 User Guide — athenaOne Medical Coding (for hospital customers)
User Guide — athenaOne Medical Coding (for hospital customers)
athenaOne for Hospitals & Health Systems
athenaOne® Medical Coding is an optional add-on service for athenaOne for Hospitals & Health Systems.
Note: We also offer this service for ambulatory customers. If your practice does not handle inpatient coding, please see the User Guide — athenaOne Medical Coding (for ambulatory customers).
With this service, athenahealth certified coders review the patient health records for ICD-10 diagnosis, DRG, and CPT/HCPCS procedural documentation in athenaOne and assign appropriate codes. athenaOne Medical Coding adheres to CMS/AMA guidelines and coding conventions.
Your organization must sign a contract before using this feature. Please contact your Customer Success Manager to begin the process.
See also: User Roles and Permissions.
athenaOne® Medical Coding is an optional add-on service for athenaOne for Hospitals & Health Systems.
Note: We also offer this service for ambulatory customers. If your practice does not handle inpatient coding please see the User Guide — athenaOne Medical Coding (for ambulatory customers).
- athenahealth certified coders review the patient health records for ICD-10 diagnosis, DRG, and CPT/HCPCS procedural documentation in athenaOne and assign appropriate codes.
- Only evaluation & management CPT/HCPCS codes are extracted, as ICD-10 PCS procedures are not included in the service. Any evaluation & management (E/M) coding must be selected at the time of contracting and onboarding and cannot be added later.
- athenaOne Medical Coding adheres to CMS/AMA guidelines and coding conventions.
Routing is configured in the athena Medical Coding Settings page in athenaOne. For details, see To configure On Demand Medical Coding Service settings in the Step-by-step instructions section below.
As set forth in your athenahealth services agreement, athenahealth will complete medical coding upon your go-live date. When setting up the contract, your organization decides which version of athenaOne Medical Coding to use, which determines how charts route to the service:
- Exclusive — Select Exclusive to send all charts for a particular level of care to athenaOne Medical Coding. When you select the Exclusive Option for a particular Level of Care, athenahealth will activate that toggle on your behalf and will complete medical coding for all visits in that Level of Care.
- Note: These settings cannot be activated and deactivated at will; please see the on-demand setting for that option.
- On-Demand — Select On-Demand to control which charts you send to athenaOne Medical Coding and when you send them. After your organization signs the contract, you can configure the service settings on the athena Medical Coding Settings page.
- Your organization can deactivate and reactivate athenaOne Medical Coding at will, by activating or deactivating the toggle within athenaOne for any level of care (unless you executed an agreement with athenahealth that states otherwise).
- The coding service will complete coding for visits in that level of care until you deactivate the toggle for that specific selection.
- Note: You must configure the coding settings every time you activate the service.
When a visit is routed to athenaOne Medical Coding, athenahealth certified coders review the patient health records for ICD-10 diagnosis, DRG, and CPT/HCPCS procedural documentation in athenaOne and assign appropriate codes.
athenahealth will complete coding for the following (if applicable for the level of care):
- ICD-10 CM Diagnosis Codes — These codes will be added on the Medical Codes tab.
- ICD-10 PCS Procedure Codes — These codes will be added on the Medical Codes tab (only when corresponding with E/M code).
- Evaluation and Management CPT Codes (E&M codes for facility, professional, or both) — These codes will be added on the Charges tab. These are the only codes that will be entered on the Charges tab.
- Customers must opt in for Evaluation and Management coding.
- Diagnosis Related Groups (DRGs) — These codes will be added to the Medical Codes tab.
- All other codes that are not listed above are out of scope for athenaOne Medical Coding. This includes, but is not limited to, all other CPTs (other than evaluation and management), HCPCS, etc.
- If athenahealth coders determine that additional information or documentation is needed, we will send a message through a query, and we will not complete medical coding until you address the request in the query and resolve the question, update documentation, etc.
- Other exclusions of the service include: any specialized or non-standard coding, including coding related to MIPS, customer-specific directives or requirements, or payer contracts. We will not perform Medical Coding for any services performed outside of the Hospital setting, such as ambulatory (e.g., professional office or clinic) or nursing facilities.
Prior to sending a visit to athenaOne Medical coding, ensure all information relevant to the visit is accurate and complete in athenaOne:
- Merge/combine visits when necessary
- Enter and review charges
- Enter billing codes and modifiers on the Charges tab
- Confirm all necessary documentation/orders are available
Once a visit has been sent to Medical Coding, customers are responsible for reviewing and resolving queries from the coders.
For details on sending or recalling a chart, see the following in the Step-by-step instructions section below:
A claim coded by athenaOne Medical Coding may go into a HOLD status for a coding-related reason. When this happens, athenaOne Medical Coding works the claim to resolve the hold. The athenaOne system scans claims coded by Medical Coding twice a day to flag claims in a coding-related hold.
athenahealth may determine that your organization must resolve a claim in a coding-related hold, in which case the Medical Coding service routes the visit back to HOLD status or MANAGER HOLD status for resolution.
After coding and any coding-related holds are completed, claims are sent directly to payers for adjudication.
athenahealth examines patient health records for completeness and necessary supporting documentation to enable us to complete coding. athenahealth completes coding based on what is present in the record and does not support customized directives to place codes in any order or by default.
Charts with insufficient, incomplete, or conflicting documentation will be routed back to your organization via a coder query process. It is your responsibility to respond to any queries. For detailed steps, see To resolve queries sent by athenaOne Medical Coding in the Step-by-step instructions section below.
You can access reports that use key industry revenue cycle metrics to highlight your facility's medical coding performance.
The Hospital Activity Summary provides a comprehensive view of claim management issues and provides links to Visit Billing Tasks (coding, chart review and charges), claim worklists, enrollment items, interface items and more.
For additional reports and resources, please reach out to your Customer Success Manager.
athenaOne Medical Coding is available during the normal hours of operation for the athenaOne system, usually available 24 hours per day, 365 days per year, except when maintenance is required. If we need to disable athenaOne Medical Coding for maintenance, athenahealth notifies all users of the service.
To configure the On-Demand Medical Coding settings, you must have the Vendor Coding Settings Admin permission.
- Display the athena Medical Coding Settings page: On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Vendor Coding, click athenaOne® Medical Coding Settings.
>Billing. In the left menu, under Practice Links — Vendor Coding, click athenaOne® Medical Coding Settings. - Chart Routing — Select one of these options:
- Route all charts to athena Medical Coding Service — Select this option to send all charts to athenaOne Medical Coding.
Note: Select the Include backlog option to send all charts currently in "Ready for Coding" status to Medical Coding. - Configure Routing and E/M Leveling — Select this option to control which levels of care you send to athenaOne Medical Coding.
- Route all charts to athena Medical Coding Service — Select this option to send all charts to athenaOne Medical Coding.
- For each level of care, select In-house if you want your organization to continue coding these charts, or select athena Medical Coding Service if you want athenaOne Medical Coding to code these charts.
- For either chart routing option, select the Include backlog option to send all charts currently in "Ready for Coding" status.
- Click Save.
Your organization can begin sending charts to the coding service immediately.
- Display the Hospital Activity Summary page: On the Main Menu, click Claims, and select Hospital Activity Summary.
- Under the Chart Review heading, in the Ready for Chart Review column, click a linked number for the desired Level of Care row.
The Chart Review worklist appears in the Task Bar on the left. - In the Task Bar, click the linked visit ID number.
The Chart Review item of the Visit - Billing page appears in the Workspace. - Review chart documents to make sure documentation is complete.
-
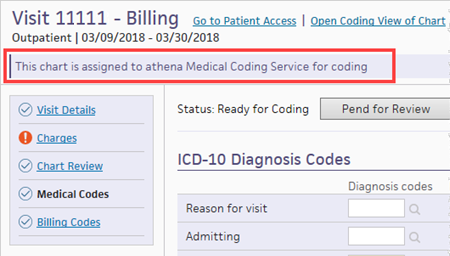
Click Send Chart to Coding. The athenaOne system sends the chart to athenaOne Medical Coding, and a banner appears on the Visit - Billing page that indicates the chart is assigned to Medical Coding.
Note: If a user at your organization completes coding for a chart that the athenaOne system sent to athenaOne Medical Coding, athenahealth still bills you for that chart.
- Display the Hospital Activity Summary page: On the Main Menu, click Claims, and select Hospital Activity Summary.
-
Under the Chart Review heading, in the Ready for Chart Review column, click a linked number for the desired Level of Care row.
The Chart Review worklist appears in the Task Bar on the left. - In the Task Bar, click the linked visit ID number.
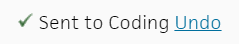
The Chart Review item of the Visit - Billing page appears in the Workspace. - At the top of the page (in the status area), next to Sent to Coding, click Undo.
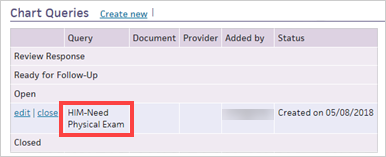
If insufficient documentation prevents athenaOne Medical Coding from completing coding, you see a chart comment, prefaced by "HIM- ," for your organization to review.
- Display the Chart Review page: On the Main Menu, click Claims, and then select Chart Review.
- Type — Select Chart Comment.
- Click Filter.
- Review the Medical Coding chart comments.
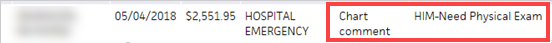
Tip: Click the Notes column heading to sort the comments in alphabetical order, making it easier to find comments from athenaOne Medical Coding. - Click the visit ID in the Visit ID column.
The Chart Review item of the Visit - Billing page appears. - Review the comment from athenaOne Medical Coding.
- Complete the steps required to resolve the query.
Important: You must preface all chart comments responding to Medical Coding with "CODER -." - Click close to close the chart comment and remove it from the visit.
- Click Send Chart to Coding.