Payer-Provided Eligibility Details
On the Payer-Provided Eligibility Details page, you can:
- Verify a patient's insurance eligibility for participating insurance plans, for various dates of service.
-
Resolve eligibility demographics conflicts that occur when the information on file in your practice is different from the payer's information.
-
View benefit coverage details received from the payer, organized by their associated Service Type.
-
View the detailed history of electronic eligibility checks for a patient.
The athenaOne system retrieves eligibility information from insurance carriers that provide eligibility information electronically whenever the payer sends it to us via the ANSI standard transaction.
Use the Payer-Provided Eligibility Details page header and tabs to view eligibility details.
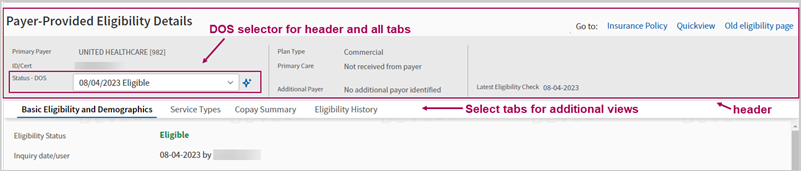
Header — stays visible as you scroll down or select various tabs:
- Displays general policy information and recent eligibility status and details.
- Status - DOS — Select a Date of Service and the entire page (including the header and all tabs on the page) will update with eligibility details for the selected date. The default DOS is Most recent benefits.
- Go to — Click a link to go to Insurance Policy, Quickview, or Old eligibility page.
Tabs — multiple views:
- Basic Eligibility and Demographics — View general plan details and eligibility status for the selected date. View Subscriber and Patient demographic information from the payer, any demographic differences detected, and make updates in athenaOne if needed.
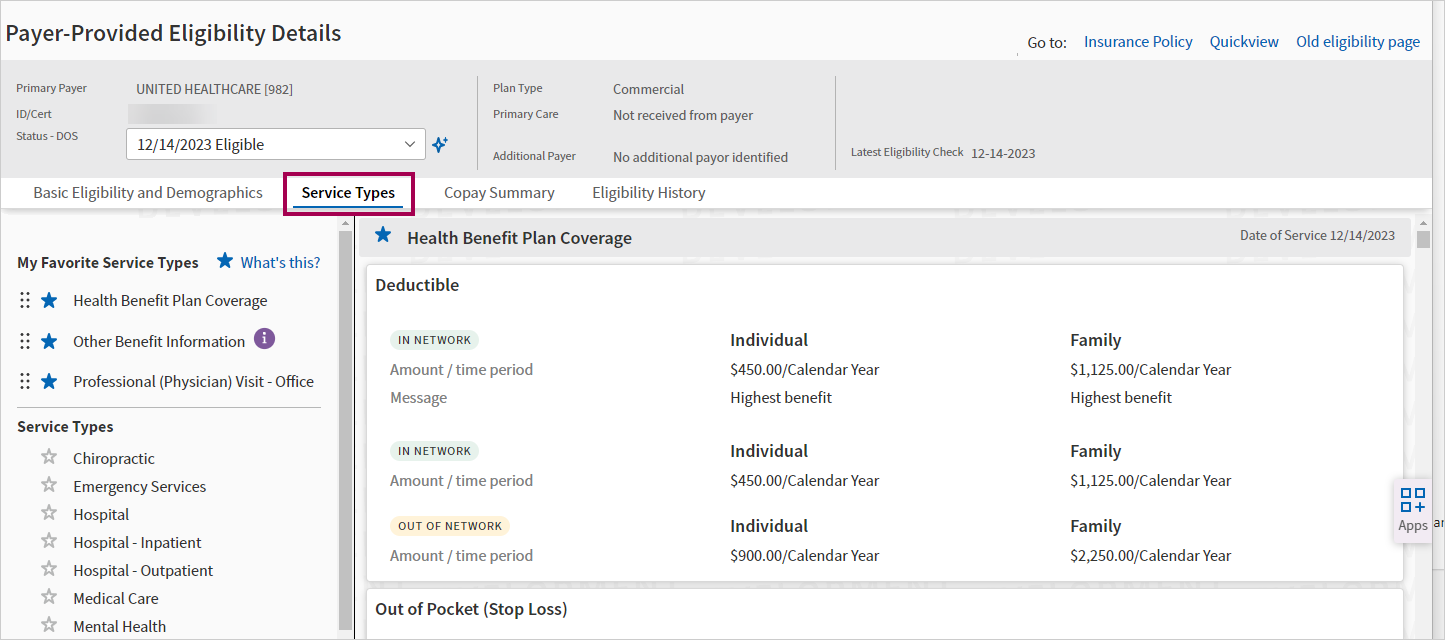
- Service Types — View the benefit coverage details received from the payer, organized by Service Type. Select "favorite" service types for easier access.
- Copay Summary — Find patient copay details more easily. Note: The copay information will still also be in the Service Types tab along with other benefit coverage details.
- Eligibility History — View the history of eligibility checks for the patient and details from each check.
For an overview video of this feature, click here:
Multiple entry points:
- On the Patient Actions Bar, click Registration, and then click Check Eligibility. If the patient has only one policy registered in athenaOne, the Payer-Provided Eligibility Details page appears.
- On the Quickview page, under the Insurances heading, click View eligibility detail and history.
- On the Quickview page, under the Insurances heading, click Perform custom eligibility check and then select the options for the custom check.
- On the Add/Update Policy Details page, click View eligibility detail and history (next to the Last eligibility message at the top).
- On the Add/Update Policy Details page, click Update & Perform Eligibility Check in the Eligibility section.
You can perform an eligibility check as follows:
- On the Quickview page (Insurances section), click the Perform eligibility check link under the specific policy.
- On the Update Policy Details page, click Update & Perform Eligibility Check.
The Payer-Provided Eligibility Details page appears with the current results for the policy.
-
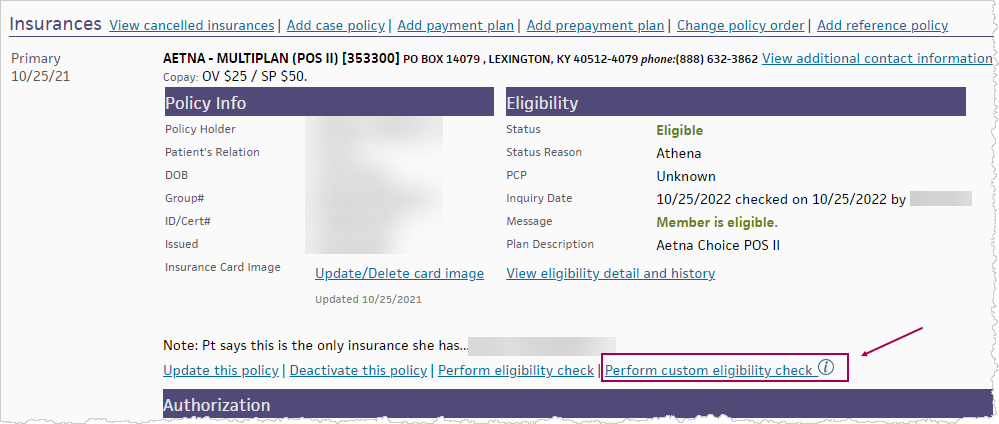
Display the Quickview page for a patient.
-
In the Insurances section, for a specific policy, click the Perform custom eligibility check link.
- This link is only available if you're using the enhanced Payer-Provided Eligibility Details page (released in Summer 2023).
- If you were using the enhanced page and then chose Go to: Old eligibility page, this link will not be visible.
The Perform Custom Eligibility Check window appears.
-
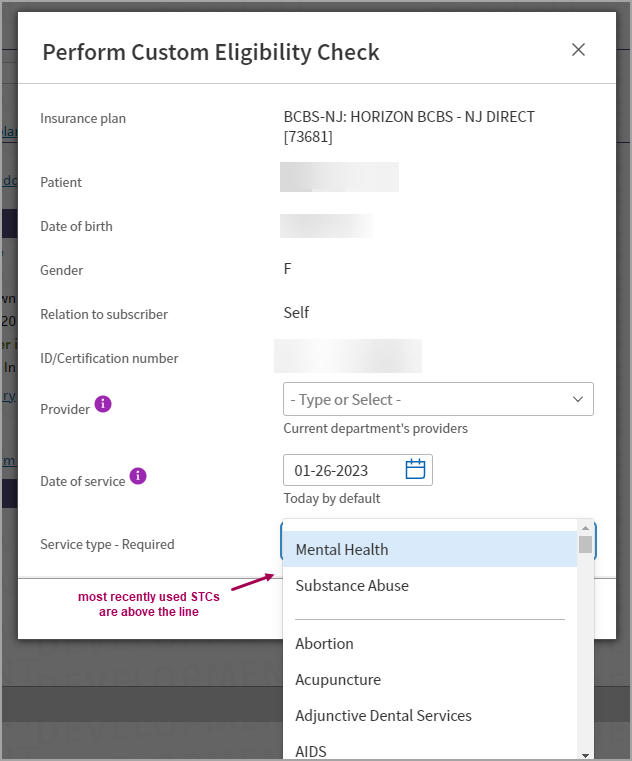
Select the details for the custom eligibility check:
- Provider — (optional) - Select a Provider.
- This list only shows the Providers within the department that you're currently logged into.
- To select a provider from another department, log into that department. If you don't select a provider, the system will choose one based on the patient's previous appointment and claims.
- Date of Service — (Today's date defaults) Select a Date of Service.
- Most payers will accept a prior or future date, but payer rules vary. Some payers may not return benefit details for dates before the current year or in the future.
- Service Type — Select a Service Type Code (STC) from the list. The most recently used STCs appear above the line in the menu.
STCs are industry standard codes that payers and clearinghouses use to specify what eligibility is being requested.
- Provider — (optional) - Select a Provider.
-
Click Check Eligibility.
-
If the STC requested does not match the STC returned:
- A message appears: "Payer Returned Different Benefits", with details of the STC(s) requested and the STC(s) returned.
-
Click View Benefits to see the returned benefits
or
-
Click Perform New Check to run a new custom check
- The Payer-Provided Eligibility Details page appears, displaying the Service Types tab with the payer's response for the STC(s) you requested.
Important: When you manually check eligibility, wait 20 seconds for a response from the payer (or an error message) before you attempt to check eligibility again.
- Check the latest eligibility information retrieved from the payer from one of the following:
- On the Quickview page (Insurances section), click the View eligibility detail and history link under the specific policy.
-
On the Update Policy Details page, click the View eligibility detail and history link next to the Last eligibility message field.
The Payer-Provided Eligibility Details page appears.
- Status - DOS — Select a Date of Service and the entire page (including the header and all tabs on the page) will update with eligibility details for the selected date. The default DOS is Most recent benefits.
- On the Quickview page, under the Insurances heading, click View eligibility detail and history.
The Payer-Provided Eligibility Details page appears.
- Status - DOS — Select a Date of Service and the entire page (including the header and all tabs on the page) will update with eligibility details for the selected date. The default DOS is Most recent benefits.
- Or, select the Eligibility History tab and view eligibility details for prior eligibility checks based on Inquiry Date or Date of Service.
Note: If there are eligibility conflicts, a warning message appears on the Quickview:
Demographics conflict: Click view detail to resolve.
- Review the list of conflicts listed in red.
- Click
Update in athenaOne to update an individual
item, or click Update All in athenaOne to update all
the conflicting data items. A dialog box appears: "Are you sure that you
want to update this policy?"
Note: The Update buttons on the Eligibility Details page synchronize patient demographic information between the practice and the insurance company for the insurance policy only. The Update buttons do not update the patient data on the Quickview, Patient Registration, or other athenaOne page. - Click OK to update the conflicting values on the policy.
- On the Quickview page, under the Insurances heading, click View eligibility detail and history.The Payer-Provided Eligibility Details page appears.
-
Status - DOS — Select a Date of Service and the entire page (including the header and all tabs on the page) will update with eligibility details for the selected date. The default DOS is Most recent benefits.
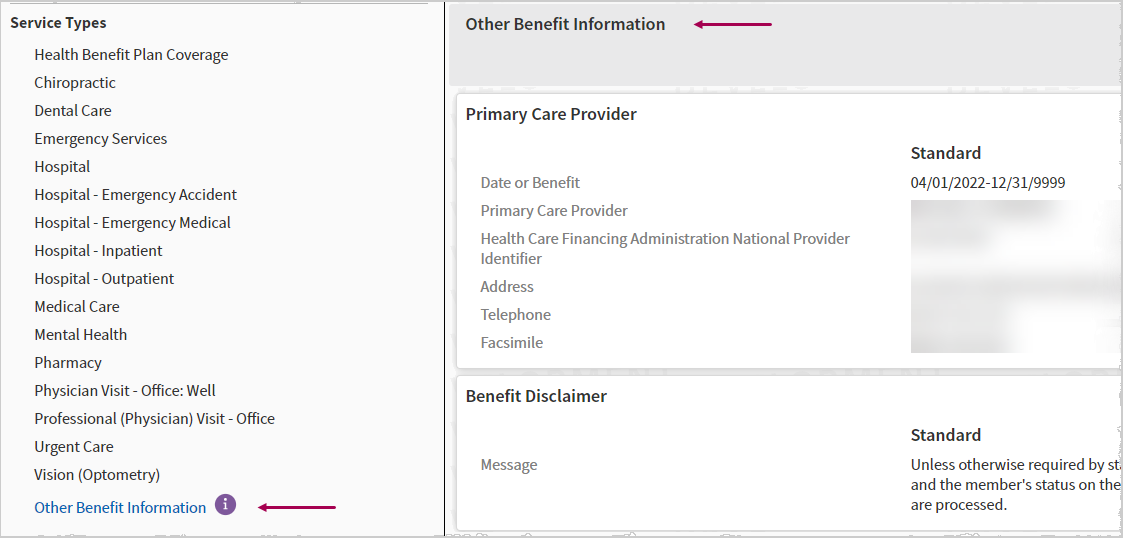
- Select the Service Types tab.
-
Select a service type from the My Favorite Service Types section or Service Types section on the left.
-
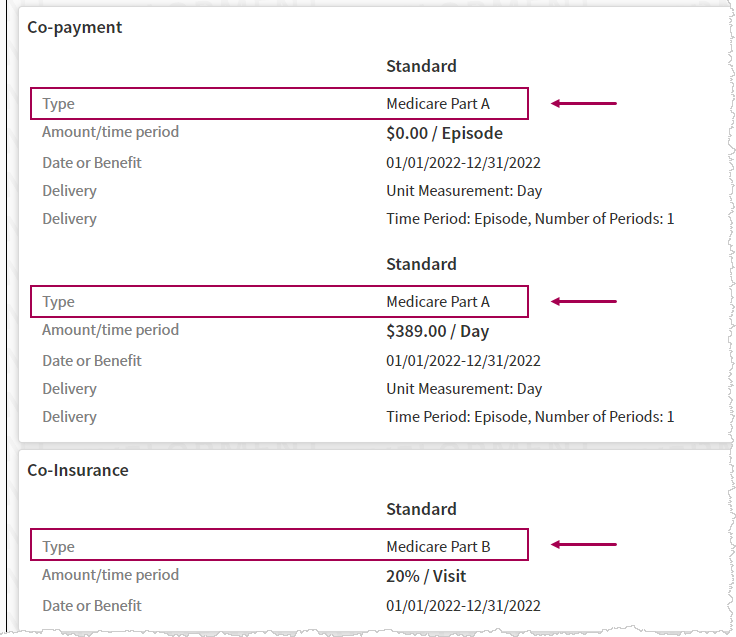
Review the benefit coverage details (such as Co-payment, Co-Insurance, Deductible) received from the Payer.
- If you have Favorites selected, they appear at the top of the service type list in the left pane and at the top of the service benefit details in the main pane.
-
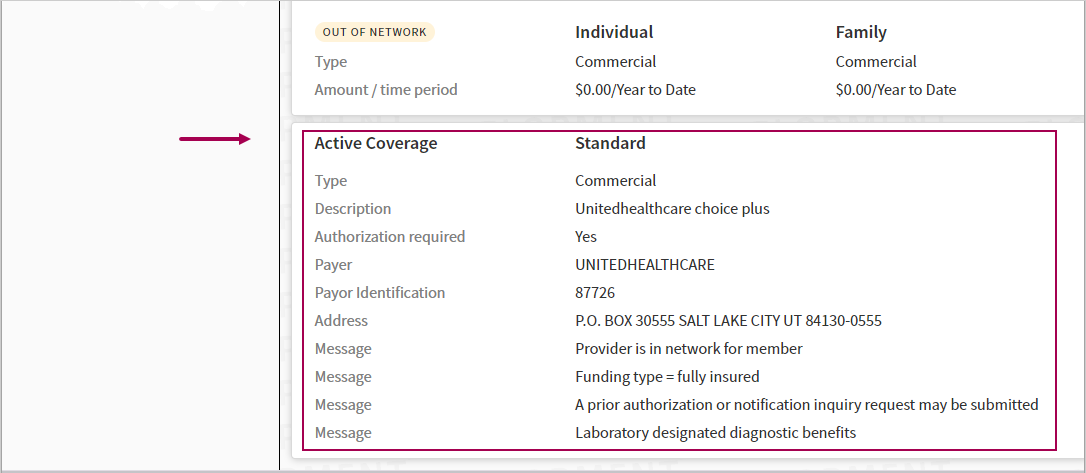
Active Coverage — Active Coverage benefit information appears for the service type if available.
Other Benefit Information — This Service Type consolidates and displays benefit information which is not specific to any service type.
-
Medicare benefit type — The Medicare benefit type appears in applicable service types.
- On the Quickview page, under the Insurances heading, click View eligibility detail and history.The Payer-Provided Eligibility Details page appears.
Status - DOS — Select a Date of Service and the entire page (including the header and all tabs on the page) will update with eligibility details for the selected date. The default DOS is Most recent benefits.
- Select the Copay Summary tab.
- Check the eligibility information retrieved from the payer from one of the following:
- On the Quickview page (Insurances section), click the View eligibility detail and history link under the specific policy.
-
On the Update Policy Details page, click the View eligibility detail and history link next to the Last eligibility message field.
The Payer-Provided Eligibility Details page appears.
- Status - DOS — Select a Date of Service and the entire page (including the header and all tabs on the page) will update with eligibility details for the selected date. The default DOS is Most recent benefits.
- Select the Eligibility History tab.
Electronic eligibility check results reflect payer data at the time of the electronic query. The results do not take into account the date of service of the appointment.
Note: If the enrollment status for the provider is set to any status other than COMPLETE, the eligibility transaction is not sent and the following error is returned when eligibility is automatically or manually checked: "This provider is not enrolled for electronic eligibility checking."
The athenaOne system formats and displays whatever information we receive from the payer. If the payer's electronic eligibility file contains formatting or data errors, these anomalies also appear on the Payer-Provided Eligibility Details page.
Note: Most payers use the ANSI standard for eligibility transactions; athenaOne provides expanded benefit information whenever the payer sends the ANSI standard transaction.
athenahealth has a dedicated team that works to establish electronic eligibility checking for as many payers as possible. However, athenahealth can provide electronic eligibility checking only for payers that are willing and able to make this information available to us electronically.
After we establish electronic eligibility checking for a payer, it is important to understand that:
- athenahealth has no control over the availability of the payer's electronic eligibility system.
- athenahealth has no control over the accuracy of the electronic eligibility information that the payer transmits.
In other words, the availability and accuracy of our electronic eligibility checking depends on the availability and accuracy of each payer's system. athenahealth actively tracks payer status and helps payers improve the availability and accuracy of the information they do provide.
In spite of our best efforts to increase our payer coverage and the reliability of this information, a payer may deny a claim even when athenaOne receives a "Member is eligible" response from the payer.
- "Member is eligible" indicates that the patient is on file at the payer with active coverage, but it does not guarantee that a given claim will be paid.
- Benefit coverage depends on the type of service, provider network status, and patient classification on the policy.
- Eligibility information must be applied correctly to a patient encounter to effectively prevent a denial.
Refer to Eligibility Verification to view the current list of payers that have electronic eligibility checking enabled with athenahealth.
The results of the most recent eligibility check information appear on the patient's Quickview page to indicate whether a patient is insured for the date of service; copayment information or restrictions are also usually supplied in the eligibility message.
When a patient's eligibility is checked electronically, these fields on the Add /Update Policy Details page are updated: Eligible status, Last inquiry, and Last eligibility message.
From the Workflow Dashboard, you can click a linked number in the Eligibility column to access the Eligibility Worklist for that department (in the Task Bar). The worklist provides appointment date, patient name, and a link to the patient's Quickview page for each patient on the list.
The Eligibility and Phone page also provides you with information about patient eligibility (On the Main Menu, click Calendar. Under APPOINTMENTS, click Eligibility and Phone List).
You can select frequently used Service Types as your "favorites" for easier access:
- Favorites appear at the top of the service type list in the left pane and at the top of the service benefit details in the main pane.
- Click the star on the left side of the Service Type header to add/remove that service type from the My Favorite Service Types section in the left pane.
- In the My Favorite Service Types section, click and drag Service Types to reorder the list.
To see benefit coverage details for specific service types or for a specific date of service, you can manually run a custom eligibility check.
Important: For customers with multiple provider groups, please note that the eligibility details are currently bounded per Provider Group.
- If you are logged into a specific Provider Group — You will NOT see eligibility information that was requested for that patient from a different Provider group. You will only see eligibility information that was requested from departments within the Provider Group that you are logged into.
- We are working to expand this functionality so that you will see eligibility information across Provider Groups if those Provider Groups share a Chart Group. Providers may choose to review and update their Chart Group settings/permissions in athenaOne if they deem it appropriate to segment sensitive patient information.
- This is consistent with how access to patient data across Provider Groups is determined based on Chart Group configuration, to ensure patient data safety/privacy.
The information provided via electronic eligibility checking can vary from payer to payer, and even from patient to patient, based on the individual policy details.
| Payer-Provided Eligibility Details — header | |
|---|---|
| Primary Payer | Primary Payer name |
| ID/Cert | Member ID/certification number on the policy |
| Status - DOS |
Status — Message result of the eligibility check (for example, Eligible).
Date of Service — Select a Date of Service and the entire page (including the header and all tabs on the page) will update with eligibility details for the selected date. The default DOS is Most recent benefits. |
| Plan Type | Plan type returned in the eligibility check. |
| Primary Care | Primary care physician returned in the eligibility check. |
| Additional Payer | Addtional payer returned in the eligibility check. |
| Last Eligibility Check |
Date of most recent conclusive eligibility check. (The following responses are considered conclusive: Eligible, ineligible, patient not found) |
| Go to: |
Click a link to go to the athenaOne page:
|
| Basic Eligibility and Demographics tab | |
| Eligibility Status | Message result of the eligibility check (for example, Eligible) |
| Inquiry date/user | The date and username for the eligibility check, or the event that triggered an automated check. |
| Date of Service | The Date of Service for the eligibility check. |
| ID/Certification Number | Member ID/certification number on the policy |
| Policy/Group Number | Group/policy number on the policy. |
| PCP | Primary care physician returned in the eligibility check |
| Payer Disclaimer |
Standard benefit disclaimer message. This field appears only for eligible and ineligible responses. |
| Patient/Subscriber Differences section | |
|
|
athenaOne compares the information returned by the payer to the demographic information on file in athenaOne. Any discrepancies are listed in red in this section.
These discrepancies appear for "eligible" responses only. A row appears in this section if the following conditions are true:
Values in athenaOne that conflict with the data returned are displayed in red with instructions to correct them on the Add/Update Policy Details page. |
| Payer Subscriber/Patient Demographic Information section | |
|
Subscriber Details |
This section displays any subscriber or patient demographic information received in the eligibility response from the payer. |
| Patient Details | |
| Service Types tab | |
|---|---|
| My Favorite Service Types |
Choose your favorite Service Types for easy access:
|
| Service Types (left pane) |
The benefit service types returned by the payer in the eligibility check. If no benefit information was supplied by the payer for a category, that heading does not appear.
Click a Service Type in the left pane to see benefit coverage details for that service type in the main pane. |
| Service Types — Benefit Details (main pane) | |
| Service Type | The benefit type of service |
|
Benefit Coverage Type |
The type of benefit coverage, such as Co-payment, Co-Insurance, Deductible, Limitations |
| Benefit coverage details |
Each benefit coverage type displays the following details if available:
|
| Copay Summary tab | |
| Service Type |
The Service Type for benefit coverage. Note: The ordering of Service Types listed within the Copay Summary tab will reflect the "favorites" you selected on the Service Types tab. |
| Copay | The copay amount (per Visit or per Day) for the service type. |
| Network | The provider's network status (In, Out, Either). |
| Payer Messages | Messages returned by the payer in the eligibility response, if any. |
| Date of Service |
The date of service for the eligibility check. Use the Status - DOS selector in the header to see copay summary for another date of service. |
| Eligibility History tab | |
| Inquiry Date | The date that the eligibility check was performed. |
| Result | The result of the eligibility check. |
| Date of Service |
The Date of Service for the eligibility check. Click a linked date to see a date-filtered view of additional details on the Service Types tab. |
| Checked by |
The username of the person who performed the eligibility check, or the event that triggered an automated check (for example, an upcoming appointment).
For custom eligibility checks, this column shows the Service Type requested. |
| Provider | The Provider received from the payer in the eligibility response. |
| Subscriber ID | The Subscriber ID received from the payer in the eligibility response. |
| Outgoing Request | Click the link to see the detailed Eligibility 270 Request in ANSI X12 format. |
| Service Type Received |
The Service Type(s) received from the payer in the eligibility response.
Tip: Hover your cursor over a Service Type code to see the service type description. For a list of standard Service Type codes and descriptions, see the X12 Service Type Codes website. |
| Primary Care Provider | The PCP received from the payer in the eligibility response. |
| Incoming Response | Click the link to see the detailed Eligibility 271 Response in ANSI X12 format. |