Claim Edit
This page allows you to edit fields on a claim, so that you can correct errors and provide missing information needed to achieve DROP status. The claim number always appears at the top of the page, and the page header is fixed to the top of the page when you scroll.
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
Click the Go to Advanced View link on the Claim Action page
Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view)
On the Patient Actions Bar, click Billing, and then click Post Payment. On the Post Payment page, click edit claim (the link is on the line item's advanced view)
To edit claim information, you need both of these user permissions:
- Claim Edit Pages — This user permission provides view access to pages used to edit claims.
- Edit Claims — This user permission provides view access to pages used to edit claims and allows the user to add, edit, and delete information on a claim.
To change payers on a claim or to void claims, you also need the Void Charges and Transactions role.
Several user roles are associated with voiding transactions. These roles give your practice administrators more control over voiding permissions.
The Void Charges and Transactions role includes these permissions:
- Void Charges
- Void Collect Adjustments
- Void Own TOS Payments
- Void Transactions
- Onboarding Dashboard
- Live Benchmarks Access
- Messaging, user, and practice pages
- View Invoices
- EDIT SCHEDULES
- EDITBILLINGADMIN
- EDITDEMOGRAPHICS
- Research Menu
- Workflow Dashboard Access
The Void Transactions role includes these permissions:
- Void Collect Adjustments
- Void Own TOS Payments
- Void Transactions
- Onboarding Dashboard
- Live Benchmarks Access
- Messaging, user, and practice pages
- View Invoices
- EDIT SCHEDULES
- EDITBILLINGADMIN
- EDITDEMOGRAPHICS
- Research Menu
- Workflow Dashboard Access
The Void Transactions (excluding Collect Adjustments) role includes all permissions included in Void Transactions, excluding the permission to void collect adjustments, allowing you to designate certain users who can void transactions in general but not collect adjustments. The Void Transactions (excluding Collect Adjustments) role includes these permissions:
- Void Own TOS Payments
- Void Transactions
- Onboarding Dashboard
- Live Benchmarks Access
- Messaging, user, and practice pages
- View Invoices
- EDIT SCHEDULES
- EDITBILLINGADMIN
- EDITDEMOGRAPHICS
- Research Menu
- Workflow Dashboard Access
These instructions apply for claims that have not been billed (sent to the payer for the first time). For information about editing denied claims, see How to Correct Claims in Hold Queues.
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view).
- Review the information under Claim Notes (at the bottom of the page).
- Kick/Scrub/Note — Make the necessary changes by following the instructions in the bottom row of the Claim Notes. Refer to the Claim Status page for more information about claim status.
- Claim Status — Change claim status to DROP (optional — athenaOne automatically re-scrubs the claim and resets the status when you click Save Claim)).
- Note — Enter a note to summarize the edits you made. (athenaOne requires you to enter a note or enter a kick reason when you set the status to DROP, and prompts you if you forget.)
- Click Save Claim. The claim is "scrubbed" and the Claim Review page appears.
- Verify that the claim is in DROP status. If it is not, click the edit claim link and repeat this process until the claim is in DROP status.
Note: When a claim error is corrected, athenaOne automatically updates the claim status to reflect the correction as soon as the claim is next scrubbed or viewed.
When you edit a claim with transactions posted prior to the system close date, athenaOne transparently voids and re-creates the entire claim if any of the following fields are updated:
- Primary/Secondary Insurance
- Provider/Supervising Provider
- Procedure
- Service Dept/Patient Dept
- Charge Amount
Because the claim has been voided and re-created, the post date is changed to the current date.
Note: At least one change must be made to the claim before it can be resubmitted. It is not compliant to resubmit a claim without changes only to see whether the claim will be paid if you resubmit it to the payer.
- Display the Claim Edit page for the claim that you want to re-drop. Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view).
- Scroll down to the Add Note section.
- Applies to — Make sure that the correct insurance type (primary or secondary) is selected.
- Status — Select DROP.
- Kick reason — Enter a period to display the Kick Code Lookup tool.
- In the Kick Code Lookup tool, select Claim Redrop from the menu to display a list of kick codes used to re-drop claims.
- Select the appropriate kick code from the list. The DRPBILLING kick code is most commonly used in this case.
- Note — Enter a clear, detailed note to describe what you corrected or updated.
- Click Save Claim.
- Review the claim,
making sure that the claim status is no longer HOLD or MGRHOLD.
Note: If the claim is still in HOLD or MGRHOLD status, the claim requires additional work.
- On the Claim Edit page, move all balances to the secondary column and void applicable adjustments (you cannot switch payers if any adjustments are applied to the claim).
- Secondary payer — Change the selection to reflect the patient's tertiary payer.
- Force drop to paper for secondary — Select Yes-Athena to drop the claim to paper, and select TERTIARY: Tertiary Billing from the Reason menu.
Add Note section (bottom of the page)
- Applies to — Select Secondary Insurance.
- Status — Change the status to DROP.
- Kick reason — For non-Medicaid payers, enter DRPBILLING.
- Note — Enter a claim note saying "Claim dropped to tertiary insurance."
- Click Save.
The Claim Review page appears.
The claim is printed at athenahealth, where a staff member attaches a copy of the EOBs that appear in athenaOne for both the primary and the secondary payers. athenahealth then submits the paper claim to the tertiary payer.
- On the Claim Edit page, move all balances to the secondary column and void applicable adjustments (you cannot switch payers if any adjustments are applied to the claim).
- Secondary payer — Change the selection to reflect the patient's tertiary payer.
Add Note section (bottom of the page)
- Applies to — Select Secondary Insurance.
- Status — Change the status to CBOHOLD.
- Kick reason — For Medicaid payers only, enter TERTIARY.
- Note — Enter a claim note to indicate the reason for sending the claim to the tertiary payer.
- Click Save Claim.
The claim is printed at athenahealth, where a staff member attaches a copy of the EOBs that appear in athenaOne for both the primary and the secondary payers. athenahealth then submits the paper claim to the tertiary payer.
Exception for CO, GA, MA, NC, NJ, and OH: The claim is placed in Fully Worked Receivable (FWR) status because these states require electronic billing to Medicaid. athenaOne does not support electronic tertiary billing.
Important: Follow your state's Medicaid requirements and submit any required paperwork, as well as the primary and secondary EOBs, when sending your claim
Note: Medicaid CO, GA, MA, NC, NJ, and OH do not accept paper tertiary submissions.
- On the Claim Edit page, move all balances to the secondary column and void applicable adjustments (you cannot switch payers if any adjustments are applied to the claim).
- Secondary payer — Change the selection to reflect the patient's tertiary payer.
- Force
drop to paper for secondary — Select Yes-Practice, and select TERTIARY: Tertiary Billing from the Reason menu. When you select this option, the claim appears in the list of claims on the Generate Claims page that you can include in a paper claims batch at your practice.
Note: If you do not have this option, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Add Note section (bottom of the page)
- Applies to — Select Secondary Insurance.
- Status — Change the status to DROP.
- Kick reason — For Medicaid payers, enter DRPBILLING.
- Note — Enter a claim note saying "Claim dropped to tertiary insurance."
- Click Save.
The Claim Review page appears.
- On the Claim Edit page, move all balances to the secondary column and void applicable adjustments (you cannot switch payers if any adjustments are applied to the claim).
- Secondary payer — Change the selection to reflect the patient's tertiary payer.
- Force
drop to paper for secondary — Select Yes-Practice, and select TERTIARY: Tertiary Billing from the Reason menu. When you select this option, the claim appears in the list of claims on the Generate Claims page that you can include in a paper claims batch at your practice.
Note: If you do not have this option, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Add Note section (bottom of the page)
- Applies to — Select Secondary Insurance.
- Status — Change the status to DROP.
- Kick reason — Enter DRPBILLING.
- Note — Enter a claim note saying "Claim dropped to tertiary insurance."
- Click Save.
The Claim Review page appears.
Important: Follow your state's Medicaid requirements and submit any required paperwork, as well as the primary and secondary EOBs, when sending your claim.
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view).
- Scroll down to the Add Note section at the bottom of the page.
- Applies to — Select the payer type that is responsible for the claim.
- Status — Select the new claim status.
- Kick reason — Enter a kick reason code. You can enter data in this field only if you selected a new claim status from the Status menu. A warning message appears if you enter a kick code that is not appropriate for the selected status. You can also type a period in the Kick reason field to access the Kick Code Lookup tool. This tool displays only those kick codes that correspond to the claim status selected.
- Note — Enter a descriptive note to document the change of claim status. A claim note entered in this field appears under the Claim Notes section of the Claim Review, Claim Action, and View Claim History pages.
- Click Save. The claim is now updated.
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view).
- Make sure that there is an open balance in the payer column for which you need to change the payer. For example, if you need to bill a different primary, there must be an open balance in the primary column of the claim.
- Void any previously posted adjustments and transfers in the payer columns that you wish to change. Do not void any payments or takebacks. If you billed the incorrect payer in error and that payer paid on the claim, contact the payer to issue a refund. If you cannot open the balance properly because of the way payments are posted, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center for help.
- Primary payer or Secondary payer — Select the correct payers. A message alerts you that all transactions except for payments will be switched to the new payer when you select it.
Note: If you do not see the desired insurance listed in the menu, you must first add the insurance package to the patient's list of insurances. - Click OK.
- Add Note — Do not change the Applies to selection.
- Status — Select DROP.
- Kick reason — Enter DRPBILLING.
- Note — Document why you are changing the payers on the claim.
- Click Save Claim. The claim is now updated.
- Review the claim to ensure that no holds or rules have fired, and that it is now in drop status to the correct payer.
Note: If we receive adjudication back from a payer that is not listed on the patient's Quickview or under the View Cancelled Insurances section, and that payer can be matched to a specific claim, we select the insurance package "Unspecified Remit Payor" to post per the EOB. This happens most often when Medicare crosses over a claim to a payer not listed in the patient's account. To fix this, add the correct insurance package to the patient's account and change the secondary payer on the Claim Edit page to that payer. After you add the correct insurance package to the claim, the claim posting of the secondary column will still show "Unspecified Remit Payor." To correct this, please submit a support case asking for the claim to be posted to the correct secondary payer, or contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
-
Display the Claim Edit page:
-
In the text box at the top right of your screen, enter the claim number, select Claim ID from the menu, and then click the search icon. The Find tool looks for an exact claim ID match. (Searching for claims requires claim billing user permissions.)
-
Click the Go to Advanced View link on the Claim Action page
-
Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view)
-
On the Patient Actions Bar, click Billing, and then click Post Payment. On the Post Payment page, click edit claim (the link is on the line item's advanced view)
-
-
In the Charges section, click Split Charges.
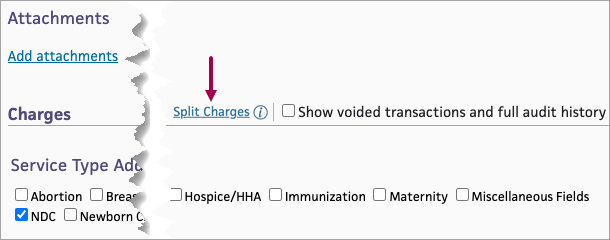
The Split Charges for Claim #[000000] page appears. -
Select charges to move from the Claim #[000000] column to the New Claim column. You can:
-
Check the box next to the Move → link to select all charges.
-
Check the box next to an individual row.
-
-
Click Move →
The selected charges move from the Claim #[000000] column to the New Claim column.
Note: To move charges back to the Claim #[000000] column, you can check the boxes in the charge rows of the New Claim column or check the box next to the Move ← link, and then click Move ←. -
Click Save Changes.
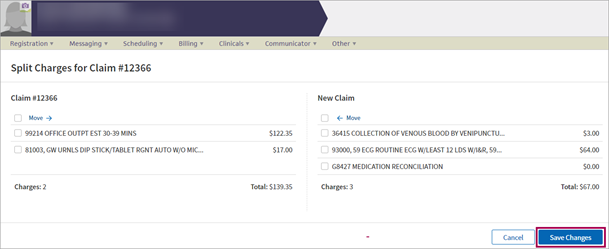
Note: The Save Changes button is only accessible when there are charges on both the original claim and the new claim. You can't move all of the charges off of the original claim to create a new claim. -
Notice claim rules run.
Important: The original claim scrubs once the charges move to the new claim. The new claim adheres to the normal claim generation process since it goes through the Rules Engine the same way it would if you were creating the claim from Charge Entry.
Note: The Cancel button disappears and the Save Changes button displays the word "Saving" and a spinning circle, indicating that the save is in progress. -
Review the status messages that appear to confirm a successful charge split and new claim generation.
Note: The original claim number stays on the left-side column labeled Claim #[000000]; the New Claim column changes to display the new claim number in the right-side column labeled Claim #[000000].
The Authorization field appears at different stages of the appointment workflow, so that you can add a new authorization or referral when it becomes known to you. Best practice is to add a new incoming authorization when you schedule the patient's appointment on the Schedule Appointment page.
You can add a new authorization by selecting Add new from the Authorization menu on any of these pages:
When you enter an authorization or referral on these pages, it is saved and associated with the primary insurance on the appointment or claim. You can click the Audit history link to display the history of previously saved authorizations and referrals.
On the Authorization Worklist page, you can view and filter all incoming and outgoing referral and precertification insurance authorizations. On the Insurance Authorization page, you can track, update, and complete incoming and outgoing insurance authorizations.
To add a new authorization on the Schedule Appointment page, Check-in page, or Claim Edit page:
- Authorization — Select Add new from the menu. Additional fields appear.
Note: If a patient cannot furnish all the authorization information, the authorization is still saved on the Authorization Worklist. - Notes — Enter any notes about the authorization.
These notes appear on the Insurance Authorization page. - Referring provider — Click Choose/view to display the Referring Provider Lookup tool. In the tool, you can search for the referring provider by number, name, specialty, or NPI number. Enter your search information and click Find. For more information, see Referring Provider Lookup.
Note: This field does not appear on the Claim Edit page. - Type — Select Pre-cert or Referral.
- Insurance authorization number — Enter the insurance authorization number.
- Effective date — Enter or select the effective dates for this authorization or referral.
- Authorized visits/units — Select Visits or Units from the menu, and then enter the number of approved units or visits in both fields. athenaOne automatically decrements the number of authorized visits or units.
- Referred-to provider — Select the provider to whom the patient is being referred.
This field automatically displays the name of the rendering provider (or the provider with whom you are scheduling the appointment on the Schedule Appointment page). - Specialty — Select the specialty of the provider to whom the patient is being referred.
This field automatically displays the specialty of the rendering provider (or the provider with whom you are scheduling the appointment on the Schedule Appointment page). - Diagnosis code — Enter or select the
diagnosis codes associated with the authorization. You can type a period to
access the Diagnosis Lookup tool in the ICD-9 or ICD-10 fields.
After you enter a diagnosis code, a description of the code is displayed to the right of it.
Note: If the diagnosis code that you entered is not coded to the highest level of specificity, a warning appears next to the code. - Procedure code — Enter or select the
procedure codes associated with the authorization. You can type a period to
access the Procedure Lookup tool.
After you enter a procedure code, a description of the code is displayed to the right of it.
Note: The exact procedure code is required if you select Units from the Authorized visits/units menu. The procedure is validated against your fee schedule. - Additional information — Enter any additional information that you want to record about this incoming authorization.
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view). You can also use the Find tool at the top of the screen.
- Some kick reasons require that a claim with $0 outstanding remain open until you close it manually. To close such a claim, review any active claim notes (in red), and resolve any issues noted.
- Ensure that all charges on the claim for the payer in question have been resolved (no balances or credits are due).
- Claim Status (at the top of the page) — Change the claim status to CLOSED.
- Add Claim Edit Note — Enter a claim note explaining what changes you made and why. A claim note entered here appears under the Claim Notes section of the Claim Review, Claim Action, and View Claim History pages.
- Click Save
Claim.
The claim is now closed.
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view).
- Scroll down to the charge lines. Under the Type column, locate the TRANSFERIN information.
- On the Claim Edit page, click Void this transaction for the transaction.
The Void Transaction page appears. - Click Void This Transaction.
- Click Continue. The Claim Edit page reappears showing the updated balance under the Ins1 column.
Medicaid not the secondary payer
If the balance is under the Ins1 column on the Claim Edit page and Medicaid is not the secondary payer, display the Claim Edit page for the claim:
- Secondary Payer — Select the secondary payer for the charge.
- Kick Reason — Enter the kick code that correlates with the EOB (COINSURANCE, DEDUCT, COPAY).
- Click Save Claim.
Medicaid is the secondary payer
If the balance is under the Ins1 column on the Claim Edit page and Medicaid is the secondary payer, display the Post Payment page for the patient:
- Locate the charge, highlight it, and click to expand the fields.
- Patient Insurance — Select the Medicaid payer.
- Other Transfer — Select the reason for the transfer. (Medicaid requires a reason that the charges are transferred to Medicaid.)
- $ — Enter the amount of the transfer.
- Click Save.
You can move patient payments made on a claim to unapplied credit for this patient.
Note: You can move only patient payments to unapplied credit.
- From the Claim Edit or Patient Activity page, display the Move Payment window for the payment that you need to work on.
 In the text box at the top right of your screen, enter the claim ID, select Claim ID from the search menu, and click the search icon. On the Claim
Edit page, scroll down to the Charges table and click move next to the payment transaction.
In the text box at the top right of your screen, enter the claim ID, select Claim ID from the search menu, and click the search icon. On the Claim
Edit page, scroll down to the Charges table and click move next to the payment transaction.On the Patient Actions Bar, click Billing, and then click Patient Activity. On the Patient Activity page, click Detail view at the top of the Patient Activity table. Locate the payment and click move.
- In the Move Payment window, select the Unapplied credit for this patient option.
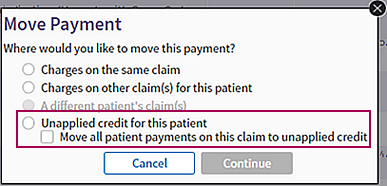
- If more than one patient payment was made on the claim, you can move all the payments to unapplied credit by selecting the Move all patient payments on this claim to unapplied credit option.
- Click Continue.
A confirmation message appears. (The message differs slightly, depending on whether you selected the Move all patient payments on this claim to unapplied credit option.) - Click OK.
The claim is updated, and all transactions occur within the specified payment batch. athenaOne automatically creates and closes the batch after a successful reposting.
You can void multiple patient transactions on a claim at once and move balances assigned to patient responsibility back to the insurance listed on the claim. When you select the Move responsibility from patient back to insurance option on the Move Payment window, you accomplish these actions:
- Move all patient payments on the claim to unapplied credit.
- Void all patient adjustments and transfers from the claim.
Note: The Move responsibility from patient back to insurance option on the Move Payment window applies only to patient transactions on a claim, not to insurance payments.
- Display the Claim Edit page:
 In the text box at the top right of your screen, enter the claim number, select Claim ID from the menu, and then click the search icon.
In the text box at the top right of your screen, enter the claim number, select Claim ID from the menu, and then click the search icon.
Note: This option does not appear on the Move Payment window when you access the Move Payment window from the Patient Activity page. - On the Claim
Edit page, scroll down to the Charges table and click move next to the transaction.
The Move Payment window appears. - In the Move Payment window, select the Move responsibility from patient back to insurance option.
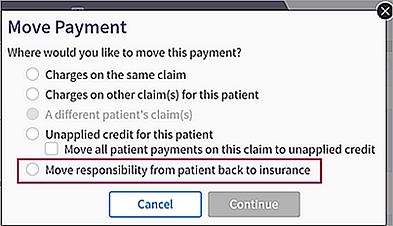
- Click Continue.
A confirmation message appears. - Click OK.
The claim is updated, and all transactions occur within the specified payment batch. athenaOne automatically creates and closes the batch after a successful reposting. - If some patient transactions cannot be voided, you see a message to that effect.
- In the message box, click OK.
The Claim Edit page appears. - Scroll down to the Charges table and select the Show voided transactions and full audit history option.
The Claim Edit page displays voided transactions as grayed out rows.
- In the message box, click OK.
- Display the
Claim Edit page:
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions. - Status — Select CBOHOLD.
- Kick reason — Enter PLSAPPEAL.
- Notes — Enter a text note about the appeal. Make sure to describe on what grounds you deem the claim a candidate for appeal, list facts to support the appeal, and indicate whether you attached any supporting documentation or faxed any documentation to athenahealth (you may want to do so).
- Click Save Claim.
- Display
the Claim Edit page of any claim for which
you have received an electronic payment (ERA):
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions. - Scroll to the charge line section near the bottom of the page.
- Identify
the charge history line that, in the type
section, the EOB (claim) link appears.
Note: This link appears only for remittance received electronically (for example, via ERA). - Click EOB (claim). The individual Athena Replicated EOB page appears.
- Click Print Athena Replicated EOB. The Windows print driver window opens.
- Make
any additional selections necessary (for example, number of copies).
Note: Do not change the default setting of "portrait" because EOBs printed in "landscape" could cause claims to be denied. - Click
Print.
Note: If the browser page settings for margins are greater than 0.25 inch left and right, the MREP will be truncated. To automatically configure your athenaOne settings to the 0.25 print margins, on the athenaOne login page, click the Configure browser link, and then follow the instructions.
Note: You can use the buttons to toggle back and forth between individual AREPs and MREPs. After you click View Whole EOB Batch, you can toggle back and forth between the AREP and MREP batches, but not individual EOBs.
- Display
the Claim Edit page of any claim for which
you have received an electronic payment (ERA).
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions. - Scroll to the charge line section near the bottom of the page.
- Identify
the charge history line that, in the type
section, displays the EOB (claim) link.
Note: This link appears only for remittance received electronically (for example, via ERA). - Click EOB (claim). The individual Athena Replicated EOB page appears.
- Click View Medicare Replicated EOB. The Medicare Replicated EOB page appears.
- Click Print Medicare Replicated EOB. The Windows print driver window appears.
- Make
any additional selections necessary (for example, number of copies).
Note: Do not change the default setting of "portrait" because EOBs printed in "landscape" could cause claims to be denied. - Click Print.
Note: If the browser page settings for margins are greater than 0.25 inch left and right, the MREP will be truncated. To automatically configure your athenaOne settings to the 0.25 print margins, on the athenaOne login page, click the Configure browser link, and then follow the instructions.
Note: You can use the buttons to toggle back and forth between individual AREPs and MREPs. After you click View Whole EOB Batch, you can toggle back and forth between the AREP and MREP batches, but not individual EOBs.
For claims with incentive payments, the Claim Edit page shows payment incentive information and a show incentive payments link so that you can view the details on the Remittance Record page.
Note: When you generate a Program Payment Worklist on the Program Payments page, the task bar entry for a remittance record includes a link to the claim if the claim includes an incentive payment.
- Display the Claim Edit page for a claim that has an incentive payment record:
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions. - Scroll down to the Remittance Records section and click show incentive payments (above the charge lines).
Note: This link appears when an incentive payment is posted to the claim. - Click the ID link to display the Remittance Record page for that payment.
athenaOne posts Merit-based Incentive Payment System (MIPS) payments at the charge level (these payments can be received via electronic remittance advice (ERA) or on paper EOB). These MIPS payments and adjustments appear in the Charges section of the Claim Edit page.
Note: Your organization must request this feature from athenaOne > Support > Success Community > Contact Client Support Center.
Transactions for MIPS payments on the Claim Edit page match the explanation of benefits (EOB), which makes readjudication easier and saves you time when you issue a refund for incentive payments.
Note: athenaOne may create remittance (unpostable) records for a small percentage of MIPS payments (see To view MIPS payments and adjustments for charges on a claim). These MIPS payments are from non-Medicare payers and do not include enough information to post at the charge level.
- Display
the Claim Edit page for any claim for which
you received a MIPS payments via ERA:
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
Note: You can also display claims that include MIPS payments on the Program Payments page. - Scroll
to the charge line section near the bottom of the page.
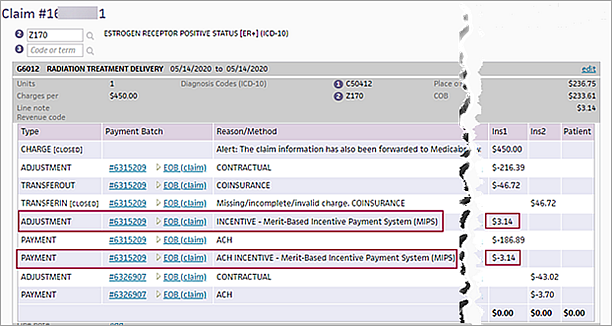
Charges related to MIPS payments are indicated by the text "INCENTIVE - Merit-Based Incentive Payment System (MIPS)" in the Reason/Method column. - You can click the EOB (claim) link to display the EOB. The MIPS payment appears in the Incent column.
Deleting a claim is an alternative to editing a claim. If charges were entered incorrectly, it may be quicker to delete the claim and start from scratch. You can delete a claim only if you have the appropriate access level. However, if the claim has been billed to the insurance carrier, we suggest that you wait until the payer adjudicates the claim. If the claim is deleted before the adjudication is received, the information is placed into a remittance record and sent to the practice for additional review.
To delete a new claim that has not been billed to insurance
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view).
- Verify the following information about the claim that you want to delete:
- No payments are posted against any charges.
- Post dates of the charges are in an open period.
- The claim was never billed.
- Click Delete This Claim.
A warning message appears. - Click OK to permanently
delete the claim, or click Cancel to preserve it.
A delete confirmation message appears if you click OK.
A Delete This Claim button appears at the bottom of the page.
To delete a claim that has already been billed to insurance
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view).
- Verify that no payments are posted against any charges on the claim that you want to delete.
- For each adjustment or transfer posted on the claim, click Void this transaction.
The Void Transaction page appears. - On the Void Transaction page, click Void This Transaction.
- After all adjustments and transfers are voided and only charges remain on the claim, void the charges.
When you void the last charge on the claim, the following message appears:
"Warning: Since this is the only charge on the claim, continuing with 'OK' will lead to deletion of this claim. Are you sure you want to void this charge?" - Click OK to permanently
delete the claim, or click Cancel to preserve it.
A delete confirmation message appears if you click OK.
- Display the Claim Edit page: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view). You can also use the Find tool at the top of the screen.
- Force drop to paper for primary — Select one of these options:
- No — The claim does not drop to paper automatically and is submitted according to the default submission method for the payer.
- Yes-Athena — Routes claims to athenahealth for paper claim submission. This option causes the claim to appear in the list of claims on the Generate Claims page that you can include in a paper claims batch.
- Display the Generate Claims page for additional instructions.
The Claim Form page displays a simplified view of the submitted claim with the option to view the claim in ANSI format.
- Display the Claim Edit or View Claim History page.
- Click View claim forms.
A selection window opens.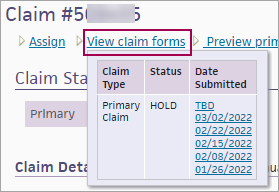
- In the Date Submitted column, click the version of the claim that you want to display.
The Claim Form window appears.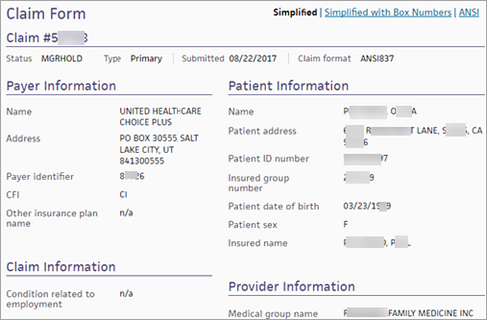
The Simplified view of the claim form is displayed.
Note: If the claim was dropped to paper (instead of being submitted electronically), the claim form is displayed in the CMS-1500 format. - To view box numbers on the claim form, click Simplified with Box Numbers at the top of the form.
- To view the claim in ANSI format, click ANSI at the top of the form.
Note: To see empty segments in the ANSI format, click Show empty segments at the bottom of the page.
- On the Claim Edit or View Claim History page, click View claim forms.
- In the Date Submitted column, click the version of the claim that you want to display. The Claim Form window appears.
- Click Simplified with Box Numbers at the top right of the form.
If the claim has an open balance, it will not print the CMS-1500 lines. To print an open claim on a CMS-1500 form, you can purchase blank CMS-1500 forms from an office supply company. If the claim is closed, it will print with the red CMS-1500 form lines. You can adjust your printer settings to print in black and white.
Note: The PDF Claim Printing feature must be enabled for your practice.
- Display the Claim Action page for a claim in HOLD status.
- Actions — Select Add Kick Reason from the menu.
- Kick reason — Enter "printonly" (or "PRINTONLY") and click outside the box.
The message "Print claim informational only; no status change" appears next to the Kick reason field. - Click Submit.
The claim appears below the View Attachments/EOBs button. - Format — You can select a different format from the menu and click Go.
- You can use the menu next to the Realign Claim button to select a different printer setting and then click Realign Claim.
- Click the Print icon
 .
.
A print version of the claim appears in a new window.
Note: To save the claim as a PDF document, click the Save icon. - Select the printer and then click Print.
In the state of Pennsylvania, it is legal to bill a patient's health plan when a workers compensation claim is in litigation.
- Attach the workers compensation litigation letter to the claim (use the Add attachments link).
For more information, see the Manage Attachments page. - Display the Claim Edit page.
- Patient's condition related to — Set the Employment option to No.
- Primary payer — Change the primary insurance from the workers compensation plan to the patient's health plan.
- Kick reason — Enter DRPBILLING.
- Note — Enter a claim note to explain the change (for example, "Workers comp in litigation; changed insurance to patient health plan").
- Click Save.
If you need to edit charges, you can edit them in the visit or directly on the claim.
- Click the Edit Charges in Visit link to edit charges attached to the claim in the visit.
Note: We recommend using this option unless you must enable editing for the entire claim. - Click the Enable editing link to edit charges directly on the claim.
Note: When you use this option, any changes you make in the visit are not propagated to the claim unless you make those changes manually. After you enable editing for a claim, you cannot disable editing.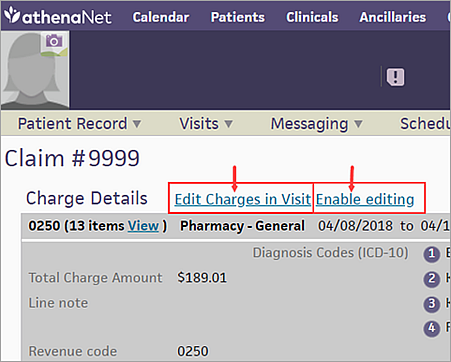
When you click Edit Charges in Visit, the Edit Visit Charges window appears so you can edit individual charges. 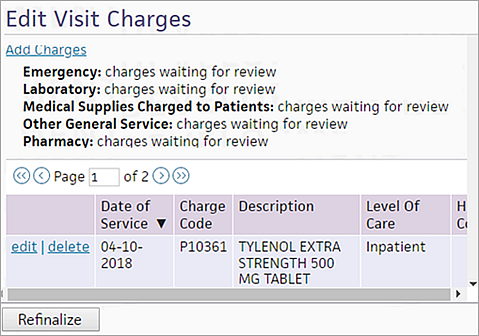
When you click Enable editing, a warning message appears, notifying you that edits made to the claim are not reflected in the visit. 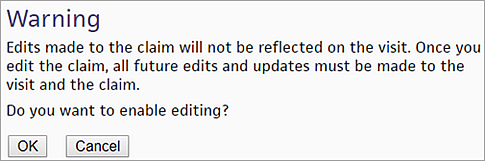
After you click OK, the new links disappear, and editing is enabled for all the charges on the claim.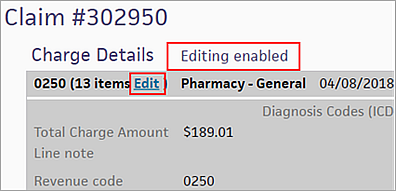
athenaOne automatically refinalizes unbilled or unpaid claims if:
- You make any changes to codes or charges on the visit, and
- The claim is unbilled or unpaid.
athenaOne scans for claims to refinalize nightly.
Note: You can also click Refinalize to refinalize an unbilled or unpaid claim manually.
On the Hospital Activity Summary page, all claims that need refinalization appear on the Needs Refinalization and Needs Late Charge Resolution worklists.
To edit charges in a visit and refinalize the claim
- Display the Claim Edit page:
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions. - Scroll down to the Charge Details heading and click Edit Charges in Visit to display the Edit Visit Charges window.
Edit the charges
- Click edit for the charge to edit. The edit charge window appears.
- Edit the charge as needed, and click Save.
Refinalize the claim
- Click Refinalize.
- Learn about kick reasons versus claim rules
- Learn about claim status, billing follow-up, and claim management — who is responsible?
- Learn how to correct claims in hold queues
Important: Visit & Claim Update is not available for any organizations that utilize athenaOne for Hospitals and Hospitals Health Systems.
A new save window appears if you make changes to a claim on Claim Edit.
In this window, you can either: save your edits, continue editing, or discard your edits and go to Visit & Claim Update to make your changes so that the connection between the claim and the visit is maintained.
Note: "Disconnected" refers to the disconnection of the claim from the visit when users directly edit claims by saving on the Claim Edit page. Claims created via the legacy Charge Entry workflow are never connected to a visit. Once the claim is disconnected from the visit (or if it was never connected to a visit), you will not be able to access the Visit & Claim Update page for that claim.
If you make direct edits on Claim Edit, a new messages appears in a save window where you can:
-
Save your edits
-
Continue editing
-
Discard your edits and go to Visit & Claim Update
-
Make the alert not appear for 90 days — Check the Don't show this warning again when editing claims box , and then click one of the buttons, to make the alert not appear for the next 90 days when editing claims.
Note: Choosing the Go to Visit & Claim Update option maintains the connection between the claim and the visit and allows the claim to be opened on Visit & Claim Update.
-
See a warning that you're about to disconnect a claim from the visit before you actually disconnect them in case you started editing on Claim Edit by mistake.
-
Better ensure that your practice staff is aware when they're about to disconnect a claim from the visit.
-
Help keep the claim and visit connected to make sure that automated claim update remains available for the claim.
A new window appears on Claim Edit when you go to save edits.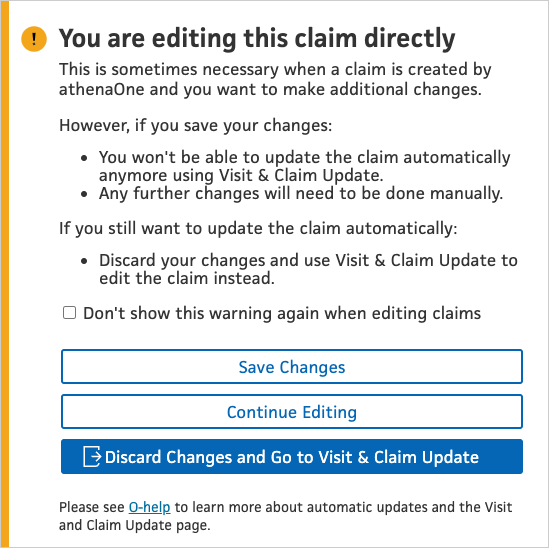
You're warned that saving these changes on Claim Edit will disconnect the claim from the visit.
| Field | Description |
|
Save Changes or Continue Editing |
When you click one of these buttons you can no longer open the claim on Visit & Claim Update. |
|
Discard Changes and Go to Visit & Claim Update
|
When you click this button your changes are discarded and the claim opens on that page instead. The connection between the claim and the visit is maintained and allows the claim to be opened on Visit & Claim Update. |
|
Don't show this warning again when editing claims |
When you check this box, and then click one of the buttons, the alert does not appear for the next 90 days. |
Note: This functionality is only available for FQHCs in the following states: AL, CA, OR, HI, MO, KS, OK, ME, MI, MS, WI, GA, AK, MT, TN.
When you edit information on Claim Edit, a new banner appears with the following alert. You're informed that editing the claim on this page will disconnect it from the associated visit.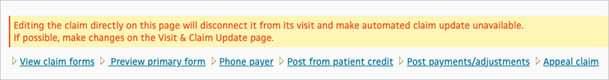
If you proceed with editing information on Claim Edit and save your changes, a new message appears in the banner to inform you that the claim is not connected to a visit and automatic formatting is no longer available on Visit & Claim Update (because the claim can no longer be opened on this page).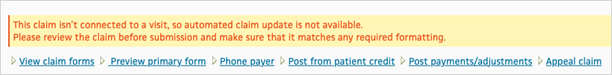
In the footer at the bottom left of the Workspace, you can use the Jump to.. tool to jump directly to any of the sections on the page, instead of scrolling up and down the page. 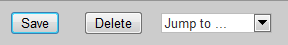
Tip: If you display the Claim Edit page to review the last claim note on the claim (that is, the most recent note), you may prefer to "Jump to... Add Note" and scroll up. Using "Jump to... Claim Notes" takes you to the first claim note (that is, the oldest note on the claim).
Only the items in red require action. Items in gray require no action — they document the claim history.
Note: When a Marketplace partner makes a change to the Claim Notes, you can see the name of that partner below the Claim Note.
For a detailed list of reasons why a claim is in HOLD, MGRHOLD, or CBOHOLD, display the View Kick Reasons page (On the Main Menu, click Claims. Under RESOURCES, click View Kick Reasons). The View Kick Reasons page also documents how claim status is associated with kick reasons or denials.
To add a claim note, use the Note field under the Add Note header at the bottom of the Claim Edit page.
To correct a claim that has been held by a "SCRUB" error, correct the claim according to the directions in the SCRUB claim note, save the claim, and change the claim status to "DROP." The claim is automatically sent to the payer.
Please do not put the claim back into CBOHOLD.
To view voided transactions and the claim audit history, check the Show voided transactions and full audit history checkbox to the right of the Charges heading.
Claim history is displayed directly below charge information, and voided transactions appear along with any charges for each procedure.
You can hover over any date field in a charge line or in the Claim Notes section to see the time that the event occurred. The time is displayed in HH:MM:SS 24-hour format. In the Charge History and Claim History sections, the time appears after the date.
If you believe the payer has rejected a claim inappropriately, please do not put the claim in DROP status. If you do, the claim is re-sent to the payer. Instead, please use the kick code "PLSAPPEAL" with a note explaining the issue, and an athenahealth staff member will assist you.
For self-pay patients, you can use the Check Fee Schedule page as a quick reference tool to look up fees for procedure codes.
Claim-level diagnoses appear under the Charges heading.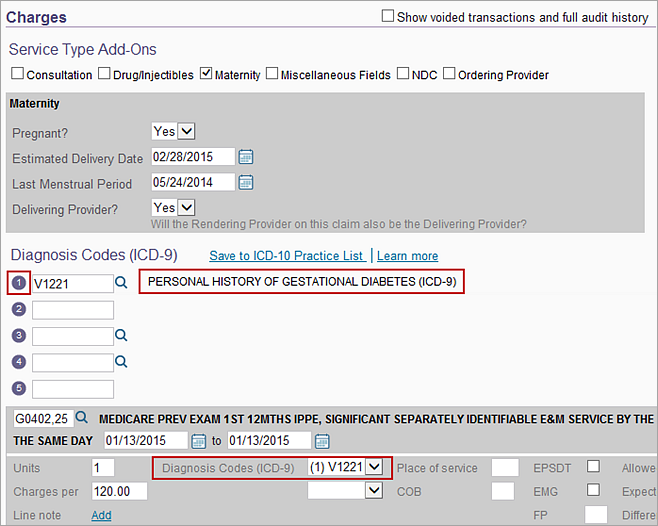
Diagnosis codes are arranged vertically, with the corresponding description to the right of each diagnosis code.
To the left of the diagnosis code, a number indicates the order on the claim (starting with 1 and continuing up to 12, as necessary).
In the procedure lines, both the number and diagnosis code that support the procedure appear.
By default, the data elements corresponding to each procedure are read-only. The Units field is updated automatically when you add a unit amount to a procedure code.
To change a charge or add a diagnosis to a procedure, click edit on the right. 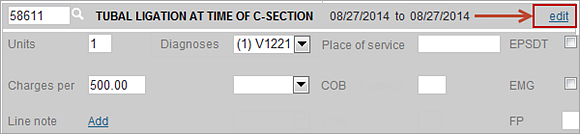
To add or edit a diagnosis on a charge, select any claim-level diagnosis code from the menu or add a new diagnosis. 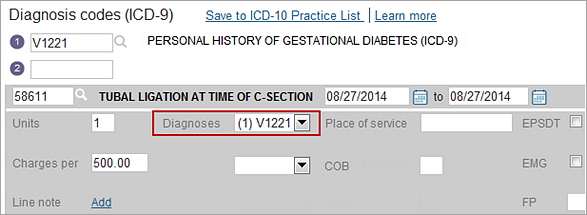
Adding a new diagnosis in the procedure section also adds that diagnosis at the claim level as the last diagnosis. The procedure section remains in edit mode until you save the claim.
Claim history is displayed directly below charge information; voided transactions appear along with any charges for each procedure.
Below the charge details for each procedure line in the Charges section, you can find links to any billing batches associated with the claim.
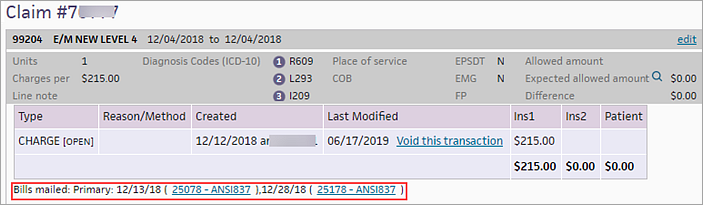
If you click a link, the View/Edit Billing Batch page opens.
If the claim was sent to collections, you can click the COLLECT, RECOVERY, or STOPCOLLECT link to see the collection batch file that was sent to a collection agency.
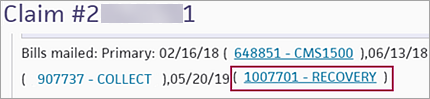
For more information, see Managing Collections and Collections Batch Management.
Provider-based billing practices need to store provider and department information about charges that were migrated from one facility claim to another and thus comply with the CMS 24-hour rule. The Charges section of the Claim Edit page includes charge-specific fields for Rendering provider, Supervising provider, and Facility (department).
Note: The CMS 24-hour rule mandates that all clinically related facility charges for a single patient be bundled together and submitted on the same UB-04/837I facility claim, regardless of whether they were performed by the same provider and/or in the same department of the clinic. (This requirement applies to provider-based billing clinics.)
Because revenue codes can differ from one fee schedule to another for any single procedure code, a charge-level field, Revenue code, is included in the Charge section of the Claim Edit page so that billers can override the revenue code that is tied to that procedure in their current fee schedule.
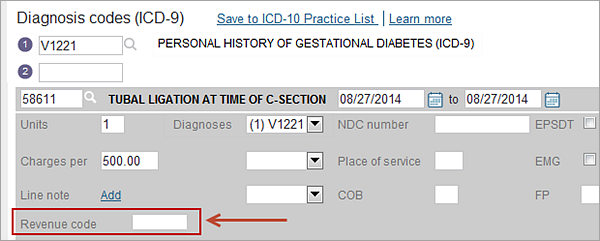
Note: Any revenue code that you enter in this field appears on the UB-04 paper form and 837I electronic submission when you create the claim. When left blank, the revenue code in your current fee schedule is used when submitting facility claims in the UB-04/837I claim formats.
Note: These fields are for reporting purposes on general ledger reconciliation; they are not sent on the UB-04 or 837I facility claims. These fields appear in the Charges area on the Claim Edit page and under the Transaction field heading in Report Builder only for practices that have the View/Edit Provider and Department at Charge Line feature enabled.
These fields are used in Provider-Based Billing or similar cases where charges must be merged from one claim to another to comply with the CMS 72-hour/24-hour rules. The first three fields appear in the Charges area of the Claim Edit page only if the View/Edit Provider and Department at Charge Line practice setting is enabled.
- Rendering provider — Menu that appears in the Charges area to store the rendering provider that performed the service for a charge in cases where it differs from the claim-level value. This value will be submitted on each charge line for electronically submitted institutional claims (837I claim format). If left unchanged, this field always matches the claim-level value (even if Rendering Provider is changed at the claim level later). The values that appear in this menu ignore the values set by the "provider" billing admin setting.
- Supervising provider — Menu that appears in the Charges area to store the supervising provider that performed the service for a charge in cases where it differs from the claim-level value. This value is not submitted on institutional claims (UB-04 or 837I claim formats). If left unchanged, this field always matches the claim-level value (even if Supervising Provider is changed at the claim level later). The values that appear in this menu ignore the values set by the "provider" billing admin setting.
- Facility — Menu that appears in the Charges area to store the facility (department) that performed the service for a charge in cases where it differs from the claim-level value. This value is not submitted on institutional claims (UB-04 or 837I claim formats). If left unchanged, this field always matches the claim-level value (even if Facility (department) is changed at the claim level later). The values that appear in this menu ignore the values set by the "department" billing admin setting.
- Revenue code — This field appears only if the UB‑92 feature is enabled. Appears in the Charges area so that billers can indicate a different revenue code from the one associated with the current fee schedule for that charge's procedure code. This field is primarily used in provider-based billing or similar billing scenarios when charges are merged from one claim to another and the originating fee schedule indicated a different revenue code. This value is submitted on institutional claims (UB-04 or 837I claim formats). When left blank, the revenue code in the current fee schedule is submitted on institutional claims (UB-04/837I).
When athenaOne receives an update to certain charges by interface, it voids the original charge and replaces it in a new charge line with the most recent message and units. A claim note alerts you to the voided and replaced charges.
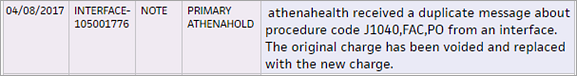
Best practice: If you intend to bill multiple units per charge, please send the information on one charge line and indicate the number of units.
The replacement of charges happens only when the following claim information matches:
- Patient
- Provider
- Date of service
- Procedure code and modifier
- Charge from date
- National Drug Code (if present)
- Primary diagnosis

Use the (NEW) Transaction History page for additional visibility into how payments are posted across all charges for the claim, including a timeline view and details by procedure code.
Note: The first release (March 2025) is only for non-FQHC customers and focuses on claims fully paid by the primary payer (Billed amount = Paid amount). We’ll continue to add more posting scenarios in upcoming releases.
athenahealth reviews certain types of claim denials and resolves the denials when possible. If athenahealth is unable to resolve and resubmit the denied claim, or if the denied codes are not expected to be paid if resubmitted, we return the claim to you with claim note advice.
If your organization uses both athenaCollector and athenaClinicals, athenahealth reviews coding-related back-end denials for claims that have been denied with the following codes.
- AGECPTMATCH
- AGEDXMATCH
- CPT
- CPTCHANGE
- DIAGNOSIS
- DXCPTMATCH
- GENDERCPTMATCH
- GENDERDXMATCH
- MODCPTMATCH
- MODIFIER
- POS
- POSCPTMATCH
If a claim has one of these coding denials and has clinical documentation in the patient chart, athenahealth assigns the claim to CBOHOLD status. After we review the claim, we mark it with one of the following tags:
- **CODING ADVICE** — If a claim needs a coding correction, we add claim note advice and return the claim to you. After you make the necessary changes and apply the DRPBILLING kick code, athenahealth resubmits the claim.
- **ADVICE TO ADJUST** — If a claim is unlikely to be paid due to payer billing requirements, we may add advice for adjustment and return the claim to you.
- **DOCUMENTATION REQUEST** — If a claim has insufficient clinical documentation to support billing, we return the claim to you with a claim note. After you add or update the clinical documentation, we will review it.
If we find that the payer erroneously denied a claim, athenahealth resubmits the claim after reviewing the billing and supporting clinical documentation.
If your organization uses both athenaCollector and athenaClinicals, athenahealth reviews denials related to medical policies and insurance benefits for claims that have been denied with the following codes:
- MEDPOLICY — athenahealth reviews the claim and available medical records to verify insurance package selection.
- NCPREVIEW — athenahealth reviews the claim and available medical records to verify insurance package selection.
- MP — athenahealth reviews the claim and available medical records to verify insurance coverage.
- SERVICEMAX — athenahealth reviews the claim and available medical records to verify insurance coverage.
- NMN — athenahealth reviews the claim and available medical records to verify medical necessity.
When athenahealth reviews these denials, we assign the claim to CBOHOLD status and attempt to resolve and resubmit the claims to the payer. If we are unable to resolve the issue and resubmit the claim, or if the denied codes are not expected to be paid if resubmitted, we return the claim to you with clear coding or adjustment advice or we request additional medical records.
Note: athenahealth is assuming this work gradually, through 2019. When this feature becomes available to your organization, you will receive an athenaNetwork posting.
athenahealth reviews denials with an IPN or NEREVIEW kick code for claims with or without an insurance card on file in athenaOne. These denials indicate that the patient's insurance information is incorrect (IPN kick code) or that the patient's eligibility is in doubt (NEREVIEW kick code).
If a claim has one of these patient insurance denials with no associated insurance card image, we assign the claim to CBOHOLD status and attempt to resolve and resubmit the claim to the payer.
Note: For information about other insurance-related denials, see Eligibility-related denials.
If athenahealth is unable to resolve the issue and resubmit the claim, we send a statement to the patient with a note asking the patient to contact you to provide updated insurance information. (This note appears in the Patient Statement Note section of the Patient Account View page.)
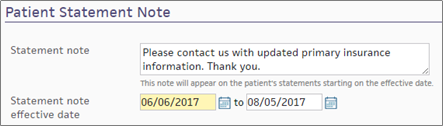
If athenahealth cannot resolve the patient insurance issue and the patient cannot be billed, the claim may be returned to you for review.
Note: athenahealth is assuming this work gradually, through 2019. When this feature becomes available to your organization, you will receive an athenaNetwork posting.
athenahealth automatically reviews claims that have been denied with the following codes:
- INDICATOR — athenahealth makes claim formatting corrections.
- NDCNUMB — athenahealth corrects the National Drug Code (NDC) number based on claim coding and medical records.
- PRACCHGRVW — athenahealth corrects posting issues.
When athenahealth reviews these denials, we assign the claim to CBOHOLD status and attempt to resolve and resubmit the claims to the payer. If we are unable to resolve the issue and resubmit the claim, we return the claim to you with clear instructions for next steps based on our research.
Note: athenahealth is assuming this work gradually, through 2019. When this feature becomes available to your organization, you will receive an athenaNetwork posting.
Beginning in April 2025, we're automating some low dollar amount athenahealth denials management tasks for charges that are unlikely to be paid.
Benefits:
- Automated tasks for faster turnaround time
-
Improved claim note format that is easier to read
- Reduced volume of claims that need resubmission
-
Focused coder intervention only where coding corrections are actually needed
- Reduced manual work for practice staff and athenahealth Denials Management team
Note: This automation only applies to CBOHOLD denials that are reviewed by the athenahealth Denials Management team.
What's automated?
- The athenahealth AI technology reviews the claim.
-
Using advanced machine learning techniques and continuous data analysis, the model identifies charges that are highly unlikely to be paid upon resubmission (based on historical payment trends and payer guidelines).
-
The athenahealth AI technology adds a claim note with details specific to the denied charges.
Will the AI-generated claim notes look different?
-
The claim note added by the athenahealth AI technology will look very similar to the claim note that is manually added by the athenahealth Denials Management team.
-
Both the manually added note and the automatically added note will have:
-
Specific details about the denied charges
-
Action: NOTE
-
Claim Status: MGRHOLD
-
- The User on the claim note will be different:
Manually added claim notes have User: <athenaOne username>
AI-generated claim notes will have User: AI Insight
| athenaOne release date | Type of Denials | Automated claim note/ kick code |
|---|---|---|
| April 2025 | Coding, Medical policy, and Benefit coverage denials |
"Advice to Adjust" / [ADJUST] kick code |
| June 2025 | Unspecified denials – When the payer has not provided a denial code, or when the payer has provided a denial code that does not indicate any helpful or guiding information. The denial requires additional research or payer contact. |
"Advice to Adjust" / [ADJUST] kick code |
| June 2025 | Coding denials that might be resolved with coding-related changes |
"CODING ADVICE" / coding-related kick code |
| October 2025 |
Coding denials with no coding changes needed
|
"Advice to Adjust" / [ADJUST] kick code |
Your practice can continue to use your existing workflow for handling claims on MGRHOLD with "Advice to Adjust" or "CODING ADVICE".
We plan to expand to other types of denials in upcoming releases. The updates will be communicated to you in future release notes.
- Display the Claim Edit page for a claim that is eligible for real-time adjudication: Click the edit claim link on the Claim Review or Post Payment page (the link is on the line item's advanced view). If the payer offers RTA and the claim is eligible, you see a link to submit claim for RTA at the bottom of the page.
- Click
submit claim for RTA at the bottom of the page to send the claim
to the payer. The elapsed time counter appears at the top of the page,
while the claim is being sent, adjudicated, and returned.
The Real Time Adjudication Notice appears when the claim has been returned.
Note: See also: Real Time Adjudication
Note: This feature works with Readjudication Notices that match a claim in the same remittance.
- Display the Claim Edit page for a claim that associated with readjudication remittance records.
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions. - Scroll down to the Claim Summary (just below the Service Type Add-on checkboxes).
- Click show readjudication records.
A row appears for each Readjudication Notice, with these columns:- Created — The date of the remittance that included the record (usually the check date or pay date).
- Readjudication Notice — The record ID (links to the remittance record).
- Payer — The payer that sent the readjudication.
- Amount — The amount of the Readjudication Notice record.
- Payer Recouped — The sum of associated Provider Takeback records.
- Amount Outstanding — The amount the payer has not yet recouped.
- Click show readjudication records again to collapse the readjudication summary view.
You can gain better insight into claim errors that athenaOne may encounter when creating a claim.
These errors should be infrequent but, when one does occur, athenaOne shows the specific table or data that may be causing the error. However, when there is an unspecified error, athenaOne is unable to identify the cause.
Note: athenaOne does not determine whether the error you encountered was corrected. When you return to the visit that contained an issue, you'll see a reminder that the last attempt to create a claim resulted in an error.
The following claim creation error alerts appear on Claim Edit:
The following error alert appears when the claim cannot be created due to the practice's fee schedule not containing per diem data.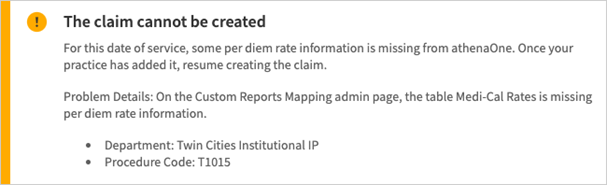
When you resolve the issue (or simply return to the same visit), athenaOne displays a reminder that when you previously tried creating a claim it resulted in an error because the specific per diem data was not in your practice's fee schedule.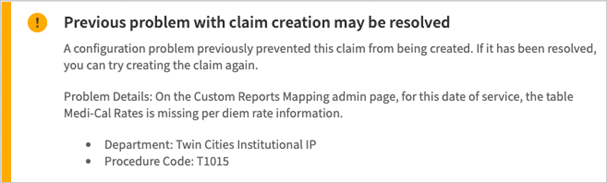
The following error alert appears when the claim cannot be created due to the practice's fee schedule not containing the specific procedure code.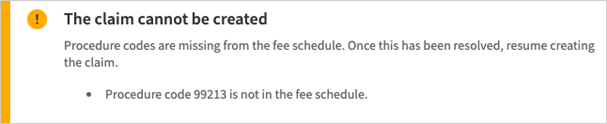
When you resolve the issue (or simply return to the same visit), athenaOne displays a reminder that when you previously tried creating a claim it resulted in an error because the specific procedure code was not in your practice's fee schedule.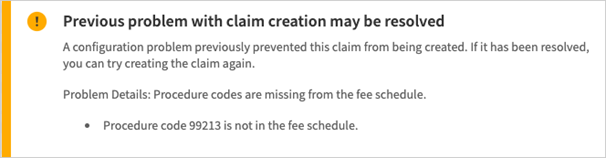
The following error alert appears when the claim cannot be created due to a configuration issue. In this example there are conflicting rows in a table of the Custom Reports Mapping admin page.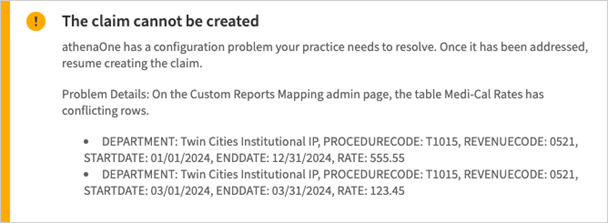
When you resolve the issue (or simply return to the same visit), athenaOne displays a reminder that when you previously tried creating a claim it resulted in an error because there were conflicting rows in a table of the Custom Reports Mapping admin page.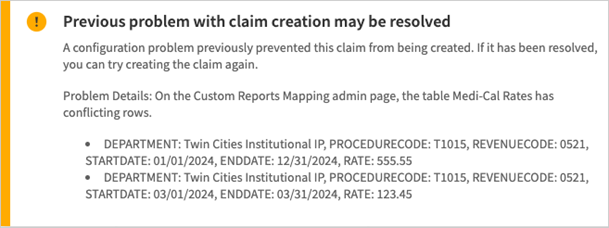
The following error alert appears when the claim cannot be created due to an unspecified issue.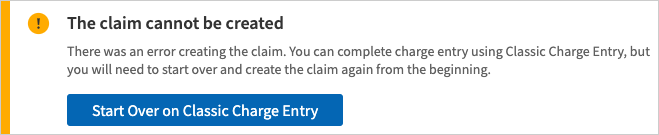
When you resolve the issue (or simply return to the same visit), athenaOne displays a reminder that when you previously tried creating a claim it resulted in an error because there was an unspecified issue.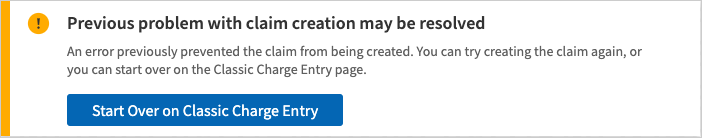
To enable service type add-ons, you must contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Note: Some service type add-ons are available only on the Claim Edit page (not on the Charge Entry page).
| Service Type Add-On — Abortion | |
|---|---|
| Special Program Code |
Select the reason the abortion services were performed. Compliant use of this field is applicable according to the state laws of each client, and may be provider-driven. Please consult your legal advisor or state healthcare agency for compliance guidelines. |
| Service Type Add-On — Anesthesia | |
| Surgeon |
Select the primary surgeon from the menu. This menu is populated from the Referring provider table. |
| Concurrency |
A claim level field typically populated by the value calculated in the anesthesia time sheet. When entering charges outside the anesthesia workflow, however, the practice user can enter the concurrency level, calculated manually, in this numeric field. |
| Anesthesia Type |
This value is typically populated from the anesthesia time sheet. But, the practice user can complete this field on the charge entry page. Further, rules can be conditioned on the anesthesia type selected. For example, if the practice user identifies the services as a monitored anesthesia case (MAC), a rule could be created to require the user to modify the anesthesia services with a MAC modifier. |
| Start Time |
The start time of an anesthesia case is entered in 24-hour format. Minutes are exclusive. A start time of 08:00 and end time of 08:30 returns total minutes of 30. |
| End Time |
The end time of an anesthesia case is entered in 24-hour format. Minutes are exclusive. A start time of 08:00 and end time of 08:30 returns total minutes of 30. |
| CPT Code |
Users entering anesthesia services using the Charge Entry page generally complete the Procedure code field with an ASA code. Practice users have the option of recording the surgical CPT code describing the patients surgery. Note: Although athenaOne does not systematically map CPT codes to ASA codes on the Charge Entry page, rules have been created to compare the two values when entered to ensure that they are appropriate. |
| Service Type Add-On — Breast Care | |
| TPL Denial Date |
The date the primary insurance denied the claim. (Note: TPL = Third Party Liability). |
| Result Code (Breast) |
Result code for breast or cervical procedures. Select from the menu of acceptable values provided by the Program. |
| Recommendation Code (Breast) |
Recommendation Code for breast or cervical procedures. Select from the menu of acceptable values provided by the Program. |
| Result Code (Cervical) |
Result code for breast or cervical procedure(s). Select from the menu of acceptable values provided by the Program. |
| Recommendation Code (Cervical) |
Recommendation Code for breast or cervical procedures. Select from the menu of acceptable values provided by the Program. |
| Months for Short-Term Follow-Up |
Required if recommendation code is 2. |
| Tumor Size (cm) |
Size of Tumor. Required for procedures 19160, 19162, 19180, 19240. |
| Tumor Stage |
Required if tumor size is present. |
| Treatment Started? |
Select Yes if surgery, chemotherapy, or radiation has been started; otherwise, select No. |
| Reason Code for No Treatment |
Select if treatment has not started. |
| Pap Smear Adequacy Code |
Select an acceptable value provided by the Program from the menu. |
| Service Type Add-On — Consultation | |
| Ordering Provider |
Enter the provider ordering services or supplies, if different from the rendering provider (Referring Provider Lookup tool available). This is required for HCPCS procedure codes that describe consultative services. Medicare claims require a referring provider and/or an ordering provider. |
| Second Opinion for Surgery |
Select Yes if the claim is for a second opinion for surgery; otherwise select No. |
| Service Type Add-On — Corporate Billing | |
| Test/Specimen Number |
Enter the test/specimen number in the field provided. Note: To enter additional notes in the Line note field, click edit (upper right corner of the charge line) and then click Add next to Line note. |
| Service Type Add-On — COVID-19 | |
| Was the patient suspected of having, diagnosed with, or tested for COVID-19 at the time of the encounter? |
Select Yes or No to indicate whether the claim is for services related to COVID‑19 care. If you select No, you cannot select answers in the remaining fields.
The athenahealth rules engine uses the answers to these questions to determine which COVID-19 related rules should fire on the claim, particularly when the patient is COVID-19 presumptive positive. You may notice a change in hold volume for claims related to COVID-19 care as rules adapt to changing payer requirements and as athenahealth gains more information about COVID-19 federal grant requirements. Note: You can use the Report Builder to report on the answers to this question in the COVID-19 service type add-on. The COVID-19 Suspected display column and filter are available in the Claim category of these report types in the Report Builder: Appointment, Claim, FCC Activity, Transaction Activity, and Transaction Aging. |
| Does this claim include services related to COVID‑19 testing? |
Select Yes or No.
The COVID-19 service type add-on appears on claims created with or without an appointment. Note: You can use the Report Builder to report on the answers to this question in the COVID-19 service type add-on. The COVID-19 Testing display column and filter are available in the Claim category of these report types in the Report Builder: Appointment, Claim, FCC Activity, Transaction Activity, and Transaction Aging. |
| Is the provider or medical group out-of-network with the patient's insurance? |
Select Yes or No.
You can use the answer to this question in conjunction with the COVID‑19 related patient balance hold to help you meet the CARES Act Provider Relief Fund grant requirements. For information about the COVID-19 related patient balance rule, see COVID-19 Management: Patient Balance Hold Rules Request on the Success Community. Note: You can use the Report Builder to report on the answers to this question in the COVID-19 service type add-on. The COVID-19 Out of Network display column and filter are available in the Claim category of these report types in the Report Builder: Appointment, Claim, FCC Activity, Transaction Activity, and Transaction Aging. |
| Service Type Add-On — Diagnostic Services | |
| Purchased Services? |
Select Yes for claims with modifier -90 (Reference (Outside) Laboratory). This indicates your practice has purchased testing kits from an outside party (CMS-1500 line 20 or equivalent). |
| Purchased Services Provider |
Select the provider supplying purchased services. For example, a physician may purchase a diagnostic exam from an outside entity. (Referring Provider Lookup tool available.) Required if Purchased Services? is set to Yes. |
| Ordering Provider |
Select the provider who ordered the services this is required if Purchased Services? is set to Yes. You can type a period to access the (Referring Provider Lookup tool. |
| Purchased Services Amount |
Enter the total cost (dollar amount) or the purchased services included on the claim. This is required if Purchased Services? is set to Yes. |
| Service Type Add-On — Dialysis | |
| Patient's Weight (pounds) |
Enter the patient's weight in pounds. This is required for EPO claims for patients on dialysis. |
| Service Type Add-On — DME | |
|
|
DME Section — This section of the add-on is used to report the length of need and certification type for DMERC CMNs excluding O2.
Complete the DME section fields only for procedures where a certificate of medical necessity (CMN) from the provider is required. For oxygen therapy claims, however, do not complete these fields. |
| DME Certification Type |
Code indicating the type of certification. |
| DME Certification Revision Date |
The date the last certification was obtained from the Provider. The DME Certification Revision date must be provided if you have indicated a DME Certification Type of Renewal or Revised. |
| DME CMN Quantity (months) |
Used to report the length of need for this CMN. Quantity is reported in months. Note: For the DME information to be submitted with a DME claim, you must complete both the DME certification type as well as the DME CMN quantity. |
| DME Therapy Begin Date |
The date DME therapy began. |
|
|
Oxygen Therapy — Used to report O2 CMN information. Required for all home oxygen therapy claims. |
| Oxygen Therapy Certification Type |
Code used to specify the type of certification. |
| Oxygen Therapy Certification Revision Date |
The date the last certification was obtained from the Provider. The Oxygen Therapy Certification Revision date must be provided if you have indicated an Oxygen Therapy Certification Type of Renewal or Revised. |
| Oxygen CMN Quantity (months) |
Used to report length of need for this CMN. Quantity is reported in months. Note: For the Oxygen therapy information to be submitted with a DME claim, you must complete both the Oxygen therapy certification type as well as the Oxygen CMN quantity. |
| ABG Test Results |
Used to report arterial blood gas result. |
| ABG Test Date |
The date of the arterial blood gas test. |
| Oxygen Test Condition |
Used to report condition under which test occurred. |
| Oxygen Saturation Test Results |
Used to report oxygen saturation blood result. |
| Oxygen Saturation Test Date |
The date of the oxygen saturation test. |
| Oxygen Flow Rate |
Valid values are 1 — 999 liters per minute and X for less than 1 liter per minute. |
| Oxygen Test Findings |
Used to answer questions 8, 9, and 10 of the Oxygen CMN. User can select multiple findings from the list. |
| Oxygen Therapy Begin Date |
The date oxygen therapy began. |
|
|
CRC DMERC Condition Indicators — Used to report conditions related to all DMERC CMNs. If either the DME section or the Oxygen therapy section is completed, this section of the add-on is required. |
| Type of Condition Indicator |
Qualifier specifying the use of this section of the add-on. |
| Conditions Apply? |
The "Condition Apply Y/N" flag is the ANSI Certification Condition Code applies indicator. A "Y" response indicates the condition codes in Condition Indicators Codes apply; an "N" response indicates the condition codes in do not apply. |
| Condition Indicators |
Condition Code describing either patient or equipment status. |
| Date Certification Signed by the Physician |
If you have indicated with a condition code that the 38-Certification signed by the physician is on file at the supplier's office, you must provide the date that the certification was signed by the physician. |
| Patient's Weight (pounds) |
Patients weight is required when submitting claims to Medicare Durable Medical Equipment Regional Carriers with certificates of medical necessity. |
|
|
Supporting Documentation — This section of the add-on is used to report responses to CMN questions. |
| Form Identifier |
Used to report the CMN form number. Must be a valid OMB approved CMN form number excluding alpha characters. |
| Question Number/Letter |
Used to report CMN question number. For multi-part questions that are not numbered individually, assign letters left to right, top to bottom, keeping question numbers constant. Must include both numbers and letters together in this field. |
| Response Code |
Used to report responses to any CMN question that requires a Y/N response. |
| Date |
Used to answer CMN questions that require a date response format. |
| Percent |
Used to answer CMN questions that require a percent response. |
| Additional Information |
Used to answer CMN questions that use a text or uncodified response format. Note: These information fields do not appear until a number is provided in the question number/letter field. |
| Service Type Add-On — Drug/Injectables | |
| Patient's Weight (pounds) |
Enter the patient's weight in pounds. |
| Service Type Add-On — EPSDT | |
| Complete EPSDT screen? | Select Yes to indicate that the physician completed the EPSDT screening. Select No to indicate that the physician did not complete the EPSDT screening. |
| Service Type Add-On — Family Planning | |
| Purpose of visit | Select the purpose of this visit from the menu. |
| Interpreter needed | Select Yes if the patient requires an interpreter. |
| Number of pregnancies | Enter the number of pregnancies the patient has had. |
| Number of births |
Enter the number of times the patient has given birth. |
| Last pregnancy ended | Select the date when the patient's last pregnancy ended. |
| Contraceptive (prior to visit) | Select the type of contraception (if any) used by the patient before the visit. |
| Contraceptive (after visit) | Select the type of contraception (if any) that the patient will use after the visit. |
| Give reason for "none" | If you selected none from the Contraceptive (after visit) menu, select the reason for this option from the menu. |
| Pregnancy test | Select the result of the administered pregnancy test (negative or positive). If no test was given, select not tested. |
| Pregnancy desirability |
Select the appropriate option for pregnancy desirability. |
| Routine medical services provided |
Select all routine medical services provided. |
| Other medical services provided | Select all other medical services provided. |
| Lab services provided |
Select all lab services provided. |
| Referring for non-family planning services | Select all referred non-family planning services. |
| STD tests/diagnoses |
Select all STD tests and diagnoses administered. |
| STD treatments | Select all STD treatments given. |
| HIV pre-test counseling |
Select Yes if HIV pre-test counseling was provided. |
| HIV test | Select Yes if an HIV test was administered. |
| HIV test result |
Select the result of an administered HIV test (negative or positive). If no test was given, select not tested. |
| HIV post-test counseling | Select Yes if HIV post-test counseling was provided. |
| Provider of medical services |
Select all providers of medical services. |
| Counseling services provided | Select all counseling services provided. |
| Provider of counseling services | Select all providers of counseling services. |
| Service Type Add-On — Foreign System Identifier | |
| Client System identifier |
By default, the value of this field is hidden unless the + is clicked. The values populating the Foreign System Identifier fields are controlled by the interface; however, users can manually modify these values.
Additional values can be stored at the charge level in addition to the claim level (see Foreign System Identifier field below). |
| Foreign System identifier |
This appears on the charge level so you can store a Foreign System Identifier for an individual charge. |
| Service Type Add-On — Hearing/Vision | |
| Prescription Date |
Enter the prescription date. Required if it was required in the Reserved(19) (remarks). |
| Service Type Add-On — Hospice/HHA | |
| Patient is Home Bound? |
Select Yes if the patient is homebound, otherwise select No. |
| Hospice/Home Health Agency |
Hospice or Home Health Agency name — click choose/view to select from a list.
Note: A claim rule assigns HOLD status to all claims billed with procedure codes 99374, 99375, 99377, 99378, G0179, G0180, G0181, and G0182 that do not contain the complete name and address of the Hospice/HHA facility and Medicare ID number. |
| Hospice ID Number |
Enter the 6-digit facility ID of the patient's hospice or home health agency.
Note: A new scrub rule assigns HOLD status to all claims billed with procedure codes 99374-99375, 99377-99378, G0179, G0180, G0181, and G0182 that do not contain the complete name and address of the Hospice/HHA facility and Medicare ID number. |
| Provider is a Hospice Employee? |
Select Yes if the provider is an employee of the hospice. This flag is necessary for all Medicare claims involving physician services to hospice patients. |
| Ordering Provider |
Select the provider ordering services or supplies; if different from the rendering provider, click choose/view to select from the Referring Provider Lookup tool. |
| Service Type Add-On — Immunization | |
| Immunization Lot Number |
Enter the serum lot number if required by state law for health data reporting. Note: You can report only one serum lot (or batch) number per claim. You must create an additional claim if you need to report a second serum batch number. |
| Service Type Add-On — Maternity | |
| Pregnant? |
This field is automatically populated with the information from the OB episode. Required in some states. Required for Indiana Medicaid. Required if LMP is entered. |
| Estimated Delivery Date |
This field is automatically populated with the date from the OB episode. |
| Last Menstrual Period |
This field is automatically populated with the date from the OB episode. |
| Delivering Provider |
Select Yes to indicate that the rendering provider on the claim is also the delivering provider. Select No to indicate that the rendering provider on the claim is not the delivering provider.
Note: When the provider of antepartum care is the same as the delivering provider, denials are common because of global coverage for pregnancies. For antepartum care, it is important to indicate when this is provided by the delivering provider. |
| Service Type Add-On — Medicaid TX | |
| Benefit code | Enter the benefit code specific to Medicaid TX. The code is required for certain types of claims only. |
| Service Type Add-On — Miscellaneous Fields | |
| Service Auth Exception Code |
Select the reason why a provider did not obtain a service authorization for a service that state law (for example, New York State Medicaid) requires an authorization. |
| Delay Reason Code |
Select the reason why a claim was filed past the filing date or the reason why a claim transmitted in response to a request for information was delayed. |
| Special Program Code |
Select the program under which services provided to the patient were performed. |
| Service Type Add-On — NDC | |
| NDC number |
NDC information is copied from your practice's fee schedule, unless you enter it manually.
When you enter a valid number in the NDC Number field, athenaOne displays the corresponding athenaCodesource trade name to the right of the field. This allows you to confirm that the NDC number entered is correct for the procedure code.
Note: NDC is an 11-digit number with the format "xxxxx-xxxx-xx." If one segment is not formatted correctly, add a leading "0" to that segment (for example, 12345-123-12 becomes 12345-0123-12). For more information, see NDC number formatting.
Note: To edit the NDC number or dosage for a procedure code, click the edit procedure fees link on the Fee Schedules page. |
| Drug name | The name of the drug. Unless entered manually, this field is populated automatically from your practice's fee schedule. |
| Unit price | The unit price that your practice paid for this drug. Unless entered manually, this field is populated automatically from your practice's fee schedule. |
| Dosage | The total amount dispensed, measured in the units selected in the menu to the right of the field. |
| Service Type Add-On — Newborn Care | |
| Patient's Weight (pounds) |
Enter the patient weight in pounds. |
| Service Type Add-On — No Surprises Act Consent | |
| Consented Amount ($) |
If a patient’s Out-of-Network Billing consented amount was entered in the appointment AND a signed consent form was attached, you’ll see that amount in this field.
Note: If no signed consent form was uploaded, the cost estimate will NOT carry over to the consented amount in Charge Entry, as it is assumed that the patient did not consent to paying Out-of-Network rates.
If a patient’s consented amount is missing at Charge Entry or Claim Edit: you can check the patient’s appointment to see if a signed consent form was attached, and then enter the consented amount.
For details, see the O-help topic: To view and edit patient's Out-of-Network Billing consented amount at Charge Entry or Claim Edit |
| Service Type Add-On — Ordering Provider | |
| Ordering Provider |
Provider ordering services or supplies if different from the rendering provider. You can type a period to access the Referring Provider Lookup tool. |
| Service Type Add-On — Paperwork | |
| Paper work |
Select Yes to indicate that additional documentation is required. |
| Attachment Control Number |
Enter a control number for the required attachment. |
| Attachment Type |
Select the type of paperwork attachment from the menu. |
| Attachment Transmission |
Select the means for transmitting the attachment paperwork. |
| Service Type Add-On — Podiatry | |
| Last Seen Date |
Enter the date last seen by the physician supervising care for the underlying condition. |
| Service Type Add-On — Post-Operative Care | |
| Assumed Care Date |
Enter the date care was assumed by another provider during post-operative care if the claim has Modifier 54 (for Surgical care only) or Modifier 55 (for post-operative care only). Required on Medicare claims involving shared post-operative care. See Relinquished Care Date (below). |
| Relinquished Care Date |
Enter the date that the provider filing the claim ceased post-operative care — (i.e., the last day of care by this provider) if the claim uses Modifier 54 (for Surgical care only) or Modifier 56 (for Pre-op management only). Required on Medicare claims involving shared post-operative care. See Assumed Care Date (above). |
| Service Type Add-On — Programs | |
| Program | Select the appropriate program from the menu. |
| Service Type Add-On — PT/OT | |
| Ordering Provider |
Select the provider ordering services or supplies if different from the rendering provider (Referring Provider Lookup tool available). |
| Date Last Seen |
Enter the date when patient was last seen by the ordering provider (above) who is supervising care for the underlying condition. |
| Service Type Add-On — Radiation Therapy | |
| Number of treatment sessions | Enter the number of radiation treatment sessions for the patient. |
| Supervising provider | Select the name of the supervising provider. |
| Interpreting provider | Select the name of the interpreting provider. |
| Number of patients served | Select the number of patients served from the menu. |
| Service Type Add-On — Reference Lab | |
| Reference Lab |
Select click the choose/view link in the Reference Lab service type add-on. Search by lab name or by CLIA number. If not found, click the add new referring provider link. |
| Service Type Add-On — Rehabilitation Services | |
| Ordering Provider |
Select the provider ordering services or supplies if different from the rendering provider (Referring Provider Lookup tool available). Required for procedure codes (HCPCS) that describe:
Medicare claims are placed in HOLD status if you have not entered either a referring provider and/or an ordering provider for the types of service described above. |
| Service Type Add-On — Spinal Manipulation | |
| Initial Treatment Date |
Date spinal manipulation services were initiated. |
| Last X-Ray Date |
Date last X-ray was taken (for example, to demonstrate a subluxation of the spine). |
| Spinal Man. Patient Condition |
Describes the nature of the patient's condition necessitating spinal manipulation.
CODE NAME A Acute Condition C Chronic Condition D Non-acute E Non-Life Threatening F Routine G Symptomatic M Acute Manifestation of a Chronic Condition |
| Spinal Man. Patient Condition Description |
Free-form description to clarify patient's spinal manipulation condition. |
| Acute Manifestation Date |
Date the patient's condition became acute. |
| Service Type Add-On — Telehealth | |
| Were services rendered via a live telehealth distant site visit? |
Select Yes or No. The Telehealth service type add-on appears only when the claim is created without an appointment. If an appointment is associated with the claim, the appointment should have the Telehealth Distant Site Visit appointment type class applied (see To add Telehealth Distant Site Visit to your available appointment types). Note: The athenahealth rules engine uses the Telehealth Distant Site Visit appointment type class or the Telehealth service type add-on information to identify the claim as telehealth and apply the appropriate billing rules per payer guidelines. |
| Service Type Add-On — Title X Family Planning | |
| English proficiency | Select Yes if an interpreter is needed. |
| Primary method of family planning | Select the patient's primary method of family planning. |
| Clinical breast exam (CBE) |
Select the Received option if the patient received a clinical breast exam during the visit. |
| Credited family planning encounter provider | Select the provider credited for the family planning encounter. |
| Service Type Add-On — UDS Reporting | |
| UDS Visit Type | Visit type selected by athenaOne based on procedure code and provider. |
| UDS Visit Type Override |
Select the override type from the menu. To exclude the visit from UDS reporting, select Non-UDS Visit from the menu. Note: The UDS STAO works only on claims. If you create a clinical encounter with no associated claim, athenaOne automatically flags the encounter as a UDS visit type for reporting, and you cannot change the visit type in athenaOne. Your UDS report details (filtered and raw files) will include all encounters, in addition to claims. |
| Clinic or Virtual |
Visit type (Clinic or Virtual) selected by athenaOne based on the department's place of service code (POS 02 - Telehealth), certain modifiers on procedure codes on the claim or encounter (.GT, .G0, or .95), or certain procedure codes. Virtual visits are reported on UDS Table 5 - Staffing and Utilization. Note: You can find the list of virtual-only procedure codes on the 2019 CPT inclusion and exclusion list on the Success Community. |
| Clinic or Virtual Override |
To override the value in the Clinic or Virtual field of the UDS STAO, select Clinic or Virtual from the menu. |
| Internal note | Enter a note to document the UDS visit override. |
| Service Type Add-On — Well Child Care | |
| EPSDT Referral Given? |
Indicates whether an EPSDT referral was given to the patient. |
| EPSDT Referral Reason |
Indicate reason why an EPSDT referral was given. Required if an EPSDT referral was given. |
| EPSDT Referral Reason |
Indicate second reason why an EPSDT referral was given. |
| EPSDT Referral Reason |
Indicate third reason why an EPSDT referral was given. |
| Claim Status | |
| Primary, Secondary, and Patient |
Primary, Secondary, and Patient indicate the responsible payer (primary insurance, secondary insurance, or the patient).
Note: If your practice is a no-posting or no-follow-up practice only, select DROP if you are requesting a proof of timely filing.
For additional information about claim status, see Claim Status. |
|---|---|
| Claim Details | |
| Service | |
| Date of service |
The date of service for the claim. The Date of service field must be populated before you can enter procedure and diagnosis information on the Charge Entry page. Note: If you arrive at the Charge Entry page through the appointment workflow, this field is pre-populated based on the appointment date. |
| Patient department |
The patient's current department of care, usually the department where the patient's chart resides. The default value is the patient's primary department as shown on the Quickview. This field is sometimes used to determine the contents of the 33A (PIN) (currently used only for Medi-Cal). |
| Facility |
This facility appears in Block 32 of the CMS-1500. It also determines the place of service code (CMS-1500 24B). |
| Insurance | |
| Primary payer |
Determines which policy this claim should be billed under. By default, the patient's current primary policy is displayed. Note: Deactivated payment plans do not appear in this menu unless the charge is currently assigned to that plan. You cannot assign the primary charge to a cancelled plan using this page.
For anesthesia claims generated from time sheets:
|
| Primary accepts assignment |
Indicates whether the provider accepts assignment of benefits from the primary payer for this claim and determines whether the Accept Assignment box will be checked off (CMS-1500 Block 27) for the primary claim.
|
| Force drop to paper for primary |
Select either:
Refer to Generate Claims for more information about generating "force drop to paper" claims.
Note: If your practice is a no-posting or no-follow-up practice only, select Yes-Athena if you are requesting a proof of timely filing. |
| Reason |
If Force drop to paper for primary is set to Yes-Athena, select a reason for the force-drop. Note: If your practice is a no-posting or no-follow-up practice only, select CSTPRFSUBM if you are requesting a proof of timely filing. |
| Primary print zero dollar charges? |
If set to Yes, indicates that any $0 charges should be included on the claim when it is printed or submitted electronically. This setting applies to charges of $0 and to outstanding balances for a charge that result in $0. If all charges on the claim are $0, the claim is set to DROP status (or HOLD status, if appropriate) until the claim is submitted, at which time the claim is closed. This option defaults to No. Note: If this field does not appear on the Charge Entry page and you want to use it, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center. |
| Secondary payer |
Determines which secondary policy this claim should be billed under. By default, the patient's secondary policy is displayed. If the patient has no secondary policy, defaults to No Insurance/Self Pay. |
| Secondary accepts assignment |
Indicates whether the provider accepts assignment of benefits from the secondary payer for this claim and determines whether the Accept Assignment box will be checked off (CMS-1500 Block 27) for the secondary claim.
|
| Force drop to paper for secondary |
If set to Yes, this claim will be submitted on paper to the secondary payer, even if the payer could accept it electronically. Refer to the Generate Claims page for more information about generating "force drop to paper" claims. |
| Reason |
If Force drop to paper for secondary is set to Yes, select a reason for the force-drop. |
| Authorization |
The authorization or referral number used for the services. Typically, this number is assigned by the payer or utilization management organization to authorize a service prior to its being rendered. |
| Add new authorization | |
| Notes |
Enter any notes about the authorization. These notes appear on the Insurance Authorization page. |
| Type |
Select Pre-cert or Referral. |
| Insurance authorization number |
Enter the insurance authorization number. |
| Effective date |
Enter or select the effective dates for this authorization or referral. |
| Authorized visits/units |
Select Visits or Units from the menu, and then enter the number of approved units or visits in both fields. athenaOne automatically decrements the number of authorized visits or units.
If you select units, a procedure code is required. The count of remaining units decreases by the number of units associated with the procedure codes listed in the authorization, regardless of any other charge on the claim. For example, you first create an authorization using units = 10 and a procedure code of 99215. You then create a claim using this authorization where procedure code 99215 bills for 3 units. The authorization decreases by 3, and the remaining units on that authorization are now 7. |
| Referred-to provider |
Select the provider to whom the patient is being referred. This field automatically displays the name of the provider with whom you are scheduling the appointment. |
| Specialty |
Select the specialty of the provider to whom the patient is being referred. |
| Diagnosis code |
Enter or select the diagnosis code associated with the authorization. You can type a period to access the Diagnosis Lookup tool in the ICD-10 fields. After you enter a diagnosis code, a description of the code is displayed to the right of it. Note: If the diagnosis code that you entered is not coded to the highest level of specificity, a warning appears next to the code. |
| Procedure code |
Enter or select the procedure codes associated with the referral. You can type a period to access the Procedure Lookup tool. After you enter a procedure code, a description of the code is displayed to the right of it. Note: The exact procedure code is required if you select Units from the Authorized visits/units menu. The procedure is validated against your fee schedule. |
| Additional information |
Enter any additional information that you want to record about this incoming authorization. |
| Signature on file for release of information |
Indicates whether the provider has on file a signed statement by the patient authorizing the release of medical data to other organizations. This field corresponds to CMS-1500 Block 12. |
| Signature on file for assignment of benefits |
Indicates whether the insured or authorized person authorizes the primary payer to assign benefits to the provider (that is, authorizes the payer to remit payment to the provider directly). This field corresponds to CMS-1500 Block 13. |
| Signature source |
Indicates how patient signatures (for release of information and assignment of benefits) were obtained and how they are being stored by the provider. This field defaults to Signed form for both HCFA-1500 block 12 & 13 on file.
To change the default value for this field, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center. |
| Reserved (10d) (remarks) |
This field is to be used for specific information required by a payer (for example, source code or TPL codes). |
| Reserved (19) (remarks) |
Use this field only for information that pertains to the entire CMS-1500 claim. Report charge-level information elsewhere. |
| Resubmission |
Box 22 on the CMS-1500 is labeled RESUBMISSION and has two data components:
|
| Provider | |
| Rendering provider | The provider who renders services to the patient. This field is typically used for internal tracking and reporting purposes; the selected provider will generally not appear as the rendering provider on the claim. |
| Supervising provider |
The provider whose credentials you intend to submit on the claim. This can be the provider who supervised the services or an individual who was supervised by another provider. In either case, use this field to identify the provider that you want to submit on the claim. The provider you select using the Supervising provider field typically appears as the rendering provider on the claim. For example, on a CMS-1500 claim form, the provider you select using the Supervising provider field typically appears in Box 24J, and the provider's name appears in Box 31. Note: If the selected Rendering provider has a supervising provider, a note appears next to the Supervising provider field.
If you arrive at the Charge Entry page through the appointment or missing slips workflow, the default selection in the Supervising provider - Required field is as follows:
Important: Any provider whose credentials you intend to submit on claims must be configured as a supervisory provider type on the Providers page so that you can select that provider using the Supervising provider field. For example, you cannot select a physician's assistant with a provider type of PA, but you can select a physician's assistant with a provider type of PASUP.
The provider selected as the Rendering provider appears by default as the Supervising provider if the Rendering provider is one of the following provider types:
See the Providers page for more information about rendering and supervising providers.
Note: If the supervising provider is non-participating with a payer listed on the claim, their non-participation status is indicated. |
| Scheduling provider | The provider or resource that was originally scheduled for this appointment. Principally recorded for reporting purposes, this provider does not generally appear on claims. |
| Referring provider |
The provider who referred this patient for services. You can click Find a provider to display the referring provider lookup tool. |
| Illness/Injury | |
| Current illness date |
The date of onset of the current illness. LMP = Date of last menstrual period. ED = Estimated date of delivery. If the EDD is given, the LMP is automatically calculated using the OB feature. |
| Same or similar illness date |
Enter or select the date that the patient had the same or a similar illness. Prints in CMS-1500 Block 15. |
| Hospitalization dates |
Enter the date range for the period when the patient was hospitalized as a result of the condition related to this claim. Prints in CMS-1500 Block 18. |
| Patient unable to work |
Enter the date range for the period when the patient was unable to work as a result of the condition related to this claim. Prints in CMS-1500 Block 16. |
| Patient's condition related to |
Select the condition that is related to the injury or illness: Employment, Another party responsible, or Accident. Note: If your practice has the "Date of Accident" feature enabled, a Date of Accident field may appear. You can record the accident date in this field. |
| Attachments | |
| Any attachments and placeholders for this claim are listed here. Click Manage attachments to add or edit attachments for this claim. | |
| Hold All Statements For This Patient? |
This field appears only when the patient has an outstanding balance. Although this field appears on the Claim Edit page, a statement hold is a property of the patient (not the claim). Therefore, if you select a reason to hold statements, athenaOne holds the entire statement, not just the charges associated with this claim. |
| Charges | |
| (NEW) Transaction History |
Use the (NEW) Transaction History page for additional visibility into how payments are posted across all charges for the claim, including a timeline view and details by procedure code. Note: The first release (March 2025) is only for non-FQHC customers and focuses on claims fully paid by the primary payer (Billed amount = Paid amount). We’ll continue to add more posting scenarios in upcoming releases. |
| Service Type add-ons |
Check the relevant checkboxes to display fields for each service type add-on used for this claim. Note: Please see the Service type add-ons field reference (above this field reference) for details about each service type add-on. |
| Diagnosis Codes (ICD-10) | |
| Diagnosis codes (ICD-10) |
The diagnosis codes that correspond to procedure codes for this claim. You can click the magnifying glass icon to access the athenaCodesource Code and Knowledge Base tool. The first four unique diagnoses, in order, are mapped to CMS-1500 blocks 21.1 through 21.4. |
| Procedures For each procedure on the claim, there is a shaded block with a bold text header showing the procedure code, description, and the date range that this service was provided. |
|
|---|---|
| Units |
Number of units. |
| Charges per | Per-unit charge for this charge line item. |
| Line note |
The line note that prints in the CMS-1500 shaded area over the charge line. This note should contain information that would pertain to a single charge on the claim (for example, notes for an unlisted procedure code). |
| Diagnosis | The diagnosis justifying this procedure. |
| Place of service |
The place of service (automatically determined from the facility). |
| COB | COB indicator. CMS-1500 24J. |
| EPSDT |
Indicates that this line item is for Early and Periodic Screening, Diagnostic, and Treatment (EPSDT). |
| EMG | EMG indicator. CMS-1500 24I. |
| FP |
Family Planning code; used for some Medicaid programs. |
| Allowed amount |
The total allowed amount (payments plus transfers) from the primary payer after the payment has been posted.
As long as a claim is not in a HOLD status, athenaOne attempts to calculate the Allowed amount for each charge as it is entered and saved. athenaOne uses the reimbursement method and the payment adjustments in the allowable schedule terms and conditions (ASTC) to price the charge. athenaOne updates estimated allowed amounts each night. If you make mid-day changes to an allowable schedule and/or the associated ASTCs, you can still prompt athenaOne to recalculate the estimated allowed amounts for all affected charges using the Payment Mismatch Tracking page. Otherwise, allowed amounts will be estimated each time the individual claim is saved. |
| Expected allowed amount |
The estimated allowed amount for the charge, as calculated by athenaOne, based on the allowable schedule and applicable terms and conditions. If athenaOne is unable to estimate the allowed amount of a service or procedure, –Unknown– appears in this column. |
| Difference |
The difference between the Expected allowed amount and the Allowed amount. Amounts above the expected allowable appear in blue. Amounts below the expected allowable appear in red.
Note: For allowable schedules with ASTCs, athenaOne automatically considers payments within +/- 5% of the expected allowed amount to be a match. For example, if your expected allowed amount is $100.00, payments between $98.00 and $103.00 are considered to be paid at the expected allowed amount. |
| Column headings for charge details Below each procedure block, there is a lightly shaded column header and grid showing the charge details for each procedure |
|
| Type | The type of transaction, for example, CHARGE, PAYMENT, ADJUSTMENT, TRANSFERIN, or TRANSFEROUT. |
| Payment Batch | The payment batch associated with this charge or transaction. |
| Reason/Method |
The type of adjustment, the transfer reason, or the current kick reason.
|
| Created | The date that the charge was created and the user or entity that created the charge. |
| Last Modified | The date that the charge was last modified and the user or entity that modified the charge. |
| Ins1 | The amount charged to the primary insurance. |
| Ins2 | The amount charged to the secondary insurance. |
| Patient | The amount charged to the patient. |
| Internal Use | |
| Other diagnoses |
Enter any other relevant diagnosis codes (for internal documentation only). |
| Note | Leave blank. On a paper claim, this information appears directly under dates of service and procedure codes. You should not use this field at all for CMS-1500 claims. |
| Column headings for Claim Notes | |
|---|---|
| Date |
The date the action occurred. |
| User |
The username of the person who took the action. AUTO indicates an automated system function. Usernames that belong to your practice appear in regular font, but athenahealth usernames are italicized. Perot users have the prefix "vhs" in front of their usernames. |
| Action |
The action taken on the claim. Highlighting indicates a system-generated action.
|
| Claim Status |
The status of the claim following this action. |
| Kick/Scrub/Note |
A brief note describing the action, generally including a kick reason. Notes that appear here also appear under the Claim Notes section of the Claim Review, , View Claims for Charge Entry Batch, and the View Claim History pages.
For older claim notes, click [expand text] to see the text as it appeared when the rule fired on the claim.
Claim rules:
The following types of claim notes are the result of claim rules. Note: To override a review claim note, you must have the Claim Note Override: Review role or permission. To override an advice claim note, you must have the Claim Note Override: Advice role or permission.
Note: An override link may also appear when a "predictive rule" fires. A predictive rule is a type of claim advice that uses historical data in athenaOne to predict likely denials, so that you can adjust them off to zero before they appear in your denial work queues. Predictive rules cover Medical Necessity Denials and Benefits Coverage (charges expected to be denied for a benefit limitation or exclusion).
Kick codes:
Each payer has its own denial codes. athenaOne associates different payer denial codes to the athenahealth standard set of kick codes, which determines the appropriate next steps.
Note: When you add a claim note that sets a claim alarm, athenaOne displays the date of the alarm beneath the text of the claim note. The date appears as long as the claim alarm remains active. Claim alarms are reset every time a claim note puts a claim in — or LEAVES a claim in — BILLED status. When claim acknowledgment applies an EMCRCVD or PAYORRCVD claim note, the original alarm is cleared and a new one is set.
Claim Status Inquiry transactions:
Note: CSI transactions are supported for athenaCollector clients only. For more information about CSI, please refer to Claim Status Inquiry. |
| Add Note | |
| Applies to | Select the payer type for this claim note. |
| Status | Select the new claim status. |
| Kick reason | Enter a kick reason for this claim note. |
| Note | Enter a note to describe why the note was added. |
| Post date |
The post date for the claim. |