 User Guide — PAMA AUC Requirements for Advanced Imaging Orders
User Guide — PAMA AUC Requirements for Advanced Imaging Orders
athenaClinicals + athenaCollector
athenaOne for Hospitals & Health Systems
Note: As announced in the CY 2024 Physician Fee Schedule (PFS) Final Rule, effective January 1, 2024, the Centers for Medicare & Medicaid Services (CMS) has paused efforts to implement the AUC program for reevaluation and rescinded the AUC regulations at 42 CFR 414.94. Providers and suppliers no longer need to include AUC consultation information on Medicare fee-for-service (FFS) claims.
For more details on the current status and background of the PAMA AUC regulation, see the following CMS article: Appropriate Use Criteria Program.
In response to this change, athenahealth is deprecating functionality for displaying PAMA AUC scores on orders in athenaClinicals and ending the PAMA AUC integration between athenaClinicals and Stanson Health, a qualified Clinical Decision Support Mechanism (qCDSM).
Currently, you can run the PAMA AUC Report and PAMA AUC Report - Hospital to assess compliance with the PAMA AUC regulation. These reports remain active in the Report Library and will be deprecated at a later time.
For more information, please see the Release Note.
We're preserving this article on the PAMA AUC program and functionality for your reference.
As part of the Protecting Access to Medicare Act (PAMA) of 2014, Congress included a requirement that ordering professionals must consult appropriate use criteria (AUC) when they order outpatient advanced imaging exams for patients with Medicare Part B coverage.
The Centers for Medicare & Medicaid Services (CMS) require ordering providers to consult a qualified Clinical Decision Support Mechanism (qCDSM) when they enter an advanced imaging order for a patient with Medicare Part B coverage.
- Open the advanced imaging order in the Assessment & Plan section of the exam, in an order group, or in the document view of an order in REVIEW status.
- Appropriateness Score — Stanson Health automatically sends an appropriateness score to athenaOne.
Note: Scoring information is automatically sent to the imaging center that provided the service along with the imaging order.- Adheres — The order adheres to the Appropriate Use Criteria guidelines. No further action is required. Your PAMA AUC consultation is complete.
- Does not adhere — The order does not adhere to the AUC guidelines. Review clinical guidance.
- Not applicable — The clinical indications for this exam do not fall within one of the eight Priority Clinical Areas from the CMS or there are no AUC guidelines for this order in the specific priority clinical area. This is a valid score.
- No score provided — Stanson Health needs additional clinical information to provide a score.
- If your order does not receive an AUC score that meets PAMA guidelines (Does not adhere or No score provided), the Decision Support panel appears to the right of your order, which provides clinical decision support (CDS) guidance from Stanson Health.
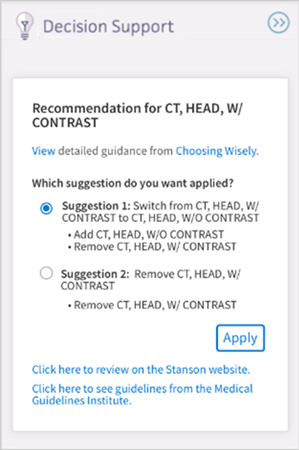
- Click Apply to apply the suggestion to the order.
- (Optional) Click Click here to review in the Stanson application to review the CDS guidance regarding the order.
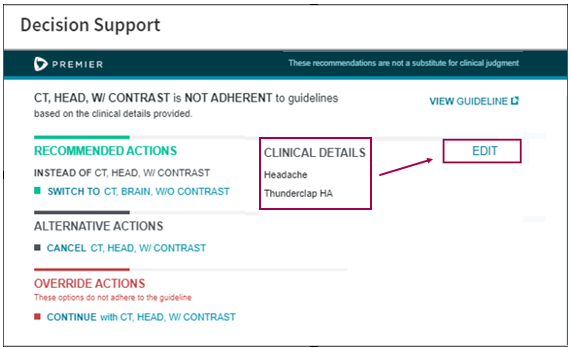
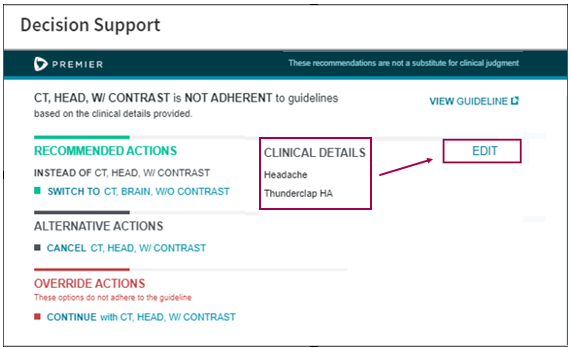
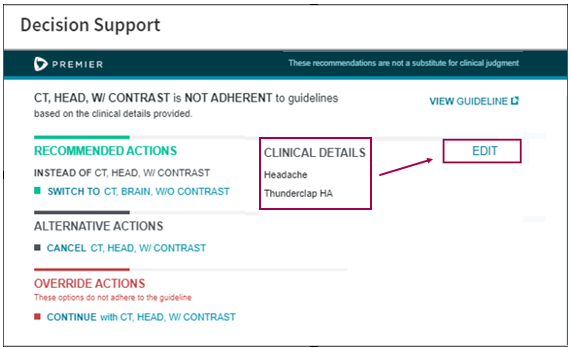
The Stanson Health application opens. - Review the CLINICAL DETAILS. To change or update them, click edit.
- Edit the clinical indications for your order.
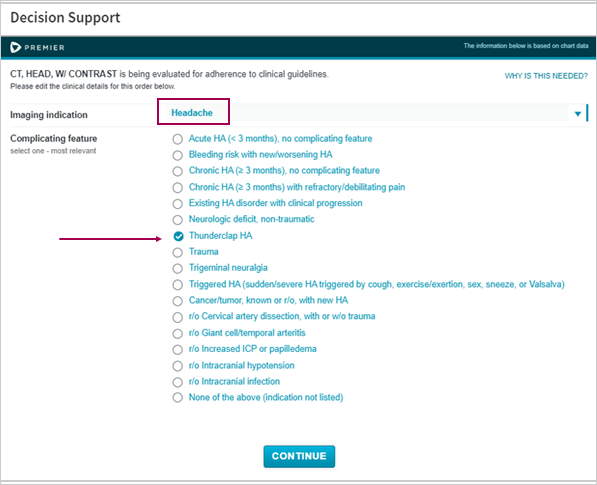
- Click CONTINUE.
Your clinical order is reevaluated and a new appropriateness score may be determined. - If your order receives a score of Does not adhere, recommended actions appear in the Stanson Health app.
- RECOMMENDED ACTIONS — Switch to an advanced imaging order that adheres to the AUC.
- ALTERNATIVE ACTIONS — Cancel the advanced imaging order.
- OVERRIDE ACTIONS — Continue with your advanced imaging order and provide an Override Reason to explain why.
Note: The Override Reason is currently not displayed in athenaOne. It is stored only in the Stanson application with the consultation details for audit purposes.
- Review the Decision Support to the right of your advanced imaging order. Stanson Health needs additional clinical information to determine the AUC score.
- Click Click here to review in the Stanson application.
- Respond to the questions in the Stanson Health CDS application so that Stanson can determine the appropriateness score.
- After you provide all the required clinical information, the Stanson application determines one of these appropriateness scores for the order:
- Adheres — The application automatically closes and the score for your order appears in athenaOne.
- Does not adhere — Three types of actions you can take on the order appear:
- RECOMMENDED ACTIONS — Switch to an advanced imaging order that adheres to the AUC.
- ALTERNATIVE ACTIONS — Cancel the advanced imaging order.
- OVERRIDE ACTIONS — Continue with your advanced imaging order and provide an Override Reason to explain why.
Note: The Override Reason is currently not displayed in athenaOne. It is stored only in the Stanson application with the consultation details for audit purposes.
- Enter an advanced imaging order.
- Appropriateness Score — If you cannot obtain an Appropriateness Score for an advanced imaging order, select a reason to indicate why:
- Not required — Patient with suspected or confirmed emergency medical condition
- Not required — Insufficient Internet access
- Not required — EHR or clinical decision support vendor issues
- Not required — Extreme and uncontrollable circumstances
- Display the advanced imaging order.
- Click MANUALLY REPLACE SCORE.
- Click Replace.
Note: All score-related information is erased when you choose to manually replace the score. - Appropriateness Score — Select an appropriateness score for the order. See Appropriateness Score determined by qCDSM for a description of each score.
- Scored by — The qualified Clinical Decision Support Mechanism that determines the appropriateness score.
- HCPCS modifier — The modifier associated with each appropriateness score to enter on the Charge Entry page.
Note: athenaOne displays this information automatically, based on the appropriateness score you add to the order. - Consultation ID — The unique consultation identifier that provides a reference to details of the qCDSM consultation.
Important: If you click CANCEL, athenaOne erases your entries and "None recorded" appears in the Appropriateness Score field.
You can use the PAMA AUC report to identify gaps in information across all advanced imaging orders so you can address them prior to qCDSM review. This report shows information related to all advanced imaging orders related to Medicare patients.
- On the Main Menu, click Reports. Under General, click Report Library.
- Click the Clinicals tab.
- Click run next to PAMA AUC Report.
- Date Range — Enter the start and end dates for the report, or select a date range from the menu.
Note: The longer the Date Range, the longer the report takes to run. - Departments — Select All or Selected.
- Report Format — Select the format for your report results.
- HTML table — Display the report results on your screen.
- Text (tab-delimited) — Export the report results to a .csv file in tab-delimited format.
- Text (comma-delimited) — Export the report results to a .csv file in comma-delimited format.
- Report Options — Select report options.
- Suppress Column Headings — Select this option to remove column headings from the report results.
- Suppress Report Name — Select this option to remove the report name from the report results.
- Show Filter Criteria — Select this option to include your selected filter criteria in the report results.
- Run Offline (will appear in your Report Inbox tomorrow morning) — Select this option for very long reports. Reports that are run offline appear in your Report Inbox the morning after the request.
- Click Run Report.
- Review the PAMA AUC Report.
Left columns — Show information about department, provider, patient, and document.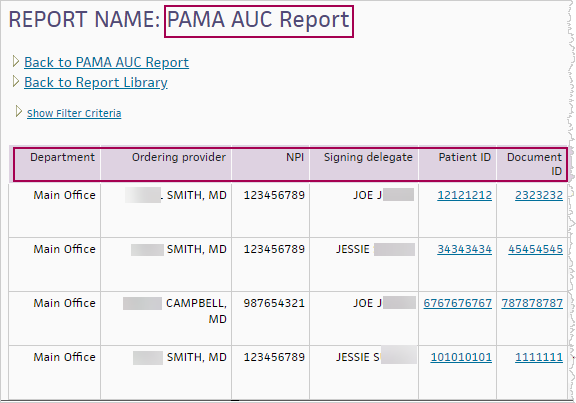
Middle columns — Show information about the order and diagnosis.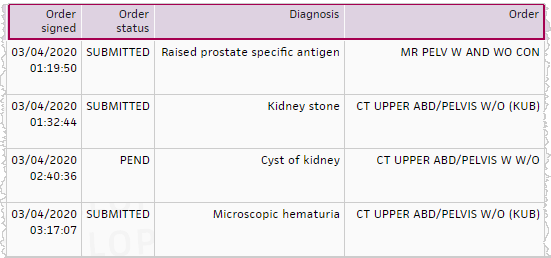
Right columns — Show information from the qCDSM.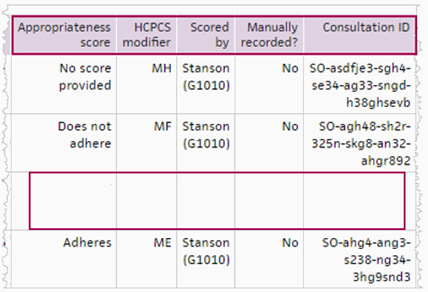
Note: Notice that some information in the third row, for the CT UPPER ABD/PELVIS W W/O, is missing. Use the report to identify gaps so you can address them.
When billing Medicare Part B, you are required to enter certain HCPCS modifiers and G‑codes during charge entry for an advanced imaging service that has an appropriate use criteria (AUC) score on the order.
- HCPCS modifiers — MA through MH and QQ represent the AUC appropriateness score.
Note: The QQ modifier is a generic modifier that will not meet the billing requirements for PAMA AUC compliance as of January 1, 2021. - G-codes — G1000 through G1011 represent the clinical decision support (CDS) vendors that determine the appropriateness score.
Note: For detailed information, see Appropriate Use Criteria (AUC) for Advanced Diagnostic Imaging – Educational and Operations Testing Period - Claims Processing Requirements on CMS.gov.
If your organization created and fulfilled the order for advanced imaging, the HCPCS modifier and G-code information appears in these locations:
- Assessment & Plan section of the exam
- Order group
- Document view (for orders in REVIEW status)
- Post-discharge orders (athenaOne for Hospitals & Health Systems only)
If your organization fulfilled the order and a different organization created the order, follow your organization's preferred workflow for obtaining information from the ordering provider and storing it with the patient's record of services in athenaOne (for example, the Quickview or patient chart).
- Review the card in the Decision Support panel that provides CDS guidance.
- Select and apply a Suggestion from Stanson.
If you choose to switch to a different advanced imaging order, the order automatically appears in athenaOne and the Appropriateness Score for the new order is Adheres.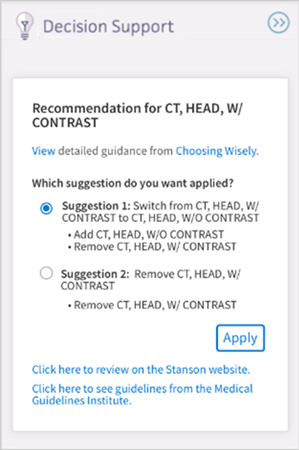
You can send PAMA consultation details to furnishing (or fulfilling) providers via outbound interfaces. This integration minimizes manual data entry required when an order is sent electronically via an interface between athenaOne and another organization, such as an imaging center.
Note: See the HL7v2 - ORM specifications on the developer portal to view the PAMA AUC imaging order standards.
If you want to send PAMA AUC information via interface to furnishing, or fulfilling, providers, contact your Customer Success Manager to open an integration request.
- Open the advanced imaging order in the Assessment & Plan section of the exam, in an order group, or in the document view of an order in REVIEW status.
- Appropriateness Score — Stanson Health automatically sends an appropriateness score to athenaOne.
Note: Scoring information is automatically sent to the imaging center that provided the service along with the imaging order.- Adheres — The order adheres to the Appropriate Use Criteria guidelines. No further action is required. Your PAMA AUC consultation is complete.
- Does not adhere — The order does not adhere to the AUC guidelines. Review clinical guidance.
- Not applicable — The clinical indications for this exam do not fall within one of the eight Priority Clinical Areas from the CMS or there are no AUC guidelines for this order in the specific priority clinical area. This is a valid score.
- No score provided — Stanson Health needs additional clinical information to provide a score.
- If your order does not receive an AUC score that meets PAMA guidelines (Does not adhere or No score provided), the Decision Support panel appears to the right of your order, which provides clinical decision support (CDS) guidance from Stanson Health.
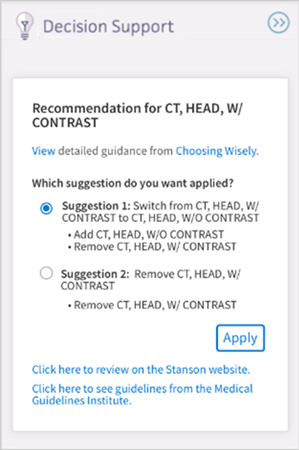
- Click Apply to apply the suggestion to the order.
- (Optional) Click Click here to review in the Stanson application to review the CDS guidance regarding the order.
The Stanson Health application opens. - Review the CLINICAL DETAILS. To change or update them, click edit.
- Edit the clinical indications for your order.
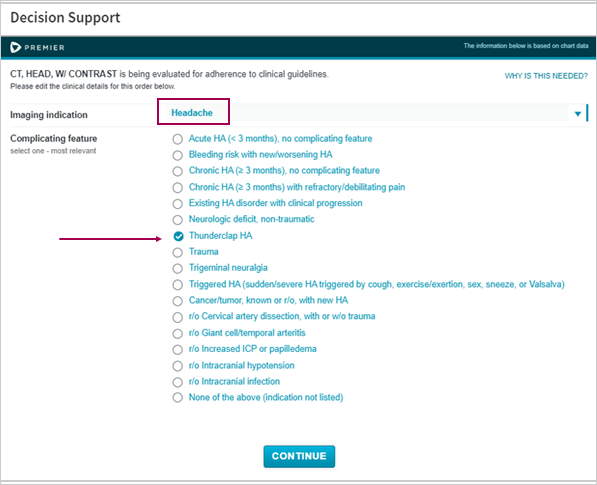
- Click CONTINUE.
Your clinical order is reevaluated and a new appropriateness score may be determined. - If your order receives a score of Does not adhere, recommended actions appear in the Stanson Health app.
- RECOMMENDED ACTIONS — Switch to an advanced imaging order that adheres to the AUC.
- ALTERNATIVE ACTIONS — Cancel the advanced imaging order.
- OVERRIDE ACTIONS — Continue with your advanced imaging order and provide an Override Reason to explain why.
Note: The Override Reason is currently not displayed in athenaOne. It is stored only in the Stanson application with the consultation details for audit purposes.
- Review the Decision Support to the right of your advanced imaging order. Stanson Health needs additional clinical information to determine the AUC score.
- Click Click here to review in the Stanson application.
- Respond to the questions in the Stanson Health CDS application so that Stanson can determine the appropriateness score.
- After you provide all the required clinical information, the Stanson application determines one of these appropriateness scores for the order:
- Adheres — The application automatically closes and the score for your order appears in athenaOne.
- Does not adhere — Three types of actions you can take on the order appear:
- RECOMMENDED ACTIONS — Switch to an advanced imaging order that adheres to the AUC.
- ALTERNATIVE ACTIONS — Cancel the advanced imaging order.
- OVERRIDE ACTIONS — Continue with your advanced imaging order and provide an Override Reason to explain why.
Note: The Override Reason is currently not displayed in athenaOne. It is stored only in the Stanson application with the consultation details for audit purposes.
- Enter an advanced imaging order.
- Appropriateness Score — If you cannot obtain an Appropriateness Score for an advanced imaging order, select a reason to indicate why:
- Not required — Patient with suspected or confirmed emergency medical condition
- Not required — Insufficient Internet access
- Not required — EHR or clinical decision support vendor issues
- Not required — Extreme and uncontrollable circumstances
- Display the advanced imaging order.
- Click MANUALLY REPLACE SCORE.
- Click Replace.
Note: All score-related information is erased when you choose to manually replace the score. - Appropriateness Score — Select an appropriateness score for the order. See Appropriateness Score determined by qCDSM for a description of each score.
- Scored by — The qualified Clinical Decision Support Mechanism that determines the appropriateness score.
- HCPCS modifier — The modifier associated with each appropriateness score to enter on the Charge Entry page.
Note: athenaOne displays this information automatically, based on the appropriateness score you add to the order. - Consultation ID — The unique consultation identifier that provides a reference to details of the qCDSM consultation.
Important: If you click CANCEL, athenaOne erases your entries and "None recorded" appears in the Appropriateness Score field.
You can use the PAMA AUC report to identify gaps in information across all advanced imaging orders so you can address them prior to qCDSM review. This report shows information related to all advanced imaging orders related to Medicare patients.
- On the Main Menu, click Reports. Under General, click Report Library.
- Click the Clinicals tab.
- Click run next to PAMA AUC Report.
- Date Range — Enter the start and end dates for the report, or select a date range from the menu.
Note: The longer the Date Range, the longer the report takes to run. - Departments — Select All or Selected.
- Report Format — Select the format for your report results.
- HTML table — Display the report results on your screen.
- Text (tab-delimited) — Export the report results to a .csv file in tab-delimited format.
- Text (comma-delimited) — Export the report results to a .csv file in comma-delimited format.
- Report Options — Select report options.
- Suppress Column Headings — Select this option to remove column headings from the report results.
- Suppress Report Name — Select this option to remove the report name from the report results.
- Show Filter Criteria — Select this option to include your selected filter criteria in the report results.
- Run Offline (will appear in your Report Inbox tomorrow morning) — Select this option for very long reports. Reports that are run offline appear in your Report Inbox the morning after the request.
- Click Run Report.
- Review the PAMA AUC Report.
Left columns — Show information about department, provider, patient, and document.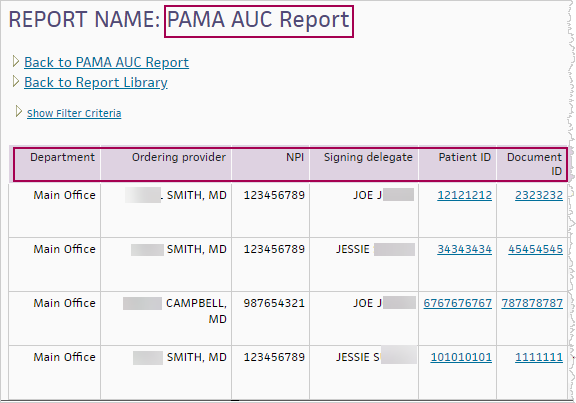
Middle columns — Show information about the order and diagnosis.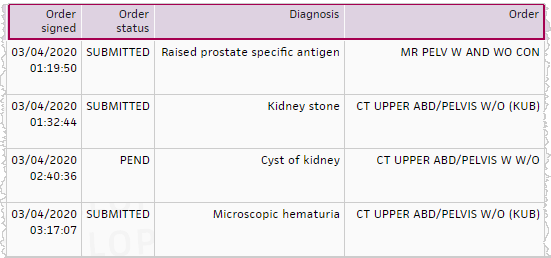
Right columns — Show information from the qCDSM.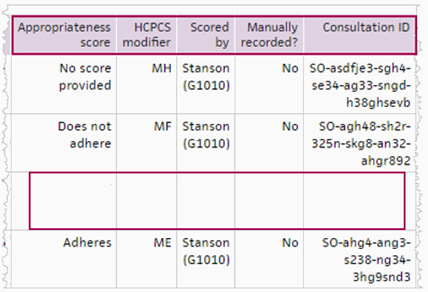
Note: Notice that some information in the third row, for the CT UPPER ABD/PELVIS W W/O, is missing. Use the report to identify gaps so you can address them.
When billing Medicare Part B, you are required to enter certain HCPCS modifiers and G‑codes during charge entry for an advanced imaging service that has an appropriate use criteria (AUC) score on the order.
- HCPCS modifiers — MA through MH and QQ represent the AUC appropriateness score.
Note: The QQ modifier is a generic modifier that will not meet the billing requirements for PAMA AUC compliance as of January 1, 2021. - G-codes — G1000 through G1011 represent the clinical decision support (CDS) vendors that determine the appropriateness score.
Note: For detailed information, see Appropriate Use Criteria (AUC) for Advanced Diagnostic Imaging – Educational and Operations Testing Period - Claims Processing Requirements on CMS.gov.
If your organization created and fulfilled the order for advanced imaging, the HCPCS modifier and G-code information appears in these locations:
- Assessment & Plan section of the exam
- Order group
- Document view (for orders in REVIEW status)
- Post-discharge orders (athenaOne for Hospitals & Health Systems only)
If your organization fulfilled the order and a different organization created the order, follow your organization's preferred workflow for obtaining information from the ordering provider and storing it with the patient's record of services in athenaOne (for example, the Quickview or patient chart).
These instructions apply to practices and non-critical access hospitals (CAH) that order or bill for advanced imaging tests and the Hospital Outpatient and Hospital Emergency departments.
- Open the advanced imaging order in the Assessment & Plan section of the exam, in an order group, or in the document view of an order in REVIEW status.
- Appropriateness Score — Stanson Health automatically sends an appropriateness score to athenaOne.
Note: Scoring information is automatically sent to the imaging center that provided the service along with the imaging order.- Adheres — The order adheres to the Appropriate Use Criteria guidelines. No further action is required. Your PAMA AUC consultation is complete.
- Does not adhere — The order does not adhere to the AUC guidelines. Review clinical guidance.
- Not applicable — The clinical indications for this exam do not fall within one of the eight Priority Clinical Areas from the CMS or there are no AUC guidelines for this order in the specific priority clinical area. This is a valid score.
- No score provided — Stanson Health needs additional clinical information to provide a score.
- If your order does not receive an AUC score that meets PAMA guidelines (Does not adhere or No score provided), the Decision Support panel appears to the right of your order, which provides clinical decision support (CDS) guidance from Stanson Health.
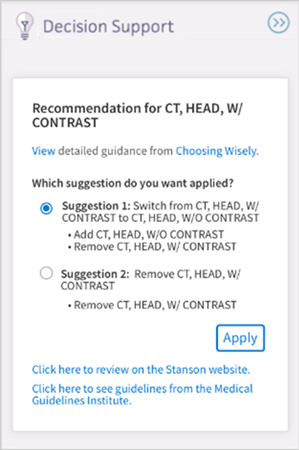
- Click Apply to apply the suggestion to the order.
- (Optional) Click Click here to review in the Stanson application to review the CDS guidance regarding the order.
The Stanson Health application opens. - Review the CLINICAL DETAILS. To change or update them, click edit.
- Edit the clinical indications for your order.
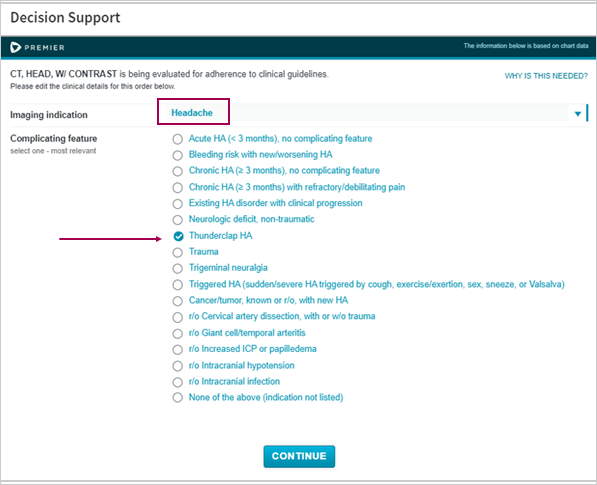
- Click CONTINUE.
Your clinical order is reevaluated and a new appropriateness score may be determined. - If your order receives a score of Does not adhere, recommended actions appear in the Stanson Health app.
- RECOMMENDED ACTIONS — Switch to an advanced imaging order that adheres to the AUC.
- ALTERNATIVE ACTIONS — Cancel the advanced imaging order.
- OVERRIDE ACTIONS — Continue with your advanced imaging order and provide an Override Reason to explain why.
Note: The Override Reason is currently not displayed in athenaOne. It is stored only in the Stanson application with the consultation details for audit purposes.
- Review the Decision Support to the right of your advanced imaging order. Stanson Health needs additional clinical information to determine the AUC score.
- Click Click here to review in the Stanson application.
- Respond to the questions in the Stanson Health CDS application so that Stanson can determine the appropriateness score.
- After you provide all the required clinical information, the Stanson application determines one of these appropriateness scores for the order:
- Adheres — The application automatically closes and the score for your order appears in athenaOne.
- Does not adhere — Three types of actions you can take on the order appear:
- RECOMMENDED ACTIONS — Switch to an advanced imaging order that adheres to the AUC.
- ALTERNATIVE ACTIONS — Cancel the advanced imaging order.
- OVERRIDE ACTIONS — Continue with your advanced imaging order and provide an Override Reason to explain why.
Note: The Override Reason is currently not displayed in athenaOne. It is stored only in the Stanson application with the consultation details for audit purposes.
- Enter an advanced imaging order.
- Appropriateness Score — If you cannot obtain an Appropriateness Score for an advanced imaging order, select a reason to indicate why:
- Not required — Patient with suspected or confirmed emergency medical condition
- Not required — Insufficient Internet access
- Not required — EHR or clinical decision support vendor issues
- Not required — Extreme and uncontrollable circumstances
- Display the advanced imaging order.
- Click MANUALLY REPLACE SCORE.
- Click Replace.
Note: All score-related information is erased when you choose to manually replace the score. - Appropriateness Score — Select an appropriateness score for the order. See Appropriateness Score determined by qCDSM for a description of each score.
- Scored by — The qualified Clinical Decision Support Mechanism that determines the appropriateness score.
- HCPCS modifier — The modifier associated with each appropriateness score to enter on the Charge Entry page.
Note: athenaOne displays this information automatically, based on the appropriateness score you add to the order. - Consultation ID — The unique consultation identifier that provides a reference to details of the qCDSM consultation.
Important: If you click CANCEL, athenaOne erases your entries and "None recorded" appears in the Appropriateness Score field.
You can use the PAMA AUC report to identify gaps in information across all advanced imaging orders so you can address them prior to qCDSM review. This report shows information related to all advanced imaging orders related to Medicare patients.
- On the Main Menu, click Reports. Under General, click Report Library.
- Click the Clinicals tab.
- Click run next to PAMA AUC Report.
- Date Range — Enter the start and end dates for the report, or select a date range from the menu.
Note: The longer the Date Range, the longer the report takes to run. - Departments — Select All or Selected.
- Report Format — Select the format for your report results.
- HTML table — Display the report results on your screen.
- Text (tab-delimited) — Export the report results to a .csv file in tab-delimited format.
- Text (comma-delimited) — Export the report results to a .csv file in comma-delimited format.
- Report Options — Select report options.
- Suppress Column Headings — Select this option to remove column headings from the report results.
- Suppress Report Name — Select this option to remove the report name from the report results.
- Show Filter Criteria — Select this option to include your selected filter criteria in the report results.
- Run Offline (will appear in your Report Inbox tomorrow morning) — Select this option for very long reports. Reports that are run offline appear in your Report Inbox the morning after the request.
- Click Run Report.
- Review the PAMA AUC Report.
Left columns — Show information about department, provider, patient, and document.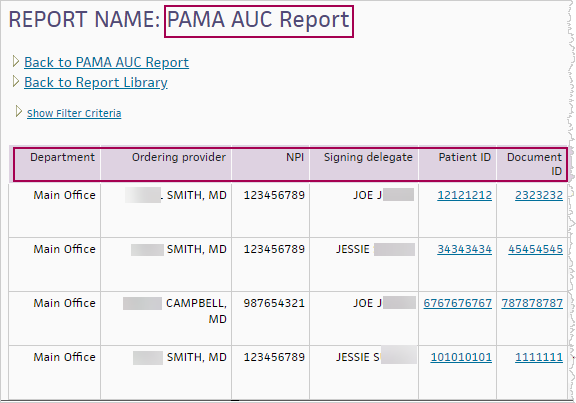
Middle columns — Show information about the order and diagnosis.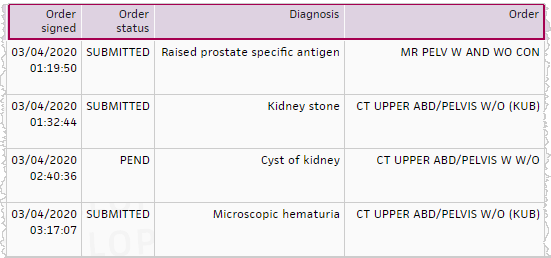
Right columns — Show information from the qCDSM.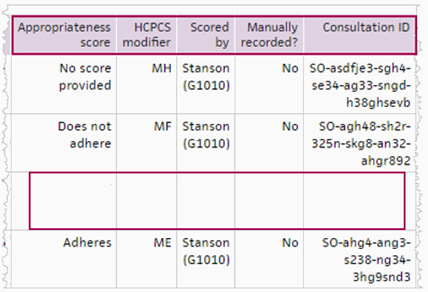
Note: Notice that some information in the third row, for the CT UPPER ABD/PELVIS W W/O, is missing. Use the report to identify gaps so you can address them.
When billing Medicare Part B, you are required to enter certain HCPCS modifiers and G‑codes during charge entry for an advanced imaging service that has an appropriate use criteria (AUC) score on the order.
- HCPCS modifiers — MA through MH and QQ represent the AUC appropriateness score.
Note: The QQ modifier is a generic modifier that will not meet the billing requirements for PAMA AUC compliance as of January 1, 2021. - G-codes — G1000 through G1011 represent the clinical decision support (CDS) vendors that determine the appropriateness score.
Note: For detailed information, see Appropriate Use Criteria (AUC) for Advanced Diagnostic Imaging – Educational and Operations Testing Period - Claims Processing Requirements on CMS.gov.
If your organization created and fulfilled the order for advanced imaging, the HCPCS modifier and G-code information appears in these locations:
- Assessment & Plan section of the exam
- Order group
- Document view (for orders in REVIEW status)
- Post-discharge orders (athenaOne for Hospitals & Health Systems only)
If your organization fulfilled the order and a different organization created the order, follow your organization's preferred workflow for obtaining information from the ordering provider and storing it with the patient's record of services in athenaOne (for example, the Quickview or patient chart).
CMS established the PAMA AUC program to reduce spending on and patient exposure to inappropriate utilization of advanced imaging tests. CMS further elaborates that "the primary goal for the PAMA AUC program is to increase the rate of appropriate advanced diagnostic imaging services provided to Medicare beneficiaries."
As part of the Protecting Access to Medicare Act (PAMA) of 2014, Congress included a requirement that ordering professionals must consult appropriate use criteria (AUC) when they order outpatient advanced imaging exams for patients with Medicare Part B coverage.
Note: For more information, see this FAQ on the Success Community: Protecting Access to Medicare Act (PAMA) Appropriate Use Criteria (AUC) Program.
The Centers for Medicare & Medicaid Services (CMS) requires ordering providers to consult a qualified Clinical Decision Support Mechanism (qCDSM) when they enter an advanced imaging order for a patient with Medicare Part B coverage.
- Ordering providers can record the qCDSM consultation details in the order.
- athenaOne sends the qCDSM consultation details to the provider that fulfills the order.
Note: This feature applies only to patients who are covered by Medicare Part B. If you want to enable this feature for all your patients, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
The following advanced imaging orders qualify for PAMA AUC:
- Computed tomography (CT)
- Positron emission tomography (PET)
- Nuclear medicine
- Magnetic resonance imaging (MRI)
Note: These imaging services are explicitly excluded from the PAMA AUC mandate: X-ray, ultrasound, mammography, and fluoroscopy.
The PAMA AUC regulation applies to providers who order advanced imaging services and providers who furnish and fulfill advanced imaging orders.
January 1, 2020
- Learning period begins for providers who order and provide advanced imaging.
- No financial penalties if the advanced image does not meet appropriate use criteria.
January 1, 2023
- Penalty phase begins. Based on a provider's behavior, a financial impact may be applied if the advanced image does not meet acceptable use criteria.
- Claims must include additional details. The CMS states that "Information regarding the ordering professional's consultation with the qCDSM, or exception to such consultation, must be appended to the furnishing professional's claim in order for that claim to be paid."
- CMS begins to audit providers. Providers who do not meet PAMA AUC regulations could be required to obtain prior authorization for advanced imaging orders in 2022 or 2023.
Note: Integrated PAMA AUC scores are automatically set to appear only for patients who have Medicare insurance. If you want the Appropriateness Score fields and the PAMA AUC integration to appear for all advanced imaging orders regardless of a patient's insurance at the time of order entry, contact the CSC.
- Open the advanced imaging order in the Assessment & Plan section of the exam, in an order group, or in the document view of an order in REVIEW status.
- Appropriateness Score — Stanson Health automatically sends an appropriateness score to athenaOne. The order receives one of the following scores:
- Adheres — The order adheres to the Appropriate Use Criteria guidelines. No further action is required. Your PAMA AUC consultation is complete.
- Does not adhere — The order does not adhere to the AUC guidelines. Review clinical guidance.
- Not applicable — The clinical indications for this exam do not fall within one of the eight Priority Clinical Areas from the CMS or there are no AUC guidelines for this order in the specific priority clinical area. This is a valid score.
- No score provided — Stanson Health needs additional clinical information to provide a score.
- HCPCS modifier — The HCPCS modifier based on your appropriateness score.
Note: You enter this modifier on the Charge Entry page. - Scored by — Stanson Health appears in this field as the athenahealth integrated qCDSM vendor.
- Consultation ID — The consultation ID obtained from your qCDSM vendor. This unique ID provides a reference to details of the qCDSM consultation.
- If your order does not receive an AUC score that meets PAMA guidelines (Does not adhere), a Decision Support panel appears to the right of your order, which provides clinical decision support (CDS) guidance from Stanson Health.
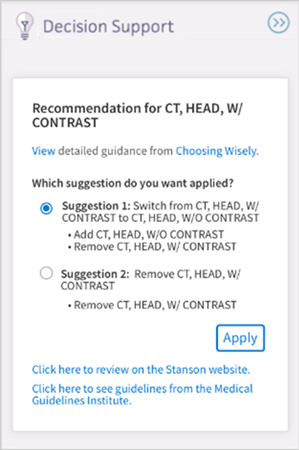
- Optional: Select a suggestion from the Decision Support panel. Suggestions show different order types that would meet PAMA appropriateness criteria.
- Click Apply to apply the suggestion to your order.
- Click Click here to review in the Stanson CDS application to review the CDS guidance regarding the order.
Important: The ordering workflow is never blocked in athenaOne, even if the AUC score does not meet PAMA guidelines.
The PAMA AUC Report shows the following information:
- Advanced imaging order details for each order to which PAMA applies from every provider
- Consultation details for each advanced imaging order from the qCDSM
- Code, the HCPCS modifier, required for the claim
Run this report to see if all advanced imaging orders contain the data required by PAMA AUC regulations. The report helps to ensure that, by 2021, claims will not be denied and the practice will not risk financial penalties for non-compliance.
When ordering providers place an advanced imaging order for Medicare Part B patients, they must consult a qualified Clinical Decision Support Mechanism (qCDSM). Evidence-based AUC for imaging can assist clinicians in selecting the imaging study that is most likely to improve health outcomes for patients based on their individual clinical presentation.
The qCDSM determines whether the advanced imaging order meets AUC guidelines and provides an appropriateness score, as follows.
- Adheres — The order adheres to the Appropriate Use Criteria guidelines. No further action is required. Your PAMA AUC consultation is complete.
- Does not adhere — The order does not adhere to the AUC guidelines. Review clinical guidance.
- Not applicable — The clinical indications for this exam do not fall within one of the eight Priority Clinical Areas from the CMS or there are no AUC guidelines for this order in the specific priority clinical area. This is a valid score.
- No score provided — The qCDSM needs additional clinical information to provide a score.
You can view the appropriate use criteria score and related information when you create an advanced imaging order. The Appropriateness Score information appears in these locations:
- Assessment & Plan section of the exam
- Order group
- Document view (for orders in REVIEW status)
- Post-discharge orders (athenaOne for Hospitals & Health Systems only)
In athenaOne, you must enter the following information in the Appropriateness Score section of the order:
- Appropriateness Score — The qCDSM determines the AUC score.
- Adheres — The order adheres to the Appropriate Use Criteria guidelines. No further action is required. Your PAMA AUC consultation is complete.
- Does not adhere — The order does not adhere to the AUC guidelines. Review clinical guidance.
- Not applicable — The clinical indications for this exam do not fall within one of the eight Priority Clinical Areas from the CMS or there are no AUC guidelines for this order in the specific priority clinical area. This is a valid score.
- No score provided — The qCDSM needs additional clinical information to provide a score.
- HCPCS modifier — The modifier associated with each AUC score to enter on the Charge Entry page.
Note: athenaOne displays the HCPCS modifier automatically based on the AUC score associated with the order. - Scored by — The qualified Clinical Decision Support Mechanism (qCDSM) that determines the appropriateness score. All organizations that use athenaClinicals (Ambulatory) will see Stanson (Stanson Health) in this field.
- Consultation ID — The unique consultation identifier that provides a reference to details of the qCDSM consultation.
The AUC information also appears on orders that you:
- Send by athenaFax
- Send via interface between athenaOne and another organization such as an imaging center
When billing Medicare Part B, you are required to enter certain HCPCS modifiers and G‑codes during charge entry for an advanced imaging service that has an appropriate use criteria (AUC) score on the order.
- HCPCS modifiers — MA through MH and QQ represent the AUC appropriateness score.
Note: The QQ modifier is a generic modifier that will not meet the billing requirements for PAMA AUC compliance as of January 1, 2021. - G-codes — G1000 through G1011 represent the clinical decision support (CDS) vendors that determine the appropriateness score.
Note: For detailed information, see Appropriate Use Criteria (AUC) for Advanced Diagnostic Imaging – Educational and Operations Testing Period - Claims Processing Requirements on CMS.gov.
If your organization created and fulfilled the order for advanced imaging, the HCPCS modifier and G-code information appears in these locations:
- Assessment & Plan section of the exam
- Order group
- Document view (for orders in REVIEW status)
- Post-discharge orders (athenaOne for Hospitals & Health Systems only)
If your organization fulfilled the order and a different organization created the order, follow your organization's preferred workflow for obtaining information from the ordering provider and storing it with the patient's record of services in athenaOne (for example, the Quickview or patient chart).
CMS created new modifiers and G‑codes for reporting appropriate use criteria (AUC) when a facility performs advanced diagnostic imaging services for Medicare Part B beneficiaries. If your organization bills claims to Medicare Part B for advanced diagnostic imaging services, you can start coding claims with these new codes in 2020 (you are not required to do so until 2021).
To meet the billing requirements for PAMA AUC compliance, you must:
- Add the HCPCS modifiers MA through MH and QQ on the Procedure Code Modifiers page.
Note: The QQ modifier is a generic modifier that will not meet the billing requirements for PAMA AUC compliance as of January 1, 2021. - Add G-codes G1000 through G1011 on the Procedure Fees page.
The PAMA consultation details for outbound interfaces to furnishing, or fulfilling, providers are available. See the HL7v2 - ORM specifications on the developer portal to view the PAMA AUC imaging order standards.
If you would like to be able to send PAMA AUC information via interface to furnishing, or fulfilling, providers, contact your Customer Success Manager to open an integration request.
Using the integration will minimize manual data entry required when an order is sent electronically, via an interface between athenaOne and another organization such as an imaging center. athenahealth offers a few standard integration solutions, but custom solutions could be available if needed. Note that delivery timelines will be faster to implement a standard interface solution and that custom interface solutions could incur additional cost.
athenahealth is initiating a proactive review of orders likely to be affected by the PAMA AUC regulation. Some of your advanced imaging orders could have an unclear order name that does not allow for mapping to the athenahealth global advanced imaging order compendium. You can leave these orders unmapped, but they will not be sent to Stanson Health for a PAMA AUC consultation.
If you notice that PAMA AUC consultation information for an advanced imaging order for a Medicare Part B patient is not populated automatically, create a case from athenaOne > Support > Success Community > Contact Client Support Center.
You can check the mapping of an order by reviewing the CLINICALORDERTYPEID in the order's audit history. To find the audit history, you must sign the order. Then click VIEW DOCUMENT. In the bottom right corner, click Audit History. If the mapping is UNKNOWN, create a case for the Clinical Content team.