 Quick Reference — To correct CPT claims
Quick Reference — To correct CPT claims
Worklist: HOLD
Issue: The Payer has indicated that a problem has been identified with the CPT/HCPCS code(s) on the claim. The procedure code (CPT or HCPCS) is not acceptable for this payer, or the CPT code has been deleted or contains a modifier that the payer deems unnecessary. Although the procedure code and modifier may each be valid codes to a payer, an incompatible combination of the two can cause the payer to deny the procedure code as invalid.
Note: athenahealth does not provide coding advice. Instead, please consult the Code and Knowledge Base for more coding information.
Next Steps: Review the EOB (if available) for additional information. The recommended Best Practice is to use the Validate Codes tool. Make the necessary coding corrections and resubmit the claim. You can also attach documentation to support the initial coding selection and ask athenahealth to appeal the claim, or you can transfer the balance to patient responsibility.
- Update diagnosis and/or procedure codes and resubmit the claim
- Request athenahealth to appeal the claim
- Transfer the balance
Note: If after acting on this error, the claim remains in a hold status (HOLD or MGRHOLD), the claim requires additional review or work.
- Display the Claim Action page: Select a claim from the Workflow Dashboard, Claim Worklist, or click the Claim Action Page link on the Claim Edit page.
- Review the claim information.
- Actions — Select Update Codes.
- Diagnosis Codes (ICD-10) — Add, update, and delete diagnosis codes as needed. You can apply these codes to the charge lines below. Type a period (.) to use the lookup tool.
- Add, update, and delete procedure codes and modifiers on the charge lines as needed.
Note: You can edit the Units field, if needed. - Select diagnosis codes on the charge lines as needed.
- Claim note — Enter a claim note to describe the changes you made and why.
- Click Submit Claim.
athenaOne applies the DRPBILLING kick code to the claim and moves the claim to athenahealth to review for payer-specific requirements.
- Display the Claim Action page: Select a claim from the Workflow Dashboard, Claim Worklist, or click the Claim Action Page link on the Claim Edit page.
- Review the claim information and existing documentation.
- Actions — Select Resubmit to Payer from the menu.
The Resubmission request page appears.
Note: You can only submit one resubmission request at a time. If you have an on-going request, you cannot access the resubmission workflow until the pending one is resolved. - Applies to — Select the payer whose denial you are appealing: Primary Insurance or Secondary Insurance.
- Resubmission type — Select a resubmission type from the menu.
- Under Optional information, enter the following information if applicable for your resubmission request:
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
Notes:- Documents that are already attached to the claim appear in the Existing Attachments section. These documents are available for athenahealth teams to use when constructing a resubmission, and do not need to be reattached via this workflow.
- You can upload only one document via the resubmission workflow. To upload multiple documents, please complete that workflow on the claim itself before coming to this page. Uploading the documents prior to completing the new resubmission workflow allows those documents to be part of the documentation that athenahealth teams select from.
- The Attachment type field sets the type of document you are attaching; it does not filter the medical documentation check boxes located in the Documents section.
- Mail-to address — Click Choose a mail-to address to expand the section. If you don’t see the appropriate address, click add a new mail-to address and enter a new address.
Best practice: To look for additional addresses, search for the address in the Find address field. - Reason for resubmission — Enter the reason for resubmitting the claim.
Note: This field has a 2000-character limit. - Claim note — Click Include claim note (internal) to expand the section. Enter any internal notes for your athenaOne practice users. Describe the reasons why the claim should be appealed, list facts to support the appeal, and indicate whether you attached any supporting documentation or faxed any documentation to athenahealth (you may want to do so).
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
- Click Submit request. This action applies the PLSPPEAL kick code and moves the claim to athenahealth to review for payer-specific requirements.
A message appears indicating that the resubmission was successfully submitted to athenahealth.
Important: We've built automation for highly predictable resubmission scenarios: When the claim is kicked with PLSAPPEAL, athenaOne automatically executes a resubmission based on the appropriate scenario. (We’re actively building tools that limit the effects of this automation by resubmission type. If you disagree with athenaOne’s automation for the resubmission, submit a case via the Success Community: Main Menu > Support > Contact Client Support Center > Billing & Claims > Correct/Resubmit Claim > Create Online Case.) - An address validation window may appear if the address you entered could not be verified. Choose the address you want to use by selecting either Correct Address or You Entered, and then Confirm address.
- Display the Claim Action page: Select a claim from the Workflow Dashboard, Claim Worklist, or click the Claim Action Page link on the Claim Edit page.
- Review the claim information.
- Actions — Select Transfer Balance.
- Select the charges that you want to adjust.
- Transfer to — Select Patient or Next Payer.
Note: Both options map to kick reasons, so reporting is unaffected. - Claim note — Enter a claim note to indicate why the balance is being transferred.
- Click Submit. Claims with a balance transferred to Patient are kicked with PTRESP; claims with a balance transferred to Next Payer are kicked with NEXTPAYOR.
Note: At least one change must be made to the claim before it can be resubmitted. It is not compliant to resubmit a claim without changes only to see whether the claim will be paid if you resubmit it to the payer.
- On the Claim Edit page, scroll down to the Claim Notes section at the bottom of the page.
- Review the claim notes.
- If athenahealth has researched the denial with the payer, a detailed description is included.
- If there is an EOB or letter from the payer, click the link to review it.
- If further clarification is needed, contact the payer directly.
- Applies to — Select the correct insurance type.
- Status — Select DROP.
- Kick reason — Enter DRPBILLING.
- Claim note — Enter a clear, detailed note for athenaOne users, describing what actions have just been taken.
- Click Save.
- Display the Claim Edit page:
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions..
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.. - Review the claim information and existing documentation.
- In the Add note section, click Resubmit to Payer.
The Resubmission request page appears.
Note: You can only submit one resubmission request at a time. If you have an on-going request, you cannot access the resubmission workflow until the pending one is resolved. - Applies to — Select the payer whose denial you are appealing: Primary Insurance or Secondary Insurance.
- Resubmission type — Select a resubmission type from the menu.
- Under Optional information, enter the following information if applicable for your resubmission request:
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
Notes:- Documents that are already attached to the claim appear in the Existing Attachments section. These documents are available for athenahealth teams to use when constructing a resubmission, and do not need to be reattached via this workflow.
- You can upload only one document via the resubmission workflow. To upload multiple documents, please complete that workflow on the claim itself before coming to this page. Uploading the documents prior to completing the new resubmission workflow allows those documents to be part of the documentation that athenahealth teams select from.
- The Attachment type field sets the type of document you are attaching; it does not filter the medical documentation check boxes located in the Documents section.
- Mail-to address — Click Choose a mail-to address to expand the section. If you don’t see the appropriate address, click add a new mail-to address and enter a new address.
Best practice: To look for additional addresses, search for the address in the Find address field. - Reason for resubmission — Enter the reason for resubmitting the claim.
Note: This field has a 2000-character limit. - Claim note — Click Include claim note (internal) to expand the section. Enter any internal notes for your athenaOne practice users. Describe the reasons why the claim should be appealed, list facts to support the appeal, and indicate whether you attached any supporting documentation or faxed any documentation to athenahealth (you may want to do so).
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
- Click Submit request. This action applies the PLSPPEAL kick code and moves the claim to athenahealth to review for payer-specific requirements.
A message appears indicating that the resubmission was successfully submitted to athenahealth.
Important: We've built automation for highly predictable resubmission scenarios: When the claim is kicked with PLSAPPEAL, athenaOne automatically executes a resubmission based on the appropriate scenario. (We’re actively building tools that limit the effects of this automation by resubmission type. If you disagree with athenaOne’s automation for the resubmission, submit a case via the Success Community: Main Menu > Support > Contact Client Support Center > Billing & Claims > Correct/Resubmit Claim > Create Online Case.) - An address validation window may appear if the address you entered could not be verified. Choose the address you want to use by selecting either Correct Address or You Entered, and then Confirm address.
- On the Claim Edit page, scroll down to the Claim Notes section at the bottom of the page.
- Review the claim notes.
- If athenahealth has researched the denial with the payer, a detailed description is included.
- If there is an EOB or letter from the payer, click the link to review it.
- Scroll down to the Add Note section.
- Applies to — If needed, select the payer type for the claim note: Primary Insurance or Secondary Insurance.
- Status — Do not change the status.
- Kick reason — Enter PLSAPPEAL.
- Note — Enter a note about the appeal.
Important: To assist athenahealth users who are finalizing your appeal package, please clearly label and differentiate between your appeal note (payer facing) and your internal claim note, for example: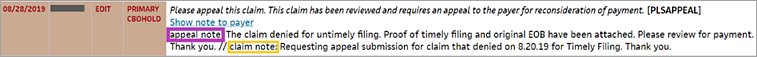
- Click Save.
- On the Claim Edit page, scroll down to the Claim Notes section at the bottom of the page.
- Review the claim notes.
- Action Taken/Note Source — Select Generic Note/From Other Source.
- Kick Reason — Select PTRESP.
- Claim Note — Enter a note to indicate why the balance is being transferred to the patient.
- Click Save. A statement will be sent to the patient.
The athenaOne Rules Engine uses athenaCodesource to check the effective and termination dates of a procedure code against the claim's from and to dates.
If a procedure code was not valid on the date of service, the claim is assigned HOLD status for the reason: "Rule #3864 Invalid Procedure Code for Date of Service." This message appears in the Claim Notes section of the Claim Edit and Claim Action pages.
- Display the Code Check page: On the Main Menu, click Claims. Under RESOURCES, click Code Check. The tool appears in the Task Bar.
- Select a Function — Select CPT/CCI.
- Enter all the CPT codes on the claim in the fields provided. Do not enter modifiers that are on the claim.
- Select the CCI version that matches the date of service on the claim.
You can click the CCI version link to display a table of dates and versions to help you determine the version. - Click Submit. An analysis of the coding of that specific claim appears in the Workspace.
Note: The analysis reveals only bundling issues on the claim and includes modifiers that can resolve the bundling issues. Any modifiers that you use must be supported by the medical record. Because the analysis addresses only bundling issues, there may be other reasons why a modifier is recommended. - Determine which modifier to use. For every code that has a MISMOD message, click the M link to the right of the code description. A list of possible modifiers and their descriptions appears in a new window.
Note: You can use only modifiers that appear in your modifier table in athenaOne. If a modifier is not in your table, please add it to the table before trying to correct the claim. - To print the MedAssets analysis, right-click the page and select Print. To return to the claim, right-click and select Back.