 User Guide — Claim Rules
User Guide — Claim Rules
In athenaOne, rules are short passages of computer code that are triggered by various attributes of a claim and take action on that claim.
Rules are short passages of computer code that are triggered by various attributes of a claim and take action on that claim. Rules are triggered by almost any combination of diagnosis, procedure-code/modifier, place of service, rendering or supervising provider, payer, patient demographics, or patient eligibility status.
Rules can change a claim's status, moving it into one of the athenaOne "buckets," such as HOLD or MGRHOLD. Rules can also:
- Post overridable warnings on claims
- Change the claim's electronic or paper format
- Create a link to a claim attachment that you faxed or uploaded into athenaOne
- Split a claim into institutional and professional components, or into two separate professional claims
In addition to triggers and actions, claim rules have scope, that is, some rules are global, and other rules are local or custom.
Global rules are written by athenahealth and attached to a benefit package ("insurance package" in athenaOne); global rules are triggered when any practice creates a claim destined for that insurance package. Global rules require payer documentation. Global rules can originate from athenahealth research, athenahealth denial management activity, government mandate (such as HIPAA or NPI), Medicare's Correct Coding Initiative (CCI) edits, or at your request, with supporting documentation.
Predictive rules are overridable and are derived automatically from denial trends from all claims in athenaOne. If you override a predictive rule, you can choose to submit the claim anyway but adjust off the balance (because you don't expect payment).
Posting rules are written by athenahealth to allow more accurate transaction and denial posting. athenahealth normally posts according to the remittance information; however, in some situations, a literal interpretation of the remittance data will lead to inaccurate posting. A posting rule overrides the literal interpretation so that the correct transaction or denial is reflected on the claim.
Local rules are requested by you and written by athenahealth, if the request is deemed by athenahealth to be legally and contractually compliant. A rule is made local in scope when there is not sufficient documentation to support it being global. Sometimes athenahealth promotes one or more of your local rules to global rules.
athenaOne allows users in your practice who have the Billing Admin: Custom Rules user permission to create custom rules for these specific circumstances:
- Procedures that require modifiers
- Procedures that require authorizations/referrals
- Procedures that require coding review
- Procedures with invalid diagnosis codes
- Procedures with invalid modifiers
- Non-billable procedures
Custom rules are a type of claim rule that allow you to move claims into HOLD or MGRHOLD based on criteria specific to your practice, and also have the option to allow override.
Because you specify the conditions of these custom rules, they are not put through our normal testing process. Therefore, it is possible to create conflicts with global rules in the athenaOne Rules Engine. Because a great deal of research goes into our Rules development process, we do not override global rules if such a conflict exists unless written documentation from the payer can be provided to update the logic within a specific global rule.
About custom rules
You can create custom rules to review claims for general completeness and accuracy, but you should use caution if you create custom rules. To avoid unnecessary holds on claims, make sure that you create rules with the narrowest scope possible and with clear instructions. Following are our recommendations for custom rules:
- Instead of creating a custom rule for a payer requirement not covered by a global rule, create a support case so that we can scope a global rule. On the Main Menu, click Support > Success Community > Contact Client Support Center.
- Make sure that only a trained, designated person or small team at your practice creates and monitors your custom rules.
- Review your custom rules quarterly to determine whether you can delete rules or conditions that no longer apply.
- If a potential athenaCollector feature could eliminate your need for a custom rule, please visit the Ideas page of the Success Community.
You can override individual custom rules or every custom rule of the same category on the Claim Edit page. One claim note appears for each custom rule that is holding the claim.
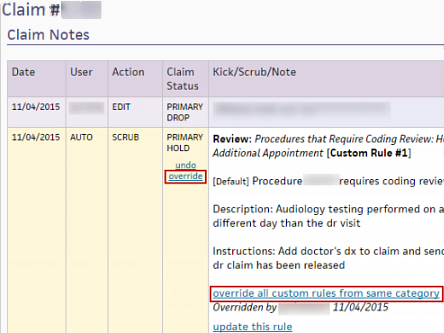
- To override a single custom rule, click the override link in the Claim Status column of the claim note.
- To override all custom rules of the same type (for example, all custom rules created on the Custom Rule: Invalid Modifiers page), click the override all custom rules from same category link in the claim note.
Note: This link appears only if overlapping custom rules fire on the same claim.
Note: This option is only available for the custom rule category Procedures that Require Coding Review for now. Based on feedback, we will determine whether to add this option to other custom rule types.
When this option is selected, the custom rule will not re-fire on a claim if it has already been overridden once. The override persists, even if the claim is closed and reopened or the conditions of the claim change.
- You can use this feature for both new rules and existing rules in this rule category.
- This option is selected by default for new rules.
- The undo override link will NOT be available in the claim note for Custom Rules using the Fire Only Once feature. If you need to undo an override in this situation, you can turn off the Fire Only Once feature for the Custom Rule
The Additional Procedure Code Filter and Additional Procedure Code Group Filter allow you to Hold claims based on a combination of procedure codes present on the same claim.
- To use the Additional Procedure Code Filter filter, you must also use the Procedure Code Filter. The rule will only fire for a claim that has at least two charges, and conditions are met for both filters.
- To use the Additional Procedure Code Group Filter filter, you must also use the Procedure Code Group Filter. The rule will only fire for a claim that has at least two charges, and conditions are met for both filters.
Example — Procedure Code filters
|
Your billing manager wants to Hold claims that have both procedure code 99213 and procedure code 90460 because in this situation, a modifier 25 should be added to the office visit (99213) charge.
|
|
|
Your Custom Rule: Procedures that Require Modifiers might look like this:
|
|
|
The rule will fire on any claims that have:
|
Example — Procedure Code Group filters
|
Your billing manager wants to Hold claims that have both an immunization procedure code and an office visit procedure code because in this situation, a modifier may be required.
|
|
|
Your Custom Rule: Procedures that Require Modifiers might look like this:
|
|
|
The rule will fire on any claims that have:
|
Claim rules are stored in the athenaOne Rules Engine. When you submit a claim in athenaOne, the claim must pass all claim rules before athenaOne assigns it DROP status. This is called "scrubbing" the claim. athenaOne automatically scrubs every claim you create, re-scrubs it every time you view or edit a claim, and re-scrubs it a final time when the claim is actually generated and sent to the payer.
Why so many scrubs? Because our Rules Engine database of claim rules is updated daily. A new claim rule may alter the status of a claim between the time that a claim is created, edited, and generated for submission.
When a claim rule detects a problem, it "fires." This means that the claim rule places an explanatory claim note in the Claim Notes section of the Claim Edit, Claim Review, Claim Action, and View Claim History pages, and assigns a claim status other than DROP. A claim note is a text explanation of the problem, often including instructions and links for correcting the claim.
There are many reasons why a claim note may appear in the Claim Notes Section, but a claim note that appears as the result of a claim rule is always shown with AUTO in the User column and SCRUB in the Action column.
The following types of claim notes are the result of claim rules.
Note: To override a review claim note, you must have the Claim Note Override: Review role or permission. To override an advice claim note, you must have the Claim Note Override: Advice role or permission.
- Rule — Claim rules that appear with bold red Rule at the beginning of the claim note text require that the claim error be corrected before the claim is assigned DROP status and submitted to the payer.
- Review — The Review type of claim rule is designed for use by billing managers and provides an override link. The billing manager reads the review claim note, decides whether any action is needed, and then updates the claim (or not) as appropriate. Review rules are based on local claim rules created for your practice, which allow us to hold certain claims for review by your billing manager. These rules typically hold claims for issues such as medical coding or other workflow-related reasons. The Claim Note Override: Review permission controls access to the override function.
Custom claim rules that you create for your practice are also designated as Review notes and include an override link. If overlapping custom rules of the same type are holding the claim (for example, multiple custom rules created on the Custom Rule: Invalid Modifiers page), you can override all the rules of that type by clicking the override all custom rules from same category link in the claim note. - Advice — The Advice type of claim rule (or "claim advice") also provides an override link that allows you to override the advice without editing the claim. The text describes potential problems with the claim and still allows for outcomes contingent upon knowledge that we do not have when the rules engine scrubs the claim. The advice allows athenahealth to apply our billing knowledge on a much broader scale.
What happens when you act on the advice and edit the claim? If you act on the advice claim note and the rule is cleared as the result of correction to the claim, the advice claim note appears gray. The claim is then assigned to the next appropriate status. (If there are no additional claim rule violations, the next appropriate status is DROP.)
What happens when you use the override? If you read the text of the advice claim note and determine that the advice action is not needed, you can click the override link. athenaOne then bypasses the advice, re-scrubs the claim, and assigns the next appropriate status. (If there are no additional claim rule violations, the next appropriate status is DROP.) The override event is logged in the claim note history (overridden by username, date). The Claim Note Override: Advice permission controls access to the override function. The "advice" type of claim rule is not available for practices that use athenaCollector (No Posting) and athenaCollector (No Follow-Up).
Note: An override link may also appear when a "predictive rule" fires. A predictive rule is a type of claim advice that uses historical data in athenaOne to predict likely denials, so that you can adjust them off to zero before they appear in your denial work queues. Predictive rules cover Medical Necessity Denials and Benefits Coverage (charges expected to be denied for a benefit limitation or exclusion).
Important: athenahealth has begun a backend upgrade to the Billing Rules system, which will enhance claims processing and transparency over time without disrupting your athenaOne experience.
- We expect implementation to continue through 2025.
- For details, see New Billing Rules System Launch (Success Community article)
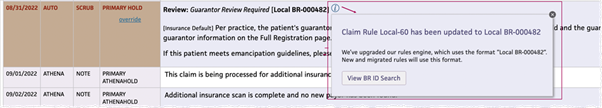
If a rule has been migrated to the new Billing Rules system (or is a new rule added only in the new Billing Rules system), you'll see a Business Requirement ID (BR-######) instead of a legacy Rule ID.
- Local rules will display as [Local BR-######].
- Click the information icon to see details about the BR ID:
- If this was a migrated legacy rule, you'll see the legacy Rule ID and the new BR ID.
- If the rule was created only in the new Billing Rules system, the information icon message will not have any legacy Rule ID.
- Click View BR ID Search to see the mapping of legacy Rule IDs to BR IDs for migrated rules in your practice.
- On the Main Menu, click Claims > (RESOURCES) BR ID Search.
- In athenaOne claim-related pages, such as Claim Action and Claim Edit, click the info icon next to a BR ID. In the pop-up window, click the View BR ID Search button.
The BR ID Search and BR ID Report appear in the left Task Bar.
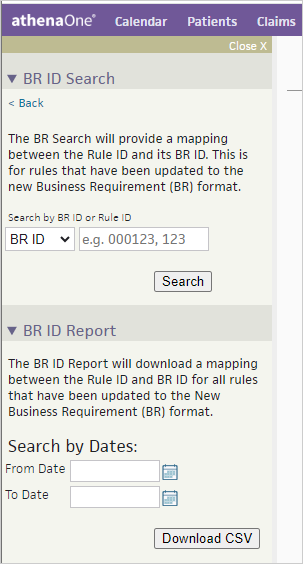
To use the BR ID Search or the BR ID Report, you must have the View Only Claims role.
Use this to see the mapping for a specific Rule ID or BR ID. This is for rules that have been updated to the new Business Requirement (BR) format.
- Search by BR ID or Rule ID — Select BR ID or Rule ID, then enter the Business Requirement ID or Rule ID you want to find.
- Click Search.
- If the Rule has been migrated, the following details appear:
- Business Requirement ID
- Rule ID — Rule ID from the legacy rules engine
- Type — Type of Rule: Global or Local
- Name — Name of the Rule
This report shows the mapping of legacy Rule ID to BR ID for all rules in a practice that have been updated to the new Business Requirement (BR) format.
Note:
- For global rules: Only migrated global rules that left a claim note will be listed in this report.
- For local and network rules: All migrated local and network rules will be included in the report (whether or not the rules left a claim note).
- In the left Task Bar, click BR ID Report to expand the section.
- Search by Dates — Select the date range for legacy rules updated to BR IDs on your system.
- Click Download CSV.
- The CSV filename appears in the top right of the page, with the From Date and To Date included in the filename: BRIDReport_MM_DD_YYYY-MM_DD_YYYY.csv
- The file is saved in the Downloads folder on your computer.
- Open the file with an application such as Microsoft Excel.
The report includes the following columns:
BR ID Report Column Description Context ID The athenahealth Context ID for your practice (and any other practices in your organization's network, if applicable) Rule ID The Billing Rule ID before the rule was updated to the new BR ID format Legacy Rule ID A combination of context ID plus local rule ID
(i.e., 1234.5 legacy ID indicates rule number 5 for context 1234)
BR ID The new Business Requirement ID Rule Name The name of the athenaOne Billing rule. Rule Type The type of rule:
- GLOBAL
- NETWORK
- LOCAL
Created The date the rule was updated to a BR ID on your system