 User Guide — Care Management Referrals from athenaClinicals to Population Health
User Guide — Care Management Referrals from athenaClinicals to Population Health
athenahealth Population Health + athenaClinicals
If your organization uses both athenahealth Population Health and athenaClinicals, providers can refer patients to a Population Health care management program by creating an order in athenaClinicals. The Population Health care manager can send summary reports of patient care to the referring provider in athenaOne. You can also bill Medicare for chronic care management services based on referrals from athenaClinicals to care management services in athenahealth Population Health.
Your organization must use athenahealth Population Health and athenaClinicals. In athenahealth Population Health, you must have a role that includes the following permissions:
- Population Management: Care Manager
- Population Management: Care Manager: Bulk Send Update to Provider — To send the care summaries for multiple patients to the referring provider
- Population Management: Care Manager: Send Care Summary — To send a care summary to the referring provider
To use the CCM integrated billing workflow, care managers must have these additional permissions:
- Population Management: Care Manager: CCM Billing — To send bill requests
- Population Management: Care Manager: CCM Billing Dashboard — To access the billing dashboard
- Population Management: Care Manager: Bulk Send Bill to Provider — To request and send billing to the referring provider for multiple patients
- Population Management: Person Center: Send Care Plan to Portal — To send care plan to the Patient Portal from the Person Center
Before you can use the integrated care management referrals feature, you must contact your Customer Success Manager (CSM) to assist you with setup.
Note: The data warehouse feed v1.1 is not required to use this feature, but athenahealth recommends that you implement it before you use this feature.
If your organization uses both athenahealth Population Health and athenaClinicals, providers can refer patients to a Population Health care management program by creating an order in athenaClinicals. The Population Health care manager can send summary reports of patient care to the referring provider in athenaOne.
- Providers can order care management referrals for any athenahealth Population Health program in the clinical encounter workflow and view feedback from the care manager about the patient.
- Care managers can add a care summary to the patient's medical record and notify the referring provider via the athenahealth Population Health Person Center.
If your organization uses both athenahealth Population Health and athenaClinicals, you can bill Medicare for chronic care management services based on referrals from athenaClinicals to care management services in athenahealth Population Health.
By sharing information between athenaClinicals and athenahealth Population Health, providers, care managers, and billing staff can coordinate and bill CMS for a patient's chronic care management.
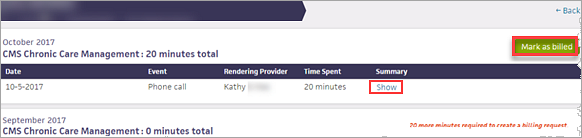
Each month, CMS allows you to bill for 20 minutes or more of CCM services rendered to patients enrolled in the CMS Chronic Care Management program. To track care management events eligible for CMS Chronic Care Management billing and attest to having sent the bill using athenaOne or third-party billing software, you can use the billing dashboard and summary.
- The billing summary in the patient's Person Center is a view of all completed care management events for the patient in each month. On this page, you can log when you submit a billing request for the patient.
- The billing dashboard (available on the Billing tab in the Care Manager), provides an aggregate view of all patients enrolled in the CMS Chronic Care Management program, as well as the total number of minutes of care management activities completed each month. On the billing dashboard, you can attest to sending billing requests for multiple patients at the same time.
Note: You can submit only one CCM bill or claim per patient per month.
Care managers document care management services by adding and completing events in the event timeline in a patient's Person Center. All event types in the menu on the Add Event page are considered CCM services. However, only events that have been closed and marked as complete count toward the 20 minutes of CCM services.
To be eligible for chronic care management services, patients must meet these requirements:
- Number of chronic conditions — Two or more
- Expected length of conditions — At least 12 months or until death
- Conditions pose significant risk — Death, acute exacerbation or decompensation, or functional decline
- Comprehensive care plan for conditions — Established, implemented, revised, or monitored
Providers who are eligible to be compensated for chronic care management services include:
- Physician (PCP or specialist)
- Physician assistant
- Nurse practitioner
- Clinical nurse specialist
- Certified nurse midwife
Note: Only one provider can submit one CCM bill or claim to CMS per month for each patient.
Care managers with the Population Management: Care Manager: Billing Dashboard permission can use the CCM billing dashboard to view the billing status of multiple patients at once (see "To view the CCM billing status of multiple patients"). On the billing dashboard, you can filter the list of patients by their CCM status.
- Not enough time spent — This status indicates that fewer than 20 minutes of CCM services have been rendered for the patient in the selected month.
- Ready to bill — This status indicates that at least 20 minutes of CCM services have been rendered for the patient in the selected month.
- Marked as billed — This status indicates that a care manager has already attested to sending the billing summary to the patient's provider for CCM services rendered to the patient in the selected month.
You can create orders in athenaClinicals for care management services provided using athenahealth Population Health.
![]() For a demonstration, see this video: How to Order General Care Management Referrals.
For a demonstration, see this video: How to Order General Care Management Referrals.
To find out whether a patient has been referred to a care management program, search for "care management referral" on the Find tab of the patient chart.
Note: To create an order for CCM care management services, see "To create an order for CCM services in athenaClinicals."
- In the Exam stage of an encounter, locate the Assessment & Plan section.
Note: You can also access the Assessment & Plan section from an order group or from the Orders and Results section of the Intake stage of an encounter. - Click the plus icon
 next to Diagnoses & Orders.
next to Diagnoses & Orders. - Search for and select care management referral.
- Select the diagnosis for this referral.
- Click the order to open it and expand the details.
- Send to — Select the care management receiver set up for your organization.
- Reason for referral — Enter the reason for the care management receiver.
- Care Program — Select the Population Health care management program for this patient.
- Sign the order.
The order is sent via interface to athenahealth Population Health.
![]() For a demonstration, see this video: How to Order a CMS Chronic Care Management Referral.
For a demonstration, see this video: How to Order a CMS Chronic Care Management Referral.
To find out whether a patient has been referred to a care management program, search for "care management referral" on the Find tab of the patient chart.
Note: To create an order for care management services not related to the CCM billing workflow, see "To create an order for care management in athenaClinicals (other than CCM referrals)."
- In the Exam stage of an encounter, locate the Assessment & Plan section.
Note: You can also access the Assessment & Plan section from an order group or from the Orders and Results section of the Intake stage of an encounter. - Click the plus icon
 next to Diagnoses & Orders.
next to Diagnoses & Orders. - Search for and select chronic care management referral.
- Select the diagnosis for this referral.
- Click the order to open it and expand the details.
- Send to — Select the care management receiver set up for your organization.
- Reason for referral — Enter the reason for the care management receiver.
- Care Program — Select CMS Chronic Care Management.
- Sign the order.
The order is sent via interface to athenahealth Population Health.
![]() For a demonstration, see these videos:
For a demonstration, see these videos:
- How to Enroll Care Programs from the Patients Dashboard
- How to Enroll Care Programs from the Person Center
When a clinician refers a patient to a care management program in athenaClinicals, the patient appears as Identified on the Patients tab in athenahealth Population Health. These patients do not have an assigned care manager.
- Display the Care Manager page: On the Main Menu, click Patients and select Care Management.
- Click the Patients tab.
- Display the list of identified, unassigned patients by setting these filters:
- Set the top filter (above the Program column) to All.
- Set the Assigned To column to None.
- In the Program column, click the name of the care management program.
Note: If you are enrolling the patient in CCM services, select CMS Chronic Care Management.
The Edit Program window opens. - Review the information in the Edit Program window and make any edits necessary.
- Status — Select Enrolled.
- Status note — Enter any notes about the status update.
- Click Save.
- Click the newly enrolled patient's name in the list to display the Person Center.
Care managers document care management services by adding events to the event timeline in a patient's Person Center. All event types in the list on the Add Event page are considered CCM services. However, only events that have been closed and marked as complete count toward the 20 minutes of CCM services.
- Display a patient's Person Center: On the Main Menu, enter the patient's name, patient ID, or member ID (insurance number) in the Search Bar. Under NETWORK PATIENTS, select the data type and then click the search icon. Matching patients are listed under the Patients tab. Click the patient name to expand the selection, and then click the patient name in large text to display the patient's Person Center.
- Click New Event at the top of the event timeline.
The Add Event window opens. - Event Type — Select the type of event.
- Reason(s) — Select one or more reason for the event.
- Roles — Check the roles the event applies to.
- Assign to — Assign the event to a member of the care team or to yourself.
- Date — Enter a date for the event.
- Time — Enter a time for the event to begin.
- Duration — Enter the duration of the event.
Tip: Click Show Schedule to open your schedule in the Person Center. Click Hide Schedule to close the schedule. - Attempt — If you try to contact the patient but are unsuccessful in reaching them, you can select a description of the attempt from the menu.
- Optional: Add a note in the free text field.
- Click Schedule or click Track Changes.
When you share or print a care plan from the Person Center, you can select the recipient and customize the content of the care plan.
- Display the patient's Person Center: On the Main Menu, enter the patient's name, patient ID, or member ID (insurance number) in the Search Bar. Under NETWORK PATIENTS, select the data type and then click the search icon.
Matching patients appear under the Patients tab. - Click the patient name to expand the selection, and then click the patient name in large text to display the patient's Person Center.
- From the SHARE WITH menu at the top right, select the person you intend to share the printed care plan with (Clinician, Patient, or Quality Manager).
Alternatively, you can click the print icon on most events to open the Share Care Plan window.
on most events to open the Share Care Plan window. 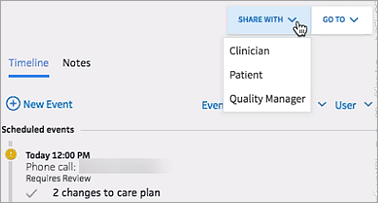
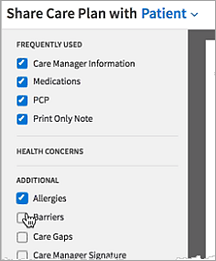
Note: The Share Care Plan with feature does not send the care plan to the selected person, but simply changes the type of information included in the printed document based on what that recipient would want to know. The default content of the printed care plan is configured for each type of recipient, but you can select or deselect information in the document preview window before printing. - Customize the printed care plan by selecting and deselecting options on the left to add or remove information. For example, you can select the Allergies option to include allergy information in the printed care plan.
- If the recipient of the printed care plan is the patient, click Record Provision to indicate when the care plan was sent to the patient, and then click Save.
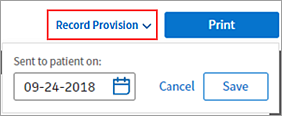
- Click Print.
The event appears on the patient's event timeline as "Care plan letter," and the Care Plan section of the Care Management tab lists the date, the sender, and the recipient of the care summary.
If your organization bills for Chronic Care Management services, follow these procedures to complete billing for CCM services and send the billing summary to athenaClinicals to generate a claim.
Care managers document care management services by adding and completing events in the event timeline of the patient's Person Center. All event types in the menu on the Add Event page are considered CCM services. However, only events that have been closed and marked as complete count toward the 20 minutes of CCM services.
- Display the patient's Person Center: On the Main Menu, enter the patient's name, patient ID, or member ID (insurance number) in the Search Bar. Under NETWORK PATIENTS, select the data type and then click the search icon.
Matching patients appear under the Patients tab. - Click the patient name to expand the selection, and then click the patient name in large text to display the patient's Person Center.
- In the event timeline, click the event that you want to bill to open the expanded event details.
- Time Spent — Enter the number of minutes of services rendered.
- Click Resume Later or Complete Event.
Note: You can only complete events that are assigned to you and that do not require review. Marking an event as Complete locks the event permanently and prevents further edits. You cannot undo or unlock completed events. If additional notes are needed after an event has been marked as complete, you can create another event and add a note there.
When the total number of minutes of CCM services rendered reaches 20 minutes in a month, the Billing Summary option appears in the GO TO top right corner of the patient's Person Center.
- Display the patient's Person Center: On the Main Menu, enter the patient's name, patient ID, or member ID (insurance number) in the Search Bar. Under NETWORK PATIENTS, select the data type and then click the search icon.
Matching patients appear under the Patients tab. - Click the patient name to expand the selection, and then click the patient name in large text to display the patient's Person Center.
- Click the GO TO menu, then select Billing Summary.
- Click Show to display the clinical summary note associated with the care event.
- Click Export to Excel under any billing summary title to create a .csv file of the billing summary.
- Click Mark as billed to the right of the month to bill.
The Billing Summary is highlighted and the rest of the page is grayed out.
Important: When you click the Mark as billed button, you are attesting that these care management activities have been billed for this month in a third-party billing system outside athenahealth Population Health. - Click Mark as billed again.
The bill is marked as sent by you on today's date.
A global rule places the claim in PRIMARY HOLD status. To view the claim:
- Display the View Claims Worklist page: On the Main Menu, click Claims > Claims Worklists. The View Claims Worklists appear in the Task Bar, with links to worklist categories.
- Under HOLD, click By Reason to view the category containing the claims for CCM services.
- Click a linked item (patient name, dollar amount, or billing slip number) for the claim.
The Claim Action page appears in the workspace. - Review the claim information and hold summaries.
- Click Override.
athenaOne submits the claim to CMS.