User Guide — Payer-Provided Eligibility Details FAQ
User Guide — Payer-Provided Eligibility Details FAQ
This page lists questions and answers about eligibility checks and the Payer-Provided Eligibility Details page.
In order to display a patient’s eligibility, athenaOne sends an eligibility request to a clearinghouse or payer. That entity will return eligibility details in what’s called a ‘271 response.’ athenaOne in turn displays what is received from the payer in the 271 response on the Service Types tab of the Payer-Provided Eligibility Details page, where we display cost sharing elements per Service Type. If data appears to be missing from the eligibility response, this can most likely be attributed to the omission of that information in the payer’s response.
At times, a payer’s eligibility system, or athenaOne’s connection with a payer, can experience downtime. This is uncommon but will surface in athenaOne as the eligibility status being ‘unavailable’.
- If this occurs, we recommend that you re-check eligibility after a few minutes.
- If the issue persists for a longer period of time, please contact athenahealth for next steps from athenaOne > Support > Success Community > Contact Client Support Center.
athenaOne performs several automated eligibility checks, including at the creation/update of an insurance package, 1-5 days prior to an appointment date, and when a claim is created.
When we do this, we request Service Type Category 30 (Plan Coverage and General Benefits). Typically, a payer will respond to this “generic” request with an array of eligibility benefits , which may or may not contain the Service Type information you need. If this is the case, there are two options we recommend:
- Perform a custom eligibility check — This targeted request may provide you with the exact Service Type information you need. See this O-help topic for details: Perform a custom eligibility check.
- If the payer still does not return the eligibility information you need in the custom check, we recommend that you call the payer directly.
With the custom eligibility check feature (released in Summer 2023), you can check eligibility for a specific date of service (past, present, or future – depending on existing limitations by payer) and review that information on the Payer-Provided Eligibility Details page.
Yes, as long as you are requesting a Service Type Code from the standard list in the Health Care Eligibility Benefit Inquiry and Response (270/271) implementation guide.
Note: athenaOne will not always receive a response to the requested Service Type from the payer.
On the Payer-Provided Eligibility Details page, athenaOne will display eligibility data for every service type received in the payer response. You can select frequently used Service Types as your "favorites" for easier access.
- Click the star on the left side of the Service Type header to add/remove that service type from the My Favorite Service Types section in the left pane.
- Favorites appear at the top of the Service Types list in the left pane. As long as we receive data for a given Service Type Category from the payer, your Favorite categories will also display at the top of the scrollable list of eligibility information in the main pane.
On the Payer-Provided Eligibility Details page, select the Eligibility History tab and search for your Date of Service.
- Each eligibility check will store the username of the person who initiated it.
- For custom eligibility checks, the username will be followed by ‘Custom’ and then an industry standard abbreviation representing the Service Type Category (STC) requested in the custom check.
- You can hover your cursor over the STC abbreviation for the full Service Type name. If this abbreviation corresponds to one of the values under the Service Types Received column, you will know that the payer returned the requested eligibility benefits for that custom check.
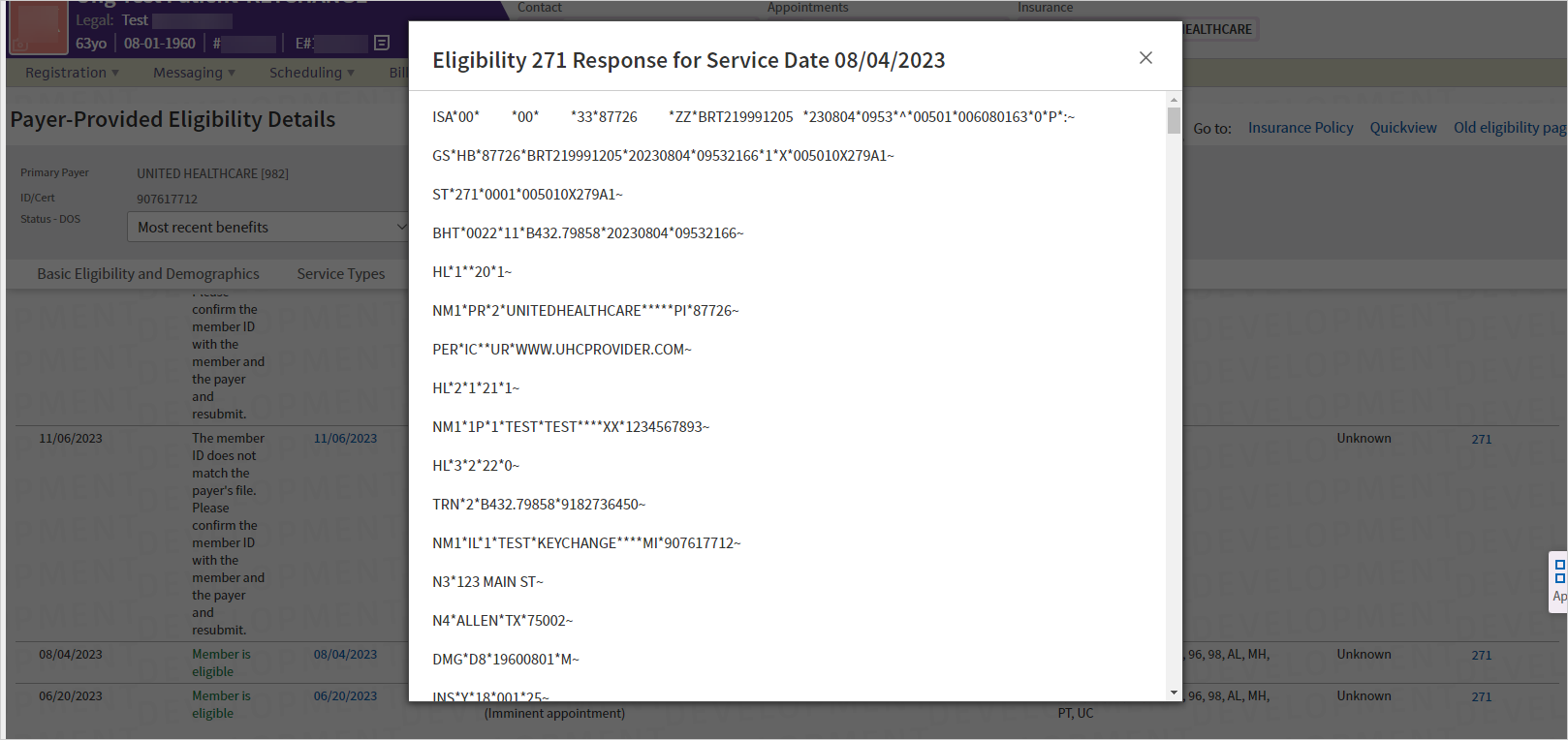
If you’re seeing something like in the screenshot below, it means you’ve accessed the 270 request or 271 response raw file.
Tip: Hover over the image to see an expanded view
This format exists mainly for the use of computers and billing/insurance experts. We display the information in a human-readable format within the Service Types tab of the Payer-Provided Eligibility Details page.
Close the pop-up window that has the computer code.
From the Eligibility History tab, click the link for the date of service you want to see. You’ll be brought directly to the corresponding DOS in the Service Types tab where all of this computer code is presented in a more legible format that can be easily understood.
There are two typical causes for this:
- If you have never had access to eligibility data: You may not have the correct permissions to view eligibility responses. Your practice manager or CSM will be able to grant these to you.
-
If you have previously had access to eligibility data: You may have clicked on the ‘Go to: Old eligibility page’ link from the new Payer-Provided Eligibility Details page. When you click on that link, athenaOne remembers that as your preference and will default you to whichever page (the new or the old) that you last chose to use. Click on the link as seen below to return to the new experience:
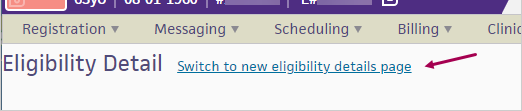
You can continue to use the legacy eligibility pages as we continue developing the new page to ensure it has all the functionality you need. We encourage you to try the new page, which has additional data fields and new features in a streamlined experience.
We’ll communicate with you in advance before we deprecate the legacy experience in Fall 2024.
The new Payer-Provided Eligibility Details page is a part of our overall modernization of Eligibility, part of which will address performance and promises significant gains in speed and stability. Thank you for your patience and continued use of the new custom eligibility check feature and revamped Eligibility Details page!
Check out the Ideas page on the Success Community to provide feedback or thoughts about how to improve this functionality.