 User Guide — Claim Attachments
User Guide — Claim Attachments
When a claim requires additional documentation, athenaOne provides the tools you need to fax or upload the information, and attach it to the claim. To use these tools, the Claim Attachments feature must be enabled for your practice.
Note: Claim rule 2804 is activated when a claim requires an attachment. You can run the Claims Missing Required Attachments report to display a list of these claims. For information about resolving claims in HOLD because of claim rule 2804, see How to Resolve Global Rule 2804: Report Missing Attachments.
Use the Manage Attachments page to attach medical documentation to a claim (this documentation must pertain to the date of service and services provided on the claim).
Important: Do not use the Manage Attachments page to submit an EOB that has not yet been posted in athenaOne; use the Submit Remittance tab on the Manage Remittance page for this purpose.
To attach a document to a claim, your practice can use the following methods:
- Browse and Attach — With athenaClinicals, you can browse for and attach documents from a patient chart.
- Fax method — You can send the hardcopy document by fax, using our barcoded fax cover sheet, to 1-888-402-7297.
- Scan method — You can scan the hardcopy attachment, save the document locally as a .pdf file, then attach it to the claim using the Browse button.
- Interface method — You can use a file-drop interface. Very large, high-volume enterprises may wish to purchase an interface (contact your athenahealth Customer Success Manager for more information).
When a claim is returned by the payer with a request for a medical record or other attachment, follow the steps on the Manage Attachments page to create an attachment and fax or scan the required attachment.
If your practice uses athenaClinicals, athenaOne automatically attaches the visit note to the motor vehicle accident (MVA) or workers compensation accident claim. The encounter associated with the claim must be closed. In the Attachments section of the Claim Edit page, you see Claim Rule/Business Requirement BR-006224 (workers compensation) or Claim Rule/Business Requirement BR-006498 (auto accident).
Note: If a rule has been migrated to the new Billing Rules system (or is a new rule added only in the new Billing Rules system), you'll see a Business Requirement ID (BR-######) instead of a legacy Rule ID.
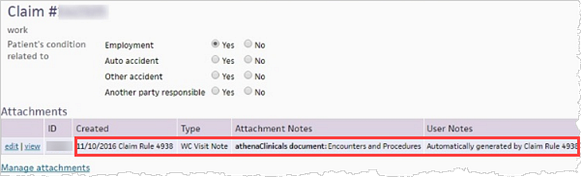
You can click Manage attachments to attach additional documents to the claim.
If you create the claim before the encounter is closed, athenaOne adds the attachments to the claim after you close the encounter.
After the Claim Attachments feature is enabled for your practice, the following pages become available.
An attachment type describes the kind of document required for an attachment. You can create and administer your own attachment types. Attachments must be in PDF format.
When a claim requires an attachment, you see an Add attachment link on the Claim Edit page, the Claim Action page, and the Claim Review page. You can fax, scan, or upload via interface the needed document and attach it to the claim. If the required document is not available, you can create a placeholder for the attachment and attach it later.
From this page, you can view and administer an individual attachment or replace a placeholder with the required document.
A "no attachment reason" describes why no attachment is needed for a claim that has an attachment placeholder. For such claims, you must select a no attachment reason to place the claim in DROP status. Your practice can administer your own "no attachment reasons."
For interface uploads, you can generate an error queue worklist of claim attachment upload errors so that you can monitor and resolve any claim attachment upload errors that may occur. (Your practice is responsible for monitoring and resolving any upload errors that appear in the queue.)
You are responsible for printing and submitting secondary or tertiary insurance claims that require documentation other than proof of prior payment. athenahealth will submit secondaries that require the primary's EOB, but you must submit secondaries that require operating notes, for example.