 User Guide — Capitation
User Guide — Capitation
You are required to report to us your capitation payments and link them to the services they cover using the Capitation Wizard in athenaOne.
Capitation contracts are contracts between a third-party administrator (usually an IPA) and an individual provider, a group of providers, a department, or a medical practice. Capitation contracts represent an alternative to traditional fee-for-service contracts. Under capitation contracts, providers are reimbursed based on the number of patients served by the provider ("covered lives"), rather than for the specific medical services provided to patients (fee for service). Capitation contracts may cover specific sets of CPT codes for specific insurance packages and may apply to particular providers or departments.
Capitation payments are lump sum, monthly payments received as reimbursement under a capitation contract. The reimbursement amount is based on the number of covered lives, rather than for the specific medical services provided to patients.
Strictly speaking, capitation payments cannot be "posted" to claims because they do not represent fees for individual services, and so cannot be applied to specific open charges. Instead, capitation payments should be recorded in athenaOne as unpostable amounts — with an unpostable type of "Capitation Payment" — in payment batches and deposit batches.
To record a capitation payment, athenahealth recommends that you first create one capitation policy for each capitation contract used in your practice. A capitation policy is the athenaOne term for a set of components that define a capitation contract to the system. Use the Capitation Wizard page to define capitation policies.
You should route capitation checks to athenahealth so that our staff can record them in athenaOne.
Note: For athenaCollector (No Posting clients), refer to the Capitation Payments page for detailed steps to record a capitation payment in athenaOne.
Recording capitation payments in athenaOne makes it easier to reconcile athenaOne with bank statements at month-end. It gives you a single place in which to compare the payments received for capitation against the fee-for-service payments forgone as a result of the capitation agreement. This makes it possible to use athenaOne utilities to help you evaluate the financial performance of your practice under the capitation plan. To evaluate your capitation contracts, use the Capitation Payments page.
athenaOne treats capitation payments as unpostable amounts. Capitation payments appear as unpostable items in the Find Unpostables worklist and report, but they do not appear as posted payments on the Activity Wizard report.
After you record a capitation payment, you can track and update the item using the Find Unpostables, Remittance Record, and Capitation Payments pages.
Charges that are covered by capitation contracts are handled by posting capitated adjustments and contractual adjustments that equal the charge amount. There are two ways to accomplish this:
- If a capitation payment EOB comes back while the charge is open, you can manually post the entire balance as a capitated adjustment.
- You can set up the Capitation Wizard to let athenaOne identify capped charges and calculate capitated adjustments according to an allowable schedule.
athenahealth always sends capitation claims to the payer. Cap adjustments are created nightly for claims that are in BILLED status. This procedure ensures that the claims are sent out once before writing them off.
The Capitation Wizard is an athenaOne utility that runs nightly. It identifies any BILLED charges covered by a capitation policy and creates automatic adjustments to write off the charges.
Important: For the Capitation Wizard to work correctly, you must create a capitation policy for each capitation contract in effect for your practice. (Use the Capitation Wizard page to define capitation policies.)
- If the claim contains only capitated charges, the wizard should create the capitation adjustments and then transfer the expected copay amounts to the next responsible party.
- If the claim contains both capitated charges and non-capitated (fee-for-service) charges, the Capitation Wizard creates the capitation adjustment only for charges that are covered under the capitation contract. The Capitation Wizard suppresses the immediate transfer of the copay to the secondary, so that when the primary payer adjudicates the fee-for-service charges and submits the remittance advice, the secondary claim is processed normally.
For primary claims, when you create a capitation policy, any matching charges that are still in BILLED status are "capped" according to the new capitation policy, regardless of the age of the charge. Any new matching charges are also capped.
Are capped procedures billed with full charges, or do they show a $0 charge?
They are billed at the full charge amount. The Capitation Wizard then applies the capitation adjustments, leaving a $0 balance.
If a capped charge is resubmitted for some reason, what happens?
If the claim is resubmitted, the charges covered by a capitation policy do not appear unless another transaction voided the capitation adjustment. For example, acknowledgment kicks and EOB denials both void the capitation adjustment. But if there is no void, the charges are not included on the claim when it is resubmitted.
If you edit or delete a capitation policy, the changes to the capitation policy apply only to future charges — BILLED status charges are not affected by the capitation policy edits. athenaOne does not re-evaluate BILLED status charges after they are capped.
Allowable schedules and capitation contracts
If an allowable schedule has been created for the payer, the Capitation Wizard:
- Creates a contractual adjustment equal to the difference between the charge amount and the allowable amount (from the allowable schedule)
- Creates a transfer in the amount of the expected copay (if a copay is expected for this charge)
- Creates a capitated adjustment equal to the remaining charge balance
If an allowable schedule has not been created for the payer, the Capitation Wizard:
- Creates a capitation adjustment — the copay amount is deducted, then the capitation adjustment is created to cover the remainder of the charge amount
- Creates a transfer in the amount of the expected copay (if a copay is expected for this charge)
You can reconcile the charges included in your monthly service invoice with the capitation payments posted in athenaOne using the Capitation Payments report:
- Display the Capitation Payments page: From the Main menu, click Financials > Capitation Payments.
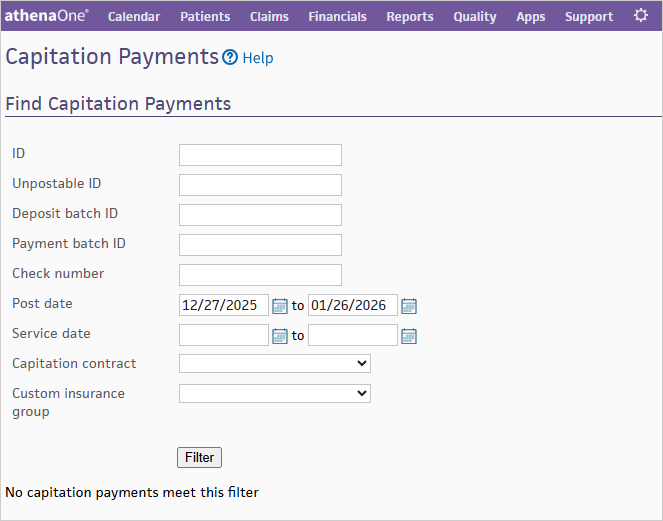
- Enter your filter criteria to search for specific Capitation Payment matching results.
- Click Run Report.
| Unpostable ID |
Click the linked unpostable ID to display the Remittance Record page for the capitation payment. |
|---|---|
| Payment Batch ID |
Click the linked payment batch ID to display the Edit Payment Batch page for the payment batch associated with the capitation payment. |
| Provider Group Name |
Name of the provider group associated with the capitation payment. |
| Provider Group ID |
ID of the provider group associated with the capitation payment. |
| Provider Name |
Name of the provider associated with the capitation payment. |
| Unpostable Post Date |
Date that the capitation payment was posted. |
| Unpostable Amount |
Amount of the capitation payment. |