 User Guide — Request Proof of Timely Filing
User Guide — Request Proof of Timely Filing
If your practice is a no-posting or no-follow-up athenaCollector practice, you can request proof of timely filing.
- Verify that you submitted the claim electronically at least once by checking that it is listed as ANSI837 in the Bills mailed section of the Claim Edit page.
Note: If you submitted the claim only on paper, athenahealth cannot provide a clearinghouse report. - Display the Claim Edit page. You can click the Go to Advanced View link on the Claim Action page.
In the Claim Details section, under Insurance
- Force drop to paper for primary — Select Yes-Athena.
- Reason: — Select CSTPRFSUBM.
In the Add Note section (at the bottom of the page)
- Status — Select DROP.
- Kick reason — Enter DRPBILLING.
- Click Save.
The claim moves into ATHENAHOLD status.
athenahealth runs a daily report to identify claims denied for timely filing; we research each claim and attach the appropriate clearinghouse report. These claims are re-dropped to print with the attachment, which athenahealth forwards to your correspondence address.
Tip: After the clearinghouse report is attached to the claim, it appears in the Manage Attachments sections of the claim.
When primary or secondary payers deny claims for timely filing, the denial is indicated by the athenahealth kick code BDE (Billing Deadline Exceeded) in the claim note history on the Claim Action and Claim Edit pages. The filing deadline for claims is specific to each insurance package (you can find the filing deadline on the Phone Payer Information page).
athenhealth proves timely filing using one of the following methods in the order shown.
Note: If a claim was submitted to the payer after the timely filing limit or if none of the following proofs are available, the claim is moved to your responsibility with the kick reason FWRFILINGLIMIT.
- USPS One Code confirmation (Paper claim delivery confirmation)
The delivery date used for USPS One Code confirmation is based on the date that the claim arrived at the USPS sorting facility nearest to the payer location.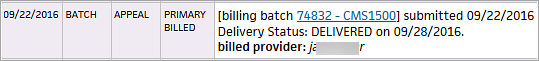
-
ACK PAYOR report (electronic claim delivery confirmation)
Payers that accept electronic claims send an acknowledgment report to inform athenahealth that the claim was received.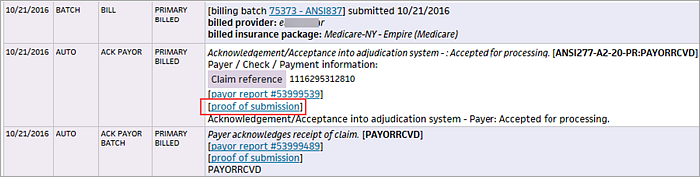
- EOB from a timely submission
- EOB for another payer
- Screenshots of billing event
This method is used only if none of the previous options are available. - Patient billing statement
This method is used only if none of the previous options are available.