View Claim History
This page allows you to view all old claims for a patient.
The Claim Form page displays a simplified view of the submitted claim with the option to view the claim in ANSI format.
- Display the Claim Edit or View Claim History page.
- Click View claim forms.
A selection window opens.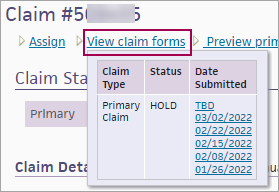
- In the Date Submitted column, click the version of the claim that you want to display.
The Claim Form window appears.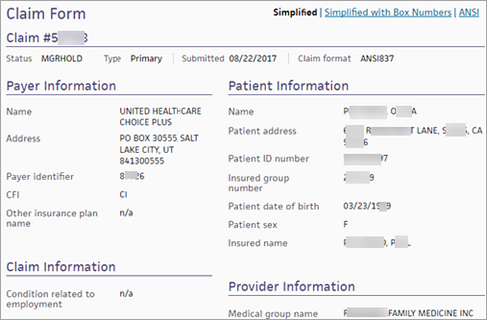
The Simplified view of the claim form is displayed.
Note: If the claim was dropped to paper (instead of being submitted electronically), the claim form is displayed in the CMS-1500 format. - To view box numbers on the claim form, click Simplified with Box Numbers at the top of the form.
- To view the claim in ANSI format, click ANSI at the top of the form.
Note: To see empty segments in the ANSI format, click Show empty segments at the bottom of the page.
A set of filter fields appears at the top of the page, showing the current filter selections. To change the filter criteria, click Edit filter. To save your selected filters for future use, select the Save as default option. These filters are selected by default the next time you open the View Claim History page.
Note: With Provider-Group-Based Data Permissions enabled, the Provider Group filter defaults to the current provider group if the patient has claims associated with it. Otherwise, the Provider Group filter defaults to All.
Each claim summary consists of a claim header that includes:
- Claim number
- Patient insurance package associated with this claim
- Patient name (last name, first name)
- Rendering provider's athenaOne username
- Supervising provider's athenaOne username
- Diagnosis codes and descriptions
Claim details include service date, procedure, charge, and a Claim Notes section showing the claim status and kick/scrub reasons.
Below the claim number are the following links:
- Claim Action page — Display the Claim Action page. This page allows you to review claims in HOLD status and resolve them on the same page. From the Claim Action page, you can appeal denials; adjust and transfer balances; update diagnosis codes, procedure codes, and modifiers; and add kick reasons.
- Edit — Display the Claim Edit page.
- View claim forms — Display the Claim Form page. This page displays a simplified view of the submitted claim with the option to view the claim in ANSI format. You can view previous submissions of the claim (see "To display the claim form window").
- Preview primary form — View the claim in the appropriate primary claim format as it would look now.
- Preview secondary form — View the claim in the appropriate secondary claim format as it would look now.
- Post — Display the Post Payment page for this patient.
| Column Headings for Charge History | |
|---|---|
| Service date |
Service date for each charge. |
| Procedure |
Procedure code and description of the procedure. |
| Charge |
Charge for each procedure or service. |
| Column headings for Claim Notes | |
|---|---|
| Date |
The date the action occurred. |
| User |
The username of the person who took the action. AUTO indicates an automated system function. Usernames that belong to your practice appear in regular font, but athenahealth usernames are italicized. Perot users have the prefix "vhs" in front of their usernames. |
| Action |
The action taken on the claim. Highlighting indicates a system-generated action.
|
| Claim Status |
The status of the claim following this action. |
| Kick/Scrub/Note |
A brief note describing the action, generally including a kick reason. Notes that appear here also appear under the Claim Notes section of the Claim Review, , View Claims for Charge Entry Batch, and the View Claim History pages.
For older claim notes, click [expand text] to see the text as it appeared when the rule fired on the claim.
Claim rules:
The following types of claim notes are the result of claim rules. Note: To override a review claim note, you must have the Claim Note Override: Review role or permission. To override an advice claim note, you must have the Claim Note Override: Advice role or permission.
Note: An override link may also appear when a "predictive rule" fires. A predictive rule is a type of claim advice that uses historical data in athenaOne to predict likely denials, so that you can adjust them off to zero before they appear in your denial work queues. Predictive rules cover Medical Necessity Denials and Benefits Coverage (charges expected to be denied for a benefit limitation or exclusion).
Kick codes:
Each payer has its own denial codes. athenaOne associates different payer denial codes to the athenahealth standard set of kick codes, which determines the appropriate next steps.
Note: When you add a claim note that sets a claim alarm, athenaOne displays the date of the alarm beneath the text of the claim note. The date appears as long as the claim alarm remains active. Claim alarms are reset every time a claim note puts a claim in — or LEAVES a claim in — BILLED status. When claim acknowledgment applies an EMCRCVD or PAYORRCVD claim note, the original alarm is cleared and a new one is set.
Claim Status Inquiry transactions:
Note: CSI transactions are supported for athenaCollector clients only. For more information about CSI, please refer to Claim Status Inquiry. |