Authorization Management - Tasks athenahealth Processes Report
athenaCollector + athenaClinicals
athenaOne for Hospitals & Health Systems
The Authorization Management - Tasks athenahealth Processes report lists all authorization management tasks that athenahealth has processed and is processing for your organization if you use the athenaOne Authorization Management add-on service. For more information about athenaOne Authorization Management, see Authorization Tracker.
Note: Authorization tasks that are closed by the rules engine are not included in this report.
Display the Report Library: On the Main Menu, click Reports. Under General, click Report Library. Click the Other tab. In the Standard Reports section of the tab, click run next to Authorization Management - Tasks athenahealth Processes.
To run this report, you must have one of the following permissions or roles:
- Practice Superuser role
- Report Reader role
- Report: Report Library: Other permission
Note: To activate the Authorization Management - Tasks athenahealth Processes report, use the Activate Reports page.
- Display the Report Library: On the Main Menu, click Reports. Under General, click Report Library.
- Click the Other tab.
- Click run next to Authorization Management - Tasks athenahealth Processes in the Standard Reports section of the tab.
The Run Report: Authorization Management - Tasks athenahealth Processes page appears. - From date - To date — Enter or select the date range for the report. All authorization tasks with a date of service within the specified date range are included in the report.
- Report Format — Select the format for your report results.
- HTML table — Display the report results on your screen.
- Text (tab-delimited) — Export the report results to a .csv file in tab-delimited format.
- Text (comma-delimited) — Export the report results to a .csv file in comma-delimited format.
- Report Options — Select report options.
- Suppress Column Headings — Select this option to remove column headings from the report results.
- Suppress Report Name — Select this option to remove the report name from the report results.
- Show Filter Criteria — Select this option to include your selected filter criteria in the report results.
- Run Offline (will appear in your Report Inbox tomorrow morning) — Select this option for very long reports. Reports that are run offline appear in your Report Inbox the morning after the request.
- Click Run Report.
The Authorization Management - Tasks athenahealth Processes report lists all authorization management tasks that athenahealth has processed and is processing for your organization if you use the athenaOne Authorization Management add-on service.
Note: The CURRENTSTATUS column indicates the status of an authorization task. Tasks with a status of IN PROGRESS are still being processed by athenahealth.
Authorization tasks that are closed by the rules engine are not included in this report. The rules engine closes authorization tasks when it determines that the associated order does not require authorization. If the rules engine cannot confidently automate a "not required" determination for an authorization task, the authorization management service contacts the payer directly.
Note: If you have any questions about your implementation of athenaOne Authorization Management, please contact your Customer Success Manager.
athenaOne® Authorization Management is an optional add-on service for organizations that use both the athenaCollector and athenaClinicals services (the service is included in athenaOne for Hospitals & Health Systems).
With athenaOne Authorization Management, athenahealth completes authorization work for you, including:
- Obtaining precertification to perform future services
- Logging referrals with payers, based on payer requirements
- Following up with payers to continually check on the status of the authorization
The Authorization Tracker displays the progress of your authorization tasks and each interaction with payers.
- athenahealth manages requests for additional documentation and assigns tasks to you only when absolutely necessary or when a conversation is needed.
-
You can locate orders that require authorization using the filters on the Authorization Tracker page, or you can locate the order from the patient chart.
Note: This page documents authorizations (precertifications) and referrals; we refer to these items collectively as "authorizations."
- Orders that require authorization include an embedded authorization status window at the top of the order document.
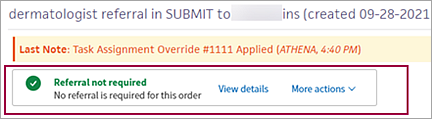
- You can click View details to open the detailed authorization or referral status window and:
- Learn why an authorization is in its current status.
- Enter missing information or fix incorrect information to resolve a problem.
- Edit an authorization.
- Cancel an authorization.
- Ask athenahealth to review an authorization.
- athenaOne guides you through the steps you need to take to resolve any issues with authorization tasks
![]() Demo video — Guided Authorization Experience
Demo video — Guided Authorization Experience
If an authorization has not been started or needs additional information to proceed, this window supplies customized instructions and information.This information depends on the type of authorization and the information that is needed.
![]()
To edit or resubmit an authorization, you can click More actions in the authorization status window at the top of the order document, or you can click the More actions menu in the detailed authorization status window.
![]()
The options available in the More actions menu depend on the status of the authorization or referral.
- Edit authorization — Edit the full authorization as needed. For example, you can update insurance information, update the estimated start date, or add and remove procedure codes.
- Attach documentation — If the authorization requires additional documentation, you can attach documentation from the patient chart (see To add a document from the patient chart to an authorization).
Note: This option appears in the More actions menu only when appropriate. - Request review — Request that athenahealth review the authorization. Select a reason for the requested review and enter a message for athenahealth (for example, you think athenahealth incorrectly marked the authorization as unsupported).
- View history — View a full list of the actions taken on the authorization task. The authorization status details window appears, with the History section to the left of it.
- Authorization tracker — Select this option to return to the Authorization Tracker page.
- Cancel authorization — Select a reason for the cancellation and enter a message for athenahealth explaining why.
- Refresh authorization — Use this option to update the authorization if you have completed additional work on it.
Note: athenaOne does not create authorizations for orders that were created before the go-live date for athenaOne Authorization Management.
Authorization tasks are assigned a status. Following is a list of authorization statuses with examples of when these statuses apply (not all reasons are shown).
- Needs practice attention: Waiting to start — athenahealth has not started authorization work on this task. The authorization task is on hold and requires action on your part, for example, if a task is missing a clinical provider, requested date of service, requested service length, or requested procedure codes, or if the order has not been signed.
- Needs practice attention: Action required — athenahealth started authorization work on this task, but you need to take additional actions, for example, obtaining a referral from the PCP or adding an insurance plan. The authorization task is on hold and requires action on your part.
- Needs practice attention: Denied — The authorization task is denied and requires your review.
- In progress with athenahealth — athenahealth is working on this authorization task. No action is needed from you at this time.
- Approved — The payer approved the authorization task and the patient is ready to have the procedure.
- Not required — Authorization (precertification or referral) is not required as determined by the payer guidelines established for this procedure, diagnosis, and service length.
- Not supported by athenahealth — The provider, insurance, or facility is ineligible for athenaOne Authorization Management, or your organization excluded the provider, insurance, or facility from Authorization Management.
- Canceled — The procedure was canceled and no further action is required.
Note: Tasks with the status "Needs practice attention: Action required" that are 60 days past their date of service are automatically cancelled. - Denial reviewed by practice — The authorization for the procedure was denied; your practice has reviewed the denial. The authorization is still marked as Not complete so that you can take action on the denial.
| Run Report: Authorization Management - Tasks athenahealth Processes Report | |
|---|---|
| From date - To date |
Enter or select the date range for the report. All authorization tasks with a date of service within the specified date range are included in the report. Note: If your fiscal year does not align with the calendar year, you can select date ranges for the fiscal year or the calendar year, for example, Fiscal Quarter-to-Date, Previous Fiscal Year, Previous Calendar Quarter, or Calendar Year thru Previous Month. |
| Report Format |
Select the format for your report results.
|
| Report Options |
Select other options for your report results.
|
| Column Headings | |
| ORDERID |
Unique document ID of the order. You can click the linked ID number to display the order document. |
| AUTHTASKID |
Unique document ID of the authorization task associated with the order. You can click the linked ID number to display the authorization task.
An authorization task is the electronic document shared between athenahealth and your organization and is used to record the information required for the authorization work. |
| AUTHTASKCREATED |
Date that the authorization task was created. |
| DATEOFSERVICE |
Date of service for the test, procedure, surgery, or consult documented in the authorization task. |
| ORDERINGPROVIDER |
Provider that ordered the test, procedure, surgery, or consult documented in the authorization task. |
| DEPARTMENT |
Department in which the order that triggered the authorization task was created. |
| ORDER_GROUP |
Order type group of the order documented in the authorization task: CONSULT, IMAGING, PROCEDURE, or SURGERY. Note: The order type group in the report corresponds to the selections available from the Order type filter field on the Authorization Tracker page. |
| ORDER_NAME |
Name of the order type documented in the authorization task. |
| INSURANCE |
Primary insurance company to which the authorization or precertification request was submitted. |
| COMPLETED_DATE |
For authorization tasks that are not in progress, date that the authorization was approved, cancelled, or deemed not required. Note: For descriptions of task statuses, see Authorization statuses. |
| CURRENTSTATUS |
Current status of the authorization task, for example, APPROVED, IN PROGRESS, NOT REQUIRED, or CANCELLED. Note: For descriptions of task statuses, see Authorization statuses. |
| SENDERHOLDS |
Number of times that the authorization task was set to the status "Needs practice attention: Action required." |
| PEER_TO_PEER_YN |
Indicates whether the task was set to the status "Needs practice attention: Action required" because the authorization required a peer-to-peer review with the insurance company (Y = Yes; N = No). |
| AUTHORIZATIONDENIALYN |
Indicates whether this authorization has been denied (Y = Yes; N = No). |
| CANCELLEDYN |
Indicates whether this authorization has been cancelled (Y = Yes; N = No). |