User Guide — athenaOne Medical Coding (for ambulatory customers)
User Guide — athenaOne Medical Coding (for ambulatory customers)
athenaCollector + athenaClinicals
athenaOne® Medical Coding is an optional add-on service for ambulatory practices using athenaOne® Base or athenaCollector®and athenaClinicals®. Ambulatory coding is often referred to as professional-fee coding, and is distinct from the hospital (inpatient) coding service.
With this service, athenahealth certified coders review patient encounters in athenaOne for ICD-10 CM diagnosis and CPT/HCPCS and assign appropriate codes and modifiers. athenaOne Medical Coding adheres to requirements and guidelines set by CMS and the AMA.
Medical Coding excludes any specialized or non-standard coding, such as coding related to MIPS, CPT II codes, customer-specific directives or requirements, or payer contracts.
In the athenaOne Success Community:
- Medical Coding Service Description — describes the Medical Coding service provided by athenahealth, including the division of responsibilities between you and athenahealth
-
FAQ: athenaOne Medical Coding Service — frequently asked questions and answers
-
Resource Overview: athenaOne Medical Coding — addtional resources to support customers using the athenaOne Medical Coding service, such as Training, Demo video, specialty-specific Best Practice guides
Your organization must sign a contract before using this feature. Please contact your Customer Success Manager to begin the process.
Practice settings — During your onboarding process, athenahealth will enable all Medical Coding settings and routing within your tablespace. These settings are required to enable the Medical Coding functionality and will give you access to an updated Workflow Dashboard, Medical Coding worklists, as well as the ability to route Visits to be coded.
For details, see athenaOne Medical Coding Settings (for ambulatory customers).
To access the athenaOne Medical Coding Performance Dashboard, you must have the Coding Services: Dashboard role added to your user profile.
For details, see the Medical Coding Service Description in the athenahealth Success Community.
athenahealth will provide the supported procedure, evaluation and management and diagnosis coding along with the appropriate modifiers (“medical coding”) for your Visits as described in the athenaOne Medical Coding ambulatory Service Description document.
- All medical coding is performed and/or reviewed by a team member holding an AAPC or AHIMA certification prior to claims being submitted to payers.
- Medical Coding excludes any specialized or non-standard coding, including coding related to MIPS, CPT II codes, customer-specific directives or requirements, or payer contracts.
- athenahealth does not handle any fee schedule updates, and any CPT/HCPCS codes must be added by the practice for coders to be able to select an applicable code.
As set forth in your athenahealth services agreement, we will complete medical coding upon your Go-Live Date for Visits that you route to us for coding.
- Prior to sending a Visit to us for coding, you must ensure that all information related to each Visit is accurately and completely documented in athenaOne, as described in our onboarding training and any documentation subsequently provided to you for Medical Coding. This includes but is not limited to, entering and verifying all visit details related to registration and the actual visit. We rely on you to verify the accuracy and completeness of all information documented in athenaOne, and we assume for Medical Coding purposes that all information has been verified as accurate and complete.
- Once you have included all the necessary information and documents, you can send a Visit to us for coding by clicking Send to Coding on the Charge Entry screen in athenaOne.
-
The athenaOne system will scan each missing slip for the following billing integrity condition:
Manual Routing — Billing Integrity Conditions Encounter Signed and closed
- If an encounter has not been reviewed and signed off by the provider, a message will notify you that the missing slip has failed the billing integrity check.
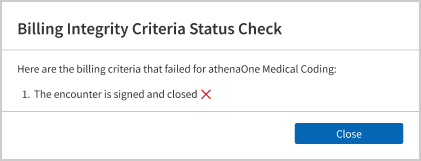
- The missing slip will then be linked under Unmet Criteria for Medical Coding on the Workflow Dashboard.
- Use the Worklist: athenaOne Medical Coding page to resolve missing slips issues that need practice attention.
- If an encounter has not been reviewed and signed off by the provider, a message will notify you that the missing slip has failed the billing integrity check.
- Missing slips that pass the Billing Integrity Check are routed to athenaOne Medical Coding to complete medical coding.
- Coders may ask you questions or request further information through a Query; all Queries must be closed out before coding can be completed.
For detailed steps, see To send a missing slip to athenaOne Medical Coding in the Step-by-step instructions section below.
For ambulatory customers who have contracted with athenahealth for athenaOne Medical Coding services, eligible missing slips can be automatically pulled in for review instead of practice users manually sending each visit from the Charge Entry page.
Automated routing of eligible missing slips to athenaOne Medical Coding is an opt-out feature for any department/provider that is contracted with Medical Coding.
-
As of November 2024, athenaOne Medical Coding best practice configurations are enabled by default for all new ambulatory Medical Coding customers at Go Live to help them avoid delays in claim creation and time to bill, and use the Medical Coding service most effectively.
- To opt out for your entire organization or for specific department(s), contact your Customer Success Manager (CSM) or your Onboarding project team. For details, see athenaOne Medical Coding Settings (for ambulatory customers).
-
Note: Automated routing is only compatible with standard appointment workflows. If your practice uses the Expedited Encounter or Appointment Workflow Bypass, your CSM or Onboarding team will change this setting to No and you will need to use manual routing.
The athenaOne Medical Coding product scans each missing slip to determine billing readiness, and provides visibility on missing slips that fail to meet one or more Billing Integrity Criteria.
Missing slips are scanned for the following Billing Integrity conditions:
| Condition | Criteria |
|---|---|
| Encounter | Signed and closed |
| Billing Tab |
Review completed
Note: You can require Billing Tab review to be completed before the encounter is closed, so more missing slips can be automatically routed to athenaOne Medical Coding. See athenaOne Medical Coding best practice configurations for details. |
| Primary insurance package | Valid primary insurance package attached to the missing slip |
| Supervising Provider |
Valid Supervising Provider attached to the missing slip
Note: Supervising Provider can be defaulted from the Provider Table, so more missing slips can be automatically routed to athenaOne Medical Coding. See athenaOne Medical Coding best practice configurations for details. |
|
Patient Check-out
|
Completed
Note: You can choose to allow missing slips without Patient Checkout completed to be automatically routed to athenaOne Medical Coding. See athenaOne Medical Coding best practice configurations for details. |
Once missing slips have met all the above conditions, a charge validation is also done to check for:
-
Charges entered but not yet defined in the practice's Fee Schedule
-
Charges entered without a Diagnosis code
Missing slips that meet all the above criteria will automatically be routed to athenaOne Medical Coding.
Missing slips that fail to meet the criteria will appear in the Unmet Criteria for Medical Coding column on the Workflow Dashboard and on the athenaOne Medical Coding — Unmet Criteria worklist, where they can be reviewed and updated by your practice.
- Once your practice completes the actions needed, those missing slips will automatically be sent to athenaOne Medical Coding during the next hourly execution of the auto routing engine.
Note: Missing slips that have been updated on the Charge Entry page by the practice users must be manually sent to athenaOne Medical Coding.
- For detailed steps, see To manually send encounters to athenaOne Medical Coding after changes saved in Charge Entry in the Step-by-step instructions section below.
athenahealth examines patient health records for completeness and necessary supporting documentation to enable us to complete coding. athenahealth accesses patient health records and completes coding based on what is present in the record.
Charts requiring additional documentation or clarification are returned to your organization via a coder query process. Medical coding will not be completed until the requested information or documentation is received. It is your responsibility to respond to any queries.
For detailed steps, see To resolve queries sent by athenaOne Medical Coding in the Step-by-step instructions section below.
athenahealth creates claims and sends them directly to payers for adjudication after coding is completed; however, holds may prevent the claim from being sent to the payer or patient.
If a claim coded by athenaOne Medical Coding has a documentation or coding-related hold, we will move that claim to a worklist to be reviewed by us.
- You will work with us to address the documentation or coding-related hold.
- You will promptly respond to any requests made through athenaOne for additional information or documents.
- We will not be alerted to and will not respond to any hold for a claim not coded by us.
athenahealth may determine that your organization must resolve a claim in a coding-related hold, in which case the Medical Coding service routes the visit back to you for resolution.
- You can view claims in hold status via the Claims tab by selecting the Workflow Dashboard. Claims appearing in Athena Hold and CBO Hold will be worked by the coding service.
- For details on claim hold status indicators, see the Claim Status O-help topic.
The athenaOne® Medical Coding Performance Dashboard provides transparency into key performance indicators (KPIs) related to the athenaOne Medical Coding service, including:
- Service utilization rate
- Turnaround times
- Amount of work done by athenahealth's coding team independently
- Amount of work where the coding team needed your practice's assistance
- Time to Bill
- Evaluation and Management (E&M) distribution
athenaOne Medical Coding is available during the normal hours of operation for the athenaOne system, usually available 24 hours per day, 365 days per year, except when maintenance is required. If we need to disable athenaOne Medical Coding for maintenance, athenahealth notifies all users of the service.
- On the Main Menu, click Support > Success Community > Contact Client Support Center.
- Select Additional Services, and then athenaOne Medical Coding.
athenahealth asks you to designate a primary point of contact for us during the onboarding process to ensure a successful coding service implementation.
After your organization signs the athenahealth services agreement for athenaOne Medical Coding, athenahealth performs these actions:
- Ensures contracting is in place and grants Coder users access to the tablespace.
-
Assigns appropriate roles and permissions, and enables all Medical Coding settings. Once enabled, the settings give you access to an updated workflow dashboard, Medical Coding worklists, as well as the ability to route Visits to be coded.
For details, see athenaOne Medical Coding Settings (for ambulatory customers). - Provides practice workflow information regarding Medical Coding, and provides training materials.
If your organization includes athenaOne Medical Coding in your initial implementation of the athenahealth suite of services, the service is added to the onboarding process for athenaOne Base or athenaCollector and athenaClinicals, as well as any other services you purchase.
If your organization did not include athenaOne Medical Coding in your initial implementation of the athenahealth suite of services, we provide onboarding to help you get started with Medical Coding.
- Display the Claim Workflow Dashboard: On the Main Menu, click Claims and then click Workflow Dashboard.
- In the Missing Slips column, click a linked total. The Missing Slips worklist appears in the Task Bar on the left.
- In the Task Bar, click a linked missing slip. The Claim: Charge Entry page appears in the Workspace.
- Make sure the following required Billing information is completed correctly:
- Date of Service
- Service Department/Place of service
- Insurance
- Rendering Provider
- Supervising Provider
- Scroll down to the Charges section. The athenahealth Medical Coding team will enter information in this section.
- Note to Coder — Enter any information you would like a medical coder to review before coding this encounter.
- Click Send to Coding.
-
The athenaOne system scans the missing slip for the following billing integrity condition:
Manual Routing — Billing Integrity Conditions Encounter Signed and closed
- If the encounter has not been reviewed and signed off by the provider, a message will notify you that the missing slip has failed the billing integrity check.
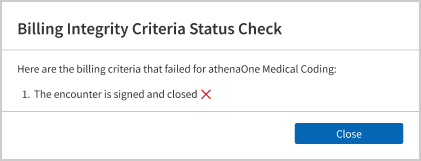
- The missing slip will then be linked under Unmet Criteria for Medical Coding on the Workflow Dashboard.
- Use the Worklist: athenaOne Medical Coding page to resolve missing slips issues that need practice attention.
- If the encounter has not been reviewed and signed off by the provider, a message will notify you that the missing slip has failed the billing integrity check.
- Missing slips that pass the Billing Integrity Check are routed to athenaOne Medical Coding to complete medical coding.
- A banner appears at the top of the Claim: Charge Entry page, confirming the encounter was successfully sent to the athenaOne Medical Coding service.
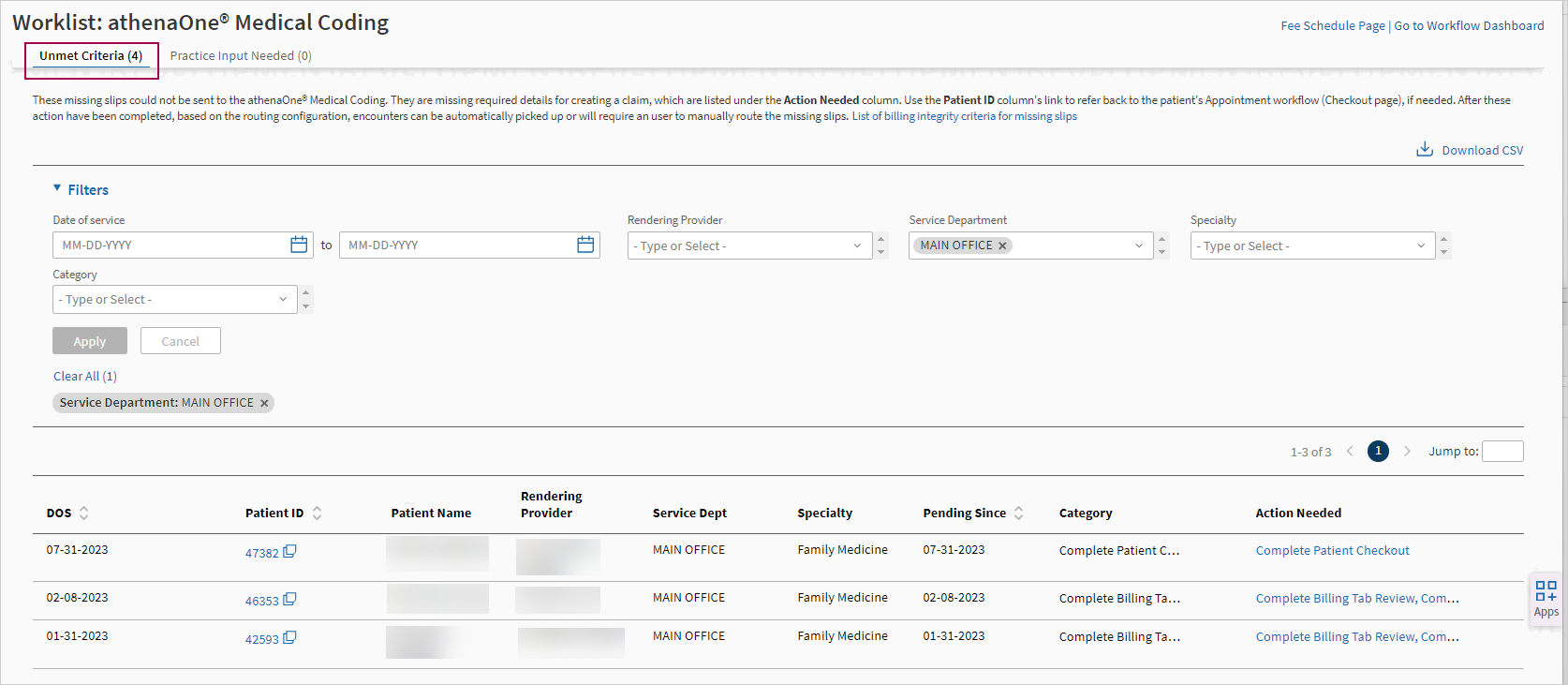
- Display the Worklist: athenaOne Medical Coding — Unmet Criteria page:
- From the Workflow Dashboard, click any linked number in the Unmet Criteria for Medical Coding column for a specific department.
- From the Non-Clinician Inbox, click the Unmet Criteria for Medical Coding link.
The Unmet Criteria tab of the Worklist: athenaOne Medical Coding page appears.
Tip: Click the image to see an expanded view
- Filter for the encounters you want to see and sort the columns if needed.
-
Hover over a linked action in the Action Needed column to see the complete list of actions needed for that encounter.
-
Click the linked action in the Action Needed column to display the page where you can complete the missing step or provide the missing information.
Action Needed athenaOne page/ Action Add Primary Insurance Claim: Charge Entry page — Update the Primary Insurance, then Save Changes.
Click Send to Coding.
Add Supervising Provider Claim: Charge Entry page — Select the Supervising Provider, then Save Changes.
Click Send to Coding.
Complete Billing Tab Review
Claim: Billing tab on the Checkout page — Verify billing information, then click Save & Enter Charges. Complete Patient Checkout Checkout page — Click Done with Checkout.
Ensure Provider has Signed and Closed the Encounter Follow up with the Provider for encounter sign off. Go to Charge Entry and Click Send to Coding Claim: Charge Entry page — Click Send to Coding. Manually Route Missing Slip Claim: Charge Entry page — Click Send to Coding. Review and Update Fee Schedule
Claim: Charge Entry page — Review the Charges section, then click Fee Schedule and update the required procedure codes.
Review and Update Procedures with Missing Diagnosis Codes Claim: Charge Entry page — Review the Charges section, update the required procedure codes, then Save Changes. Click Send to Coding.
-
Once you complete the actions needed, those missing slips will automatically be sent to athenaOne Medical Coding during the next hourly execution of the auto routing engine.
- Note: Missing slips that have been updated on the Charge Entry page by the practice users must be manually sent to athenaOne Medical Coding.
- Note: Missing slips that have been updated on the Charge Entry page by the practice users must be manually sent to athenaOne Medical Coding.
- On the page where you're completing the action needed, you'll see the Unmet Criteria task bar on the left. Click Return to Worklist: Unmet Criteria if you want to go back to the worklist.
- From the Worklist: athenaOne Medical Coding page, click Go to Workflow Dashboard in the top right if you want to return to the Workflow Dashboard.
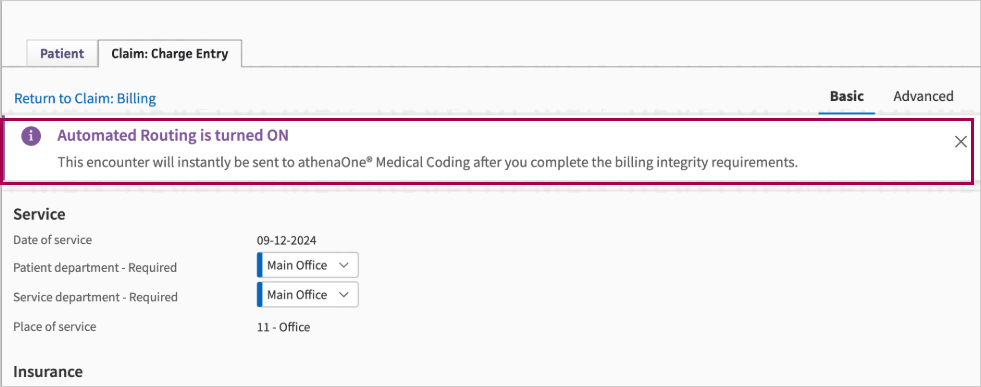
For ambulatory customers who have contracted with athenahealth for athenaOne Medical Coding services, if your organization has automated routing enabled:
-
The Send to Coding button on the Charge Entry page will be disabled by default because the system will handle routing automatically whenever possible.
An alert appears at the top of the page, letting you know the encounter will automatically be sent to athenaOne Medical Coding after you complete the billing integrity requirements.Tip: Click the image to see an expanded view
-
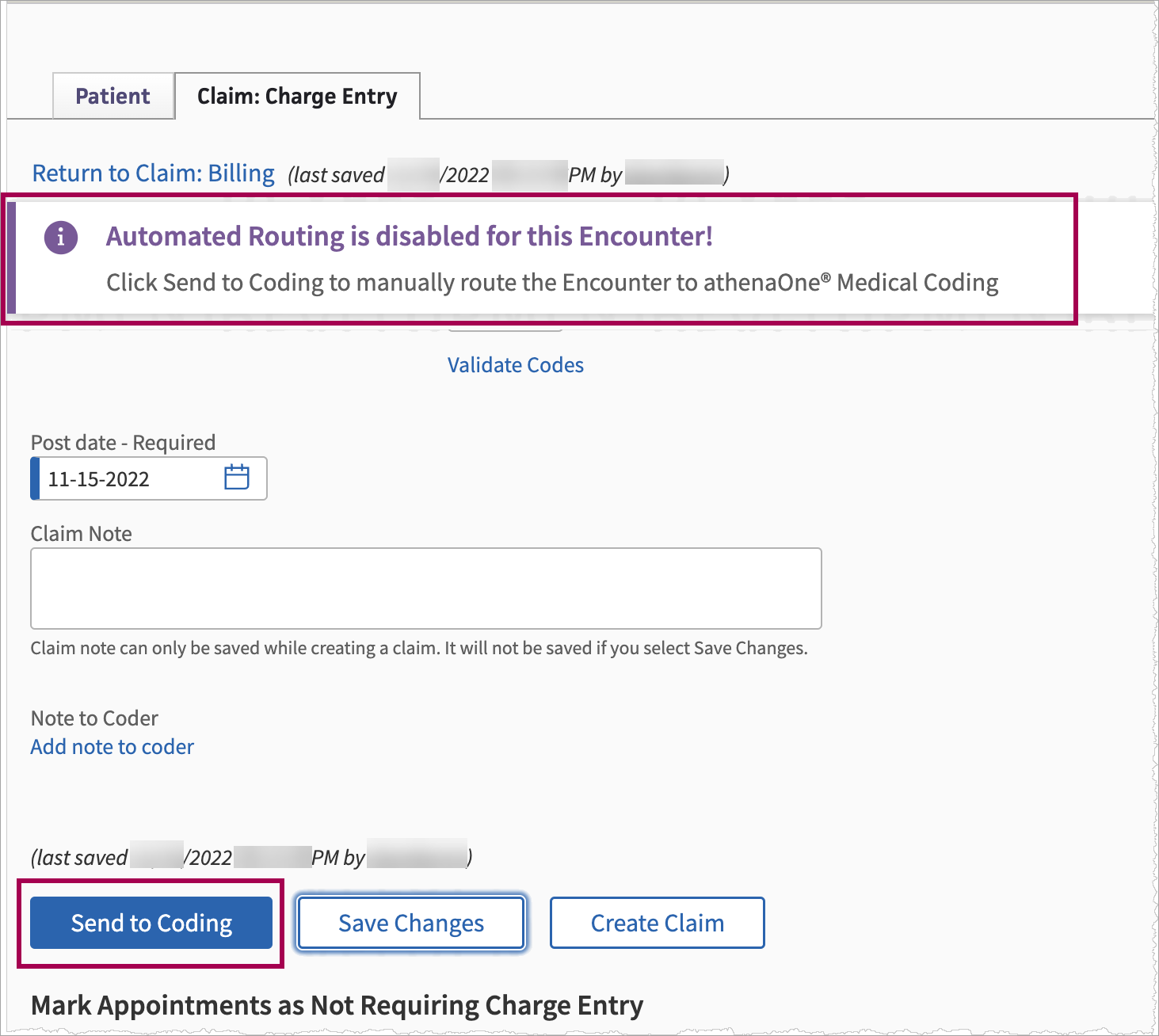
However, if you make changes on the Charge Entry page for an encounter and then click Save Changes, automated routing to athenaOne Medical Coding will be disabled and you will need to manually send that encounter to coding.
An alert appears at the top of the page:Tip: Click the image to see an expanded view
- Click Send to Coding .
-
The athenaOne system will check the billing integrity criteria and notify you if any criteria is not met.
-
Missing slips that fail to meet the criteria will appear in the Unmet Criteria for Medical Coding column on the Workflow Dashboard and on the athenaOne Medical Coding — Unmet Criteria worklist, where they can be reviewed and updated by your practice.
- In the worklist, you can filter on Action Needed: Manually Route Missing Slip to identify the missing slips that need to be manually sent to Coding.
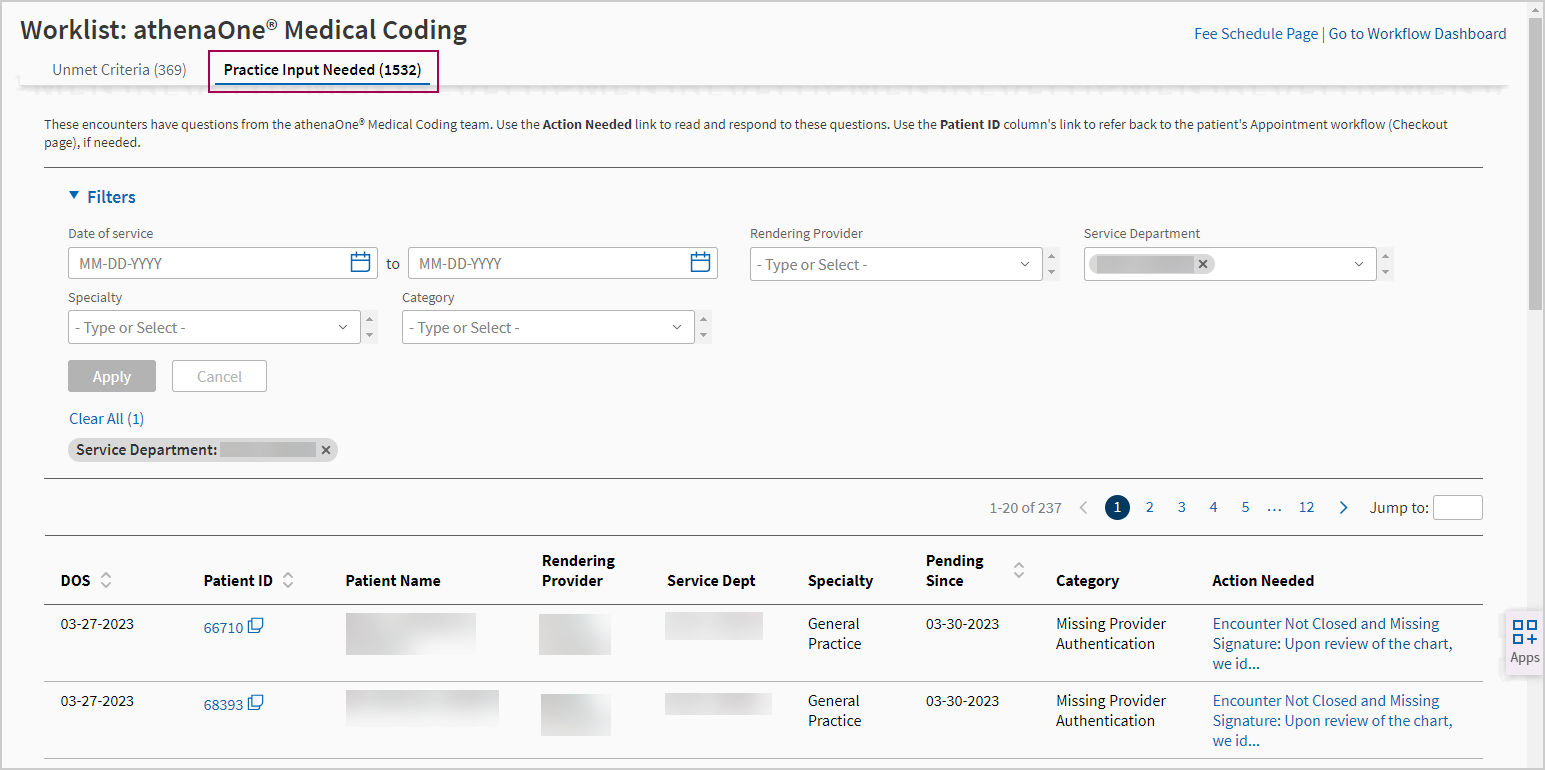
- Display the Worklist: athenaOne Medical Coding — Practice Input Needed page:
- From the Workflow Dashboard, click any linked number in the Practice Input Needed for Medical Coding column for a specific department.
- From the Non-Clinician Inbox, click the Practice Input Needed for Medical Coding link.
The Practice Input Needed tab of the Worklist: athenaOne Medical Coding page appears.
Tip: Click the image to see an expanded view
- Filter for the encounters you want to see and sort the columns if needed.
-
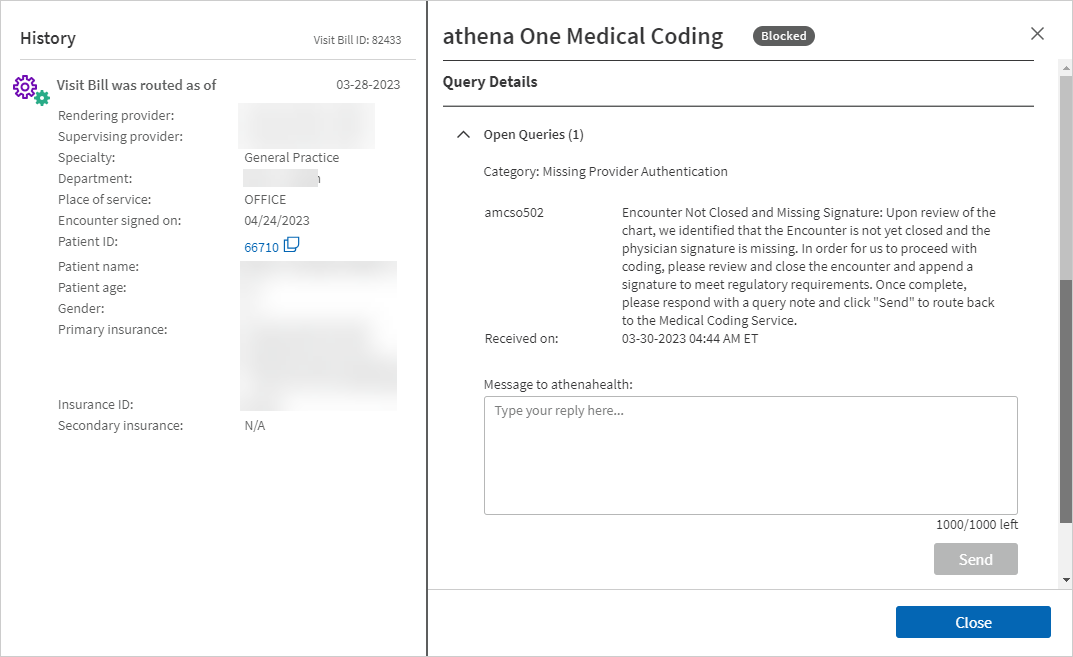
Click the linked text in the Action Needed column to view the Query Details window.
Tip: Click the image to see an expanded view
- Complete the actions needed to resolve the query.
- If the query is asking you to update documentation or provide more information, you can click the Patient ID link in this Query Details page to go to the appointment Checkout page.
- If the query is asking you to update your practice's Fee Schedule, you can click the Fee Schedule Page link at the top right of the worklist page to go directly to that page. Fee Schedule updates are one of the leading reasons why queries are raised today.
-
Respond to the coder by typing a reply in the text box in the Open Queries section, then click Send .
-
The encounter is automatically reassigned to athenaOne Medical Coding team.
-
Once you’ve responded to a query, it will move from Open Queries to Resolved Queries in the Queries Detail window.
-
You can always go back and review previous Queries, or click Add more details to add more information if needed.
-
Note: A reply is required before athenaOne Medical Coding can continue working on the visit bill.
-
-
Click Close to close the Query Details window and return to the Worklist: athenaOne Medical Coding — Practice Input Needed page.
- From the Worklist: athenaOne Medical Coding page, click Go to Workflow Dashboard in the top right if you want to return to the Workflow Dashboard.
- On the Main Menu, click Support > Success Community > Contact Client Support Center.
- Select Additional Services, and then athenaOne Medical Coding.
(Refer to the FAQs listed in the Resources section above)
Please review the below criteria/eligibility information to understand when automated routing to athenaOne Medical Coding would provide the most value and whether it's a good fit for your practice.
| Your practice should use automated routing if... | Your practice should not use automated routing if... |
|---|---|
|
|
No, automated routing can be enabled at a department level.
Only departments that are configured to send work to athenaOne Medical Coding can be enabled for automated routing to Medical Coding.
Automated routing only considers "new" appointments — this means appointments created on or after the Medical Coding go live date (not the automated routing go live date).
If your organization has the new automated routing functionality enabled, the Send to Coding button on the Charge Entry page will be disabled by default because the system will handle routing automatically whenever possible.
However, if you make changes on the Charge Entry page for an encounter and then click Save Changes, automated routing to athenaOne Medical Coding will be disabled and you will need to manually send that encounter to coding.
Missing slips are not automatically routed until they meet the Billing Integrity Criteria, which includes
- Encounter — signed and closed
- Billing Tab — review completed
- Patient Check-out — completed
So, you can still make updates to the missing slips if the encounter has not been signed, or the Billing Tab review has not been completed, or the patient has not been checked out yet.
- As Billing Staff, if you want to update any specific information in the missing slip, such as adding a practice note or including some charges, you will still be able to do that if the Patient is not checked out or the Billing Tab review is not completed yet.
- As a Provider, if you are used to having the Billing Staff review the chart before sending it to medical coding, you can still have them complete the review before signing off on the encounter.
For missing slips where the Supervising Provider is not already selected at the time of patient Check-in, the athenaOne system can auto-fill the Supervising Provider based on your practice configuration.
-
By default, we will use the Supervising Provider that is mapped to the Rendering Provider in the Provider configuration in your Billing Settings.
- If your practice is configured differently, or you would prefer to manually choose the right Supervising Provider for each missing slip, you can opt out of this auto-fill capability.
The automated routing engine does not pull in missing slips if even one of these conditions are unmet: patient is not checked out, or Billing tab is not reviewed, or encounter is not signed off. Having one of these conditions as unmet would allow you time to work on those missing slips and then have our automated routing engine pull them in once they are ready.