Pay for Performance Dashboard
athenaOne for Hospitals & Health Systems
The Pay for Performance (P4P) Dashboard is a tool in athenaClinicals that aggregates quality program enrollment and performance information.
Use to view a summary of enrolled quality programs
The P4P Dashboard may be used to view a summary of enrolled quality programs, enrolled providers, and count of measures. To view a list of enrolled measures, links are embedded that automatically load a report in the Quality Management report (QMR). Enrollment changes made on the Program Enrollment page may take a couple of hours to appear. Enrollment changes using other methods may take up to 48 hours.
Use to view measure performance
The P4P Dashboard can be used by providers, practice managers, and practice staff to monitor performance in enrolled Quality Programs by serving as a launching point for a performance report in the Quality Management report (QMR). These reports are generated by the athenaOne Quality Management Engine (QME) which is a rules engine that evaluates the most recent patient data on a nightly basis to determine if a quality measure has been met (satisfied) or not met (unsatisfied).
Use to manage the Medicare Hospital Promoting Interoperability program attestations
Customers with athenaOne for Hospital and Health Systems can use the P4P Dashboard to complete Medicare Hospital Promoting Interoperability (PI) program attestations such as the Security Risk Analysis objective and the SAFER guides objective.
On the Main Menu, click Quality > Then click Pay for Performance Dashboard
To access this page, your practice must have at least one provider enrolled in a quality management program or have clinical guidelines turned on (see the Clinical Guidelines page) and you must have the Clinicals Admin role.
Quality managers can use the self-serve Program Enrollment page to adjust measure enrollments for their providers without having to go through the support case process. Before you use the Program Enrollment page, you must configure a provider:
- Make sure that the provider has been added to athenaOne on the Users page. (On the Main Menu, click Settings
 >User. In the left menu,under Practice Links — Users, click Users.)
>User. In the left menu,under Practice Links — Users, click Users.) - Add the provider to the Providers page. (On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Providers, click Providers.)
>Billing. In the left menu, under Practice Links — Providers, click Providers.) - On the Providers page, verify that this provider can create encounters; that is, the Encounters option on this page must be selected.
- Add the provider's NPI to athenaOne. (On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Enrollment and Numbers, click NPIs and Other Numbers.)
>Billing. In the left menu, under Practice Links — Enrollment and Numbers, click NPIs and Other Numbers.)
For more information on how to enroll a provider in a pay for performance program, see Program Enrollment.
The P4P dashboard can be used to monitor performance in Quality Management Programs by:
-
Providers — A provider may only be interested in viewing measures that they are directly responsible for completing.
-
Practice managers or staff — A practice manager or front desk staff member may wish to use the dashboard to monitor performance on measures for all providers across multiple programs or only to check on the performance of only one provider in a program.
Views
For most programs, the P4P Dashboard will display the number of participants in a program, the number of measures within that program based on enrollments, and can be used as an accelerator to the Quality Management Report (QMR). The dashboard will show all active programs for which at least one provider in the practice is enrolled.
Each program on the Pay for Performance Dashboard appears in a gray bar in the "accordion" at the top of the page, with this header information:
- Name of the program
- Reporting period/days until the end of the program reporting period (exception: Medical Home type programs do not have an end date)
- Number of registered providers or TINs in the program
The programs appear in alphabetical order. You can click any program bar in the accordion header to view program progress. When a provider views the program detail, the provider's own data is highlighted in the table. If applicable, the reporting period and submission date appear in the center top of the detail.
Note: To display information about older completed programs, select the Show Archived option above the list of quality programs.
When you click and expand a program bar, you can see the provider names and clinical quality measure counts for each tax identification number (TIN) that the providers practice under (CMS requires that providers submit data based on your TINs).
Test patients are patient records created strictly for testing purposes and do not represent a real person's chart. To remain compliant with government regulations for quality programs, make sure that you report and submit data for real patients only.
Note: In accordance with CMS and other quality program sponsors, inactive patients are included in athenahealth certified eCQMs and in quality program submission data on the MIPS Dashboard, the Pay for Performance Dashboard, the eCQM Data page, the Quality Management Reporting page, and in UDS reports.
You can use the Test Patients Identification page to find test patients and mark dummy patients as test patients. Use this page to make sure that test patients are not included in quality reporting when you create test claims, encounters, problems, or diagnoses within the test patient chart.
Note: Patients marked as test patients on the Test Patients Identification page are not included in quality program submission data on the MIPS Dashboard, the Pay for Performance Dashboard, the eCQM Data page, the Quality Management Reporting page, or in UDS reports. (Quality measures appear on the Quality tab of the test patient's chart for testing purposes only.)
Note: You can report on self-pay patients excluded from pay for performance programs using the Report Builder. Select the "Patient Self-Pay Restricted Yes/No" column in a Patient Demographics report.
Use the P4P Dashboard to see your hospitals Promoting Interoperability aggregated performance at the TIN level. Attribution is provider agnostic for the PI program regardless of user actions. During the reporting time frame, any relevant action taken by any user is evaluated for respective measures in the PI program on the P4P Dashboard. This will show the aggregated overall hospital’s performance that will ultimately be used for attestation.
Hospital PI Dashboard sections
The Hospital PI Dashboard will open displaying the behavioral measures section. Under these measures will be additional sections with the following objectives: Security Risk Assessment, Clinical Quality Measures, Public Health Registries, SAFER Guides Measure Attestation, HIE bi-directional Measure Attestation and Organizational Information which includes CMS contact information.
Behavioral Measures
This section displays the hospital level PI data and performance for behavioral measures. Each PI measure will be listed with the corresponding CMS specifications, your hospital's current performance, the numerators and denominators affiliated with the measure and finally, a maximum points and points earned column. For measures or objectives that are performance based, the numerator must contain a value greater than zero to be able to snapshot for data submission, irrespective of your program score, unless an exclusion has been filed. For example, even if you score 60 points, if you haven't satisfied the objectives (i,e., your numerator = 0) you will fail the program and will be subject to a downward payment adjustment.
Objectives
The descriptions below walk you through the 'Objectives' section of the P4P Dashboard.
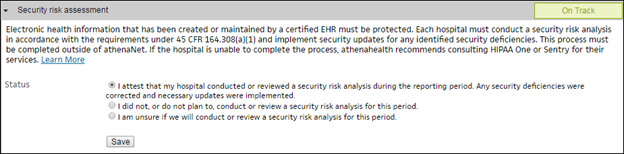
Security Risk Assessment
This section allows the MUPP to indicate completion of the Security Risk Assessment.
Report Clinical Quality Measures
athenahealth has partnered with a quality vendor, Persivia, to track and submit your electronic Clinical Quality Measure (eCQM) data. You can track your eCQM performance on the Persivia Dashboard. See the Persivia Dashboard User Manual for more details.
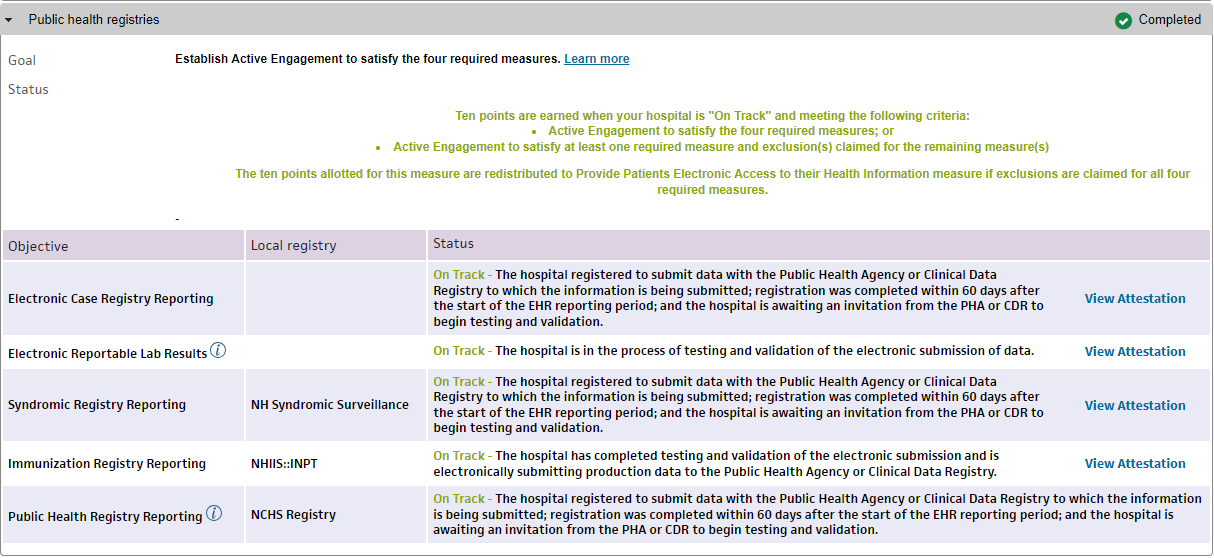
Public Health Registries
This section displays the current status of your hospital's public health reporting objective. This also shows the specific registries your hospital is engaged in, the current standing of engagement, and any tasks that must be completed.
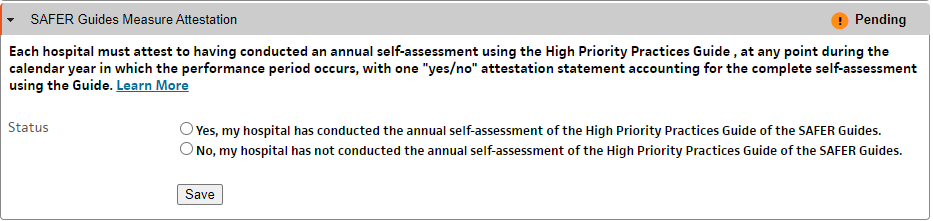
SAFER Guides Measure Attestation
This section allows the MUPP to indicate completion of the annual self-assessment using the High Priority Practices Guide.
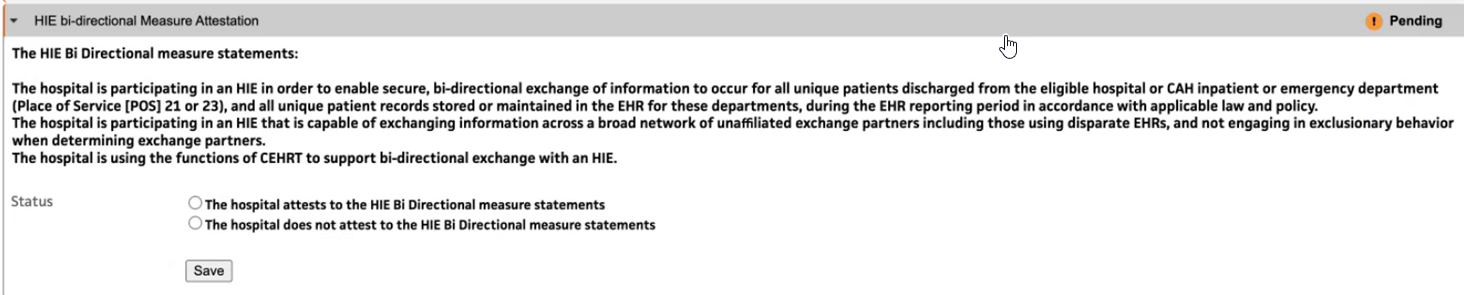
HIE bi-directional Exchange Attestation
You can attest the HIE Bi-directional measure if you are connected to a qualifying HIE. This measure is strictly an attestation-based measure for the PI Medicare program.
Note: The hospital or CAH is responsible for determining that they qualify to attest to this measure and provide CMS with any needed documents in-case of an audit.
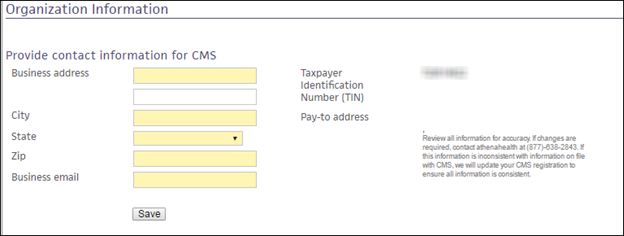
Organization Information
This section allows you to provide your hospitals contact information for CMS. This organizational information should match what is in the CMS portal.
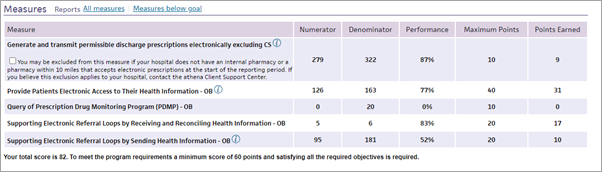
Measures — Column descriptions
-
Measure — The name of the measure along with exclusion criteria.
-
Numerator — The total number of qualifiers for that measure.
-
Denominator — The total population for that measure.
-
Performance — Your hospital's current performance for that measure.
-
Maximum Points — The number of points each objective is worth up to.
-
Points Earned — The calculation of the Numerator divided by the Denominator and then multiplied by the Maximum Points.
For more information, see the Hospital Promoting Interoperability resource page on the Success Community. You can also access this page at the top of the Hospital PI Dashboard in athenaOne.
The details for quality programs other than Promoting Interoperability include only the reporting period, list of providers participating in the program, and the number of measures for which each provider is enrolled. When you click a provider name or the number in the Measure progress column, the Quality Management Reporting page appears and displays program information for the selected provider.
Note: Generic Clinical Guidelines programs are not included in the display. These programs appear on the Quality Management Reporting page.
athenahealth supports the Together 2 Goal campaign developed by the American Medical Group Association on the Pay for Performance Dashboard. This program helps address care gaps in Type 2 diabetes.
If a provider in your practice is interested in participating, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center to request enrollment in this program. For more information about the Together 2 Goal campaign, visit the related American Medical Group Association website.