap (ICD-10 code of v28) is dismissed | The same ICD-10 code is received in a current year athenahealth claim |
|
| A clinically verified diagnosis gap (ICD-10 code of v28) is dismissed | An ICD-10 code of the same HCC (v28) is received in a current year athenahealth claim |
|
| A clinically inferred diagnosis gap without an ICD-10 code (HCC of v28) is dismissed. | A user adds an ICD-10 code of the same HCC (v28) manually |
|
| A clinically inferred diagnosis gap without an ICD-10 code (HCC of v28) is dismissed | An ICD-10 code of the same HCC (v28) is received on a past year claim that is updated now or received from athenahealth Population Health |
|
| A clinically inferred diagnosis gap without an ICD-10 code (HCC of v28) is dismissed | An external source (payer) sends an ICD-10 code of the same HCC (v28) through the Risk Gaps API |
|
| A clinically inferred diagnosis gap without an ICD-10 code (HCC of v28) is dismissed | An external source (payer) sends a clinically inferred diagnosis gap of the same HCC (v28) through the Risk Gaps API |
Note: This behavior occurs if the external gap is sent by the same payer or a different payer, and there is a change in the clinical evidence. If the evidence is the same and the payer is also same, the dismissed clinically inferred diagnosis gap remains dismissed. |