User Guide — athenaOne Support for Compliance with No Surprise Billing Legislation
User Guide — athenaOne Support for Compliance with No Surprise Billing Legislation
athenaOne for Hospitals & Health Systems
These features in the athenaOne system help support compliance with the No Surprise Billing legislation.
The No Surprises Act (effective January 1, 2022) protects patients from surprise medical bills for certain healthcare services where the provider or facility is out of their payer's network.
Resources from the Centers for Medicare and Medicaid Services:
Your practice must determine whether your providers and care facilities are subject to the No Surprises Act requirements. Use of these athenaOne features does not guarantee compliance, but will facilitate your organization’s efforts to meet relevant regulations.
The No Surprises Act was signed into law on December 27, 2020 as part of the Consolidated Appropriations Act of 2021. The legislation became effective on January 1, 2022 (for claims with a Date of Service of January 1, 2022 or later).
The No Surprises Act:
- Protects patients from surprise medical bills for emergency services and certain services performed by out-of-network providers at in-network facilities
- Requires that providers and facilities provide patients good faith estimates of charges for scheduled health care services for uninsured (or self-pay patients), and provide insured patients good faith estimates if consenting to applicable out-of-network provider services at in-network facilities
- Establishes an independent dispute resolution (IDR) process to resolve payment disputes between a provider or health care facility and a patient's health plan
Your practice must determine whether your providers and care facilities are subject to the No Surprises Act requirements. Use of these athenaOne features does not guarantee compliance, but will facilitate your organization’s efforts to meet relevant regulations.
Note: The following example is intended for illustrative purposes only and does not constitute legal advice.
Patient Jane Doe has a scheduled surgery next week at Seven Hills Medical Group.
The facility is in-network for Jane’s insurance but the surgeon, Dr. Mary Smith, is out-of-network.
If Seven Hills Medical Group wishes to balance bill Jane for the out-of-network costs associated with Dr. Smith’s services, Jane must receive notice and provide consent in accordance with the No Surprises Act requirements. This may include the following steps:
- (Within the applicable timeframe as defined by the regulations)
- Determine that Jane’s upcoming appointment includes an out-of-network provider performing non-ancillary services
- Enter Jane’s expected procedures and estimated cost of out-of-network non-ancillary services for the appointment
- Generate a patient consent form for the out-of-network non-ancillary services
- Send Jane the consent form notifying her of Dr. Smith’s out-of-network status and estimated cost
- Receive Jane's signed consent form
- Upload Jane’s signed consent form and attach it to her appointment
- Review Jane’s consented amount at charge entry
- Include the signed consent form from the appointment on Jane’s claim
These features in the athenaOne system make it easier for you to manage your practice's patient balance billing preferences and out-of-network patient consent requirements.
-
Use the Patient Billing Settings for Out-of-Network Providers page to track in athenaOne which providers are out-of-network with which payers, and specify the patient balance billing preferences for those providers.
- Flag upcoming appointments that allow for consent to balance bill (Out-of-Network Billing Consent).
- See the current Out-of-Network Billing Consent status for appointments.
- Manage Out-of-Network Billing Consent steps: Enter the expected procedure(s) and cost estimate, create consent form; send consent form to patient; attach a signed consent form to a patient's appointment.
-
See the patient's consented amount and signed consent form and option to carry the consented amount from the appointment to Charge Entry and the claim.
-
The athenaOne system uses the patient's consented amount, the payer payment amount, the adjudicated Patient Responsibility amount, and your Patient Billing Settings for Out-of-Network Providers, to determine the amount to bill the patient.
-
The athenaOne system sends claims to HOLD or bills the patient, based on your configuration settings and the patient consented amount.
-
Use claim worklists to resolve claims that are on HOLD for No Surprise Biling review.
Limitations:
- athenahealth is providing enhancements to help support compliance, but each practice will need to determine if the No Surprises Act obligations impact their organization, how to configure adjudication, and which new options they will use.
- Additional requirements, such as state laws on balance billing, may be applicable to your practice.
- We’ll continue to work closely with our customers to determine where additional enhancements in the athenaOne system can support compliance with any new requirements.
You can use the Self-Pay Cost Estimate tool to generate a cost estimate for self-pay patients when viewing an appointment that hasn't been checked in yet.
See To create a cost estimate for self-pay patient appointments for details
For practices with at least one department with athenaClinicals enabled:
- You can use a filter and display column in Report Builder to report on cost estimates shared with patients: Cost Estimate Shared with Patients Y/N
- These are available in Claim and Appointment report types
| Field Type | Field | Description |
|---|---|---|
| Filter | Cost Estimate Shared with Patients Y/N |
Include this filter in your report if you want to filter based on whether a cost estimate was shared with the patient.
Filter Criteria: (available when running a report)
|
| Display column | Cost Estimate Shared with Patients Y/N |
Include this column in your report if you want to display whether a cost estimate was shared with the patient.
Report output for this data element: (available when running a report)
|
You must be using the No Surprises Act Consent feature, and have your billing preferences entered in the Patient Billing Settings for Out-of-Network Providers page.
Before you can use the athenaOne features that support compliance with the No Surprises Act requirements, athenahealth must enable these settings for your practice:
(All three of these settings must be enabled to ensure a patient's consented amount and consent form from an appointment are included in a claim.)
- No Surprises Act Consent — Gives you access to the Patient Billing Settings for Out-of-Network Providers page to configure adjudication logic.
- This can be enabled for all departments (default) or for specific departments only
- Available service type add-ons: No Surprises Act Consent — Allows you to view and edit the patient consented amount at Charge Entry and Claim Edit.
- Default selected service type add-ons: No Surprises Act Consent — Allows you to always show this add-on at Charge Entry.
Please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center if you wish to enable these settings.
- If the No Surprises Act Consent practice setting is turned ON without specifying any departments:
- All departments will start using the new Patient Billing Settings for Out-of-Network Providers.
- Even departments that aren’t in the Emergency or Non-emergency configuration section will start using the new configuration.
- The athenaOne system will apply the Default Practice Settings, set to: Post as per the remittance and hold the claim for review.
- If the No Surprises Act Consentpractice setting is enabled, but the related Service Type Add-On is NOT enabled:
- The athenaOne system will start applying the new Patient Billing Settings for Out-of-Network Providers
- Claims will not have a patient consented amount (because you need the Service Type Add-On to enter it), so the athenaOne system will apply the Default practice settings to those claims.
| No Surprises Act Consent practice setting | No Surprises Act Consent service type add-on | Consented amount | Consent form | Claim adjudication |
|---|---|---|---|---|
| OFF | Not enabled | n/a | n/a | Claim uses existing Non-Par Providers settings |
|
ON,
Dept = default |
Enabled | Entered | Attached |
All of your departments will start using the new Patient Billing Settings for Out-of-Network Providers. Even departments that aren’t in the Emergency or Non-emergency configuration section will start using the new configuration; the Default Practice Settings are applied, set to: Post as per the remittance and hold the claim for review. |
|
ON,
Dept = specific depts selected |
Enabled | Blank | None |
Only the enabled departments will use the new Patient Billing Settings for Out-of-Network Providers; the athenaOne system will apply the Default practice settings to claims with no consented amount. |
|
ON,
Dept = specific depts selected |
Enabled | Entered | Attached |
Only the enabled depts will use the new Patient Billing Settings for Out-of-Network Providers; Adjudication logic will use the consented amount collected in the Service Type Add-On to set boundaries for patient billing, based on the Patient Billing Settings for Out-of-Network Providers. |
|
ON,
Dept = specific depts selected |
Not enabled | Blank | None |
Only the enabled departments will use the new Patient Billing Settings for Out-of-Network Providers; the athenaOne system will apply the default practice settings to claims with no consented amount. |
- To configure the Patient Billing Settings for Out-of-Network Providers, you need specific user permissions to access that page.
- To manage patient consent from the Eligibility and Phone list or the Appointment page, you need access to those pages.
- To edit patient consented amount at Charge Entry or Claim Edit, you need access to those pages.
- To review claims that are on HOLD for No Surprise Billing review, you need access to Claim Inbox or Claim Worklists.
You can flag upcoming appointments that may allow for consent to balance bill (Out-of-Network Billing Consent), and manage the patient consent requirements from either of these pages:
- Eligibility and Phone page
- Appointment page
From either page, clicking Manage consent brings you to a new Out-of-Network Billing Consent pop-up window to manage the consent steps.
Best practice: If you intend to balance bill for applicable services, the No Surprises Act requires that you notify patients about a qualifying out-of-network provider within specified timeframes before their appointment and receive appropriate consent.
- Display the Eligibility and Phone page: On the Main Menu, click Calendar. Under APPOINTMENTS, click Eligibility and Phone List.
-
View — select Out-of-Network Billing Consent to display the new Filter fields.
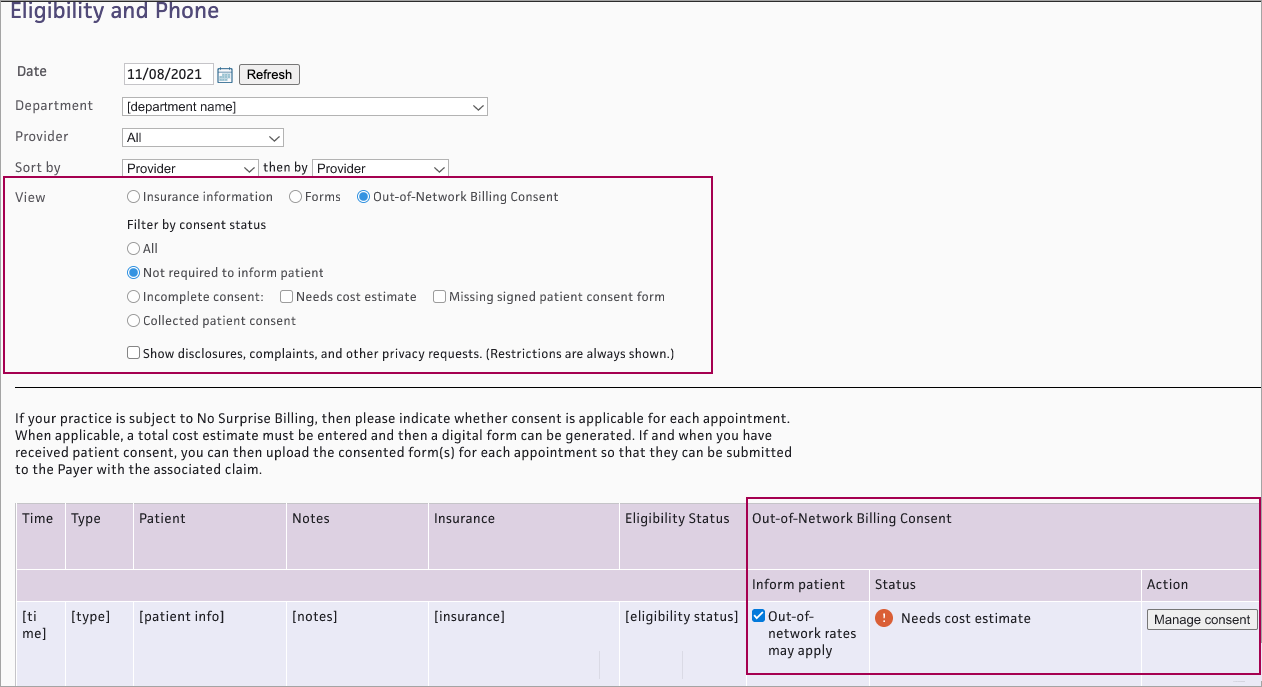
- Filter by consent status — Select a status:
- All — Shows appointments with any consent status
- Not required to inform patient — Shows appointments that have not been flagged as Out-of-network rates may apply, so patient consent is not available
- Incomplete consent — Shows appointments with incomplete consent. (If you select Incomplete consent, both Needs cost estimate and Missing signed patient consent form are automatically checked. You can also select either status independently.)
- Collected patient consent — Shows appointments with a signed patient consent form attached
- The list appears with the following new Out-of-Network Billing Consent columns for each appointment:
- Inform patient — Check the box Out-of-network rates may apply if applicable
- Status — Shows current Out-of-Network Billing Consent status for each appointment that has been flagged as Out-of-network rates may apply. See Out-of-Network Billing Consent Status for details.
- Action — Click Manage consent if needed to complete consent steps
- Display the Appointment page: On the Main Menu, click Calendar. Under APPOINTMENTS, click Today's Appointments.
- At the top of the Task Bar, select a specific Dept and Date, then click Go. The list of patients scheduled for that day appears below. Click a patient name in the schedule.
- Review the appointment information. If the appointment has an out-of-network provider: at the bottom of the Appointment Information section, select Out-of-Network rates may apply.
- The consent status and Manage consent button appear.
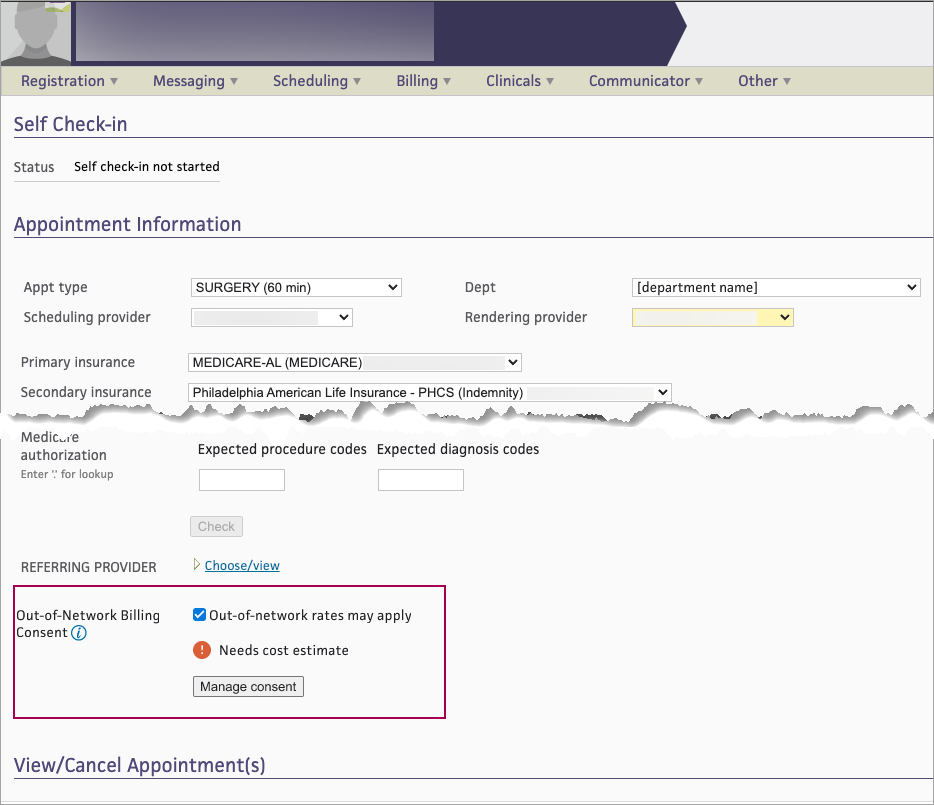
On either the Eligibility and Phone worklist or the Appointment page, you can see the current Out-of-Network Billing Consent status for each appointment that has been flagged as Out-of-network rates may apply. The status will change as the appointment moves through the steps in the patient consent process.
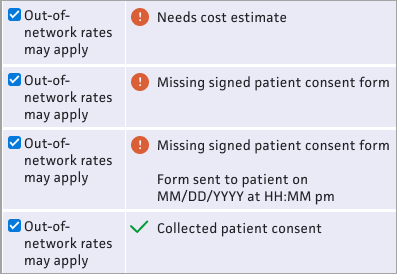
- Needs cost estimate — This status appears if the appointment has no cost estimate
- Missing signed patient consent form — This status appears if the appointment has a cost estimate but no signed consent form attached.
- Missing signed patient consent form / Form sent to patient on [MM/DD/YYYY at HH:MM pm] — This status appears if the appointment has a cost estimate, the consent form was sent to the patient, but no signed consent form is attached.
- Collected patient consent — This status appears if a signed consent form is attached to the appointment
On either the Eligibility and Phone worklist or the Appointment page, for each appointment that has been flagged as Out-of-network rates may apply, you can see the current Out-of-Network Billing Consent status and click Manage consent to complete the steps in the patient consent process.
- From either the Eligibility and Phone page or the Appointment page, click Manage consent.
-
The Out-of-Network Billing Consent window appears. The athenaOne system will use the information you enter here to populate the patient consent form.
Cost estimate
This estimate will include co-providers and/or co-facilities — When this box is checked, you are responsible for calculating and documenting the total cost estimate including costs for your practice and for each co-provider/co-facility.-
Enter the total cost estimate on the Total cost only tab.
- The consent form will include pages for you to write in the itemized services and subtotal for each provider and facility.
 Total cost only tab
Total cost only tab
Total cost only tab Field name Description Total cost estimate Enter the cost estimate Alternative in-network providers (Required for post-stabilization services) — Enter provider name(s) to be included on the HHS consent form 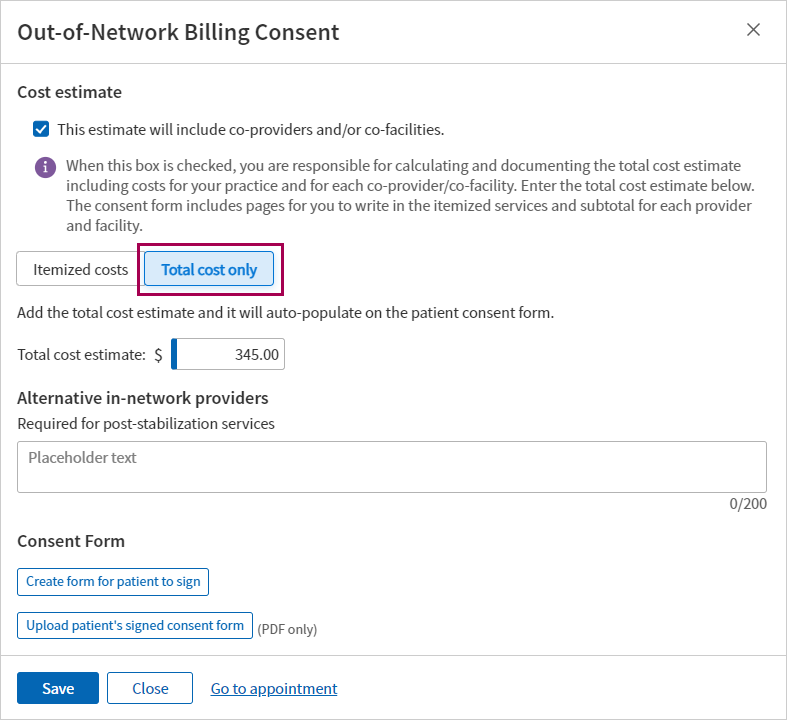
If the estimate will NOT include co-providers and/or co-facilities:
- Use the Itemized costs tab to enter up to ten specific procedure codes and estimated costs to populate the HHS consent form.
 Itemized costs tab
Itemized costs tab
Itemized costs tab Field name Description Procedure code Enter a CPT code or type a period to use the lookup Cost Enter the estimated cost for the procedure Description Displays a description for the procedure code entered Total cost estimate Displays the total of the costs entered above Alternative in-network providers (Required for post-stabilization services) — Enter provider name(s) to be included on the HHS consent form 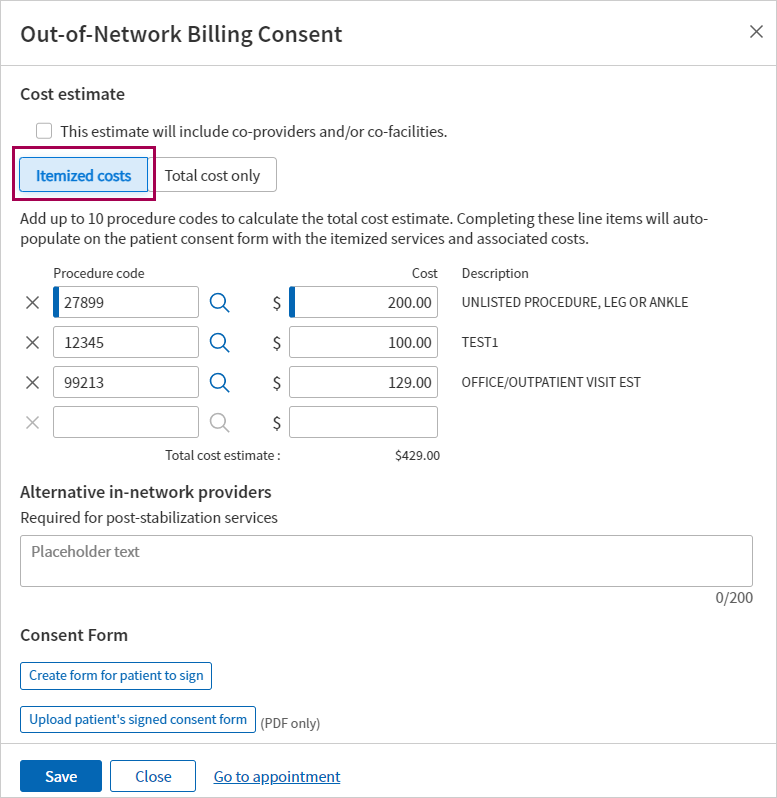
-
-
Click Save.
- If you’re ready to create and send the consent form to the patient, you can do that now. Otherwise, you can save now and return to the appointment later to send the form.
- From either the Eligibility and Phone page or the Appointment page, find appointments that have an Out-of-Network Billing Consent status: Missing a signed patient consent form (appointments in this status already have a cost estimate).
- Click Manage consent. The Out-of-Network Billing Consent window appears.
- Scroll to the bottom of the page and click Create form for patient to sign .
- A digitized version of the HHS Consent Form appears, populated with the patient’s appointment data, cost estimate, and any procedure code(s) and alternative in-network provider(s) entered.
Note: For details on what athenahealth populates in the form, see the athenahealth’s digitized version of the HHS Consent Form in the User Guide — athenaOne Support for Compliance with No Surprise Billing Legislation. -
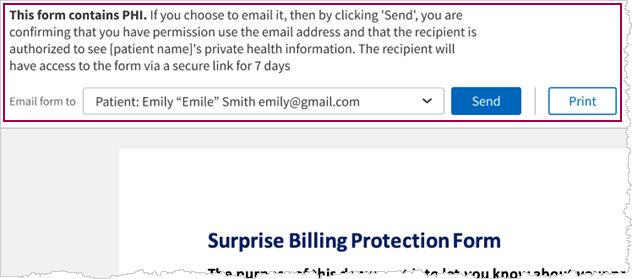
At the top of the form, you can choose to Send or Print the form.
Note: If you selected This estimate will include co-providers and/or co-facilities, the Send button is not available. You must Print the consent form and write in the itemized services and subtotal for each co-provider and co-facility.
-
If you select Send:
- Email form to — Select one of the following:
- Patient (default)
- Another recipient from the list of patient’s contacts on the patient registration record
- Other — Enter the email for a contact that is not listed
- Click Send
- The athenaOne system sends an email with the form.
Important: This form will only be available for 7 days and then will expire and need to be re-generated and resent to the patient
- You will need to have a PDF file of the patient’s signed consent form.
- Save the file to your system.
- From either the Eligibility and Phone page or the Appointment page, find appointments that have the Out-of-Network Billing Consent status: Missing a signed patient consent form.
- Click Manage consent. The Out-of-Network Billing Consent window appears.
- Scroll to the bottom of the window and click Upload patient’s signed consent form .
- Navigate to the location of the signed form on your system, select the file, then click Open.
- Click Save .
A message appears with details about who uploaded the file, along with a date/time stamp.
Important: If you reschedule an appointment, you must re-enter the consent information and re-attach the signed form. Be sure to have a copy of any signed consent forms before moving the appointment.
If a patient’s Out-of-Network Billing consented amount was entered in the appointment AND a signed consent form was attached, you’ll see that amount in the No Surprises Act Consent Service Type Add-On.
Note: On the Claim: Charge Entry tab, Service Type Add-Ons are located between the Illness/Injury section and the Charges section. They allow your practice to provide additional information that is not typically submitted on claims to health insurance payers.
Service Type Add-Ons — Select No Surprises Act Consent.
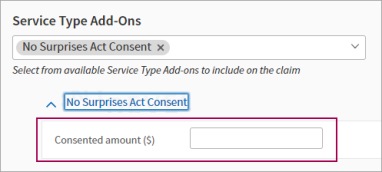
Note: If no signed consent form was uploaded, the cost estimate will NOT carry over to the consented amount in Charge Entry, as it is assumed that the patient did not consent to paying Out-of-Network rates.
If a patient’s consented amount is missing at Charge Entry or Claim Edit: you can check the patient’s appointment to see if a signed consent form was attached, and then enter the consented amount.
-
Check the patient’s appointment to see if a signed No Surprises Act Consent form was attached.
-
Consented amount ($) — Enter the consented amount.
- Continue with your Charge Entry workflow.
You can attach a signed patient consent form in Claim Edit if needed.
- On the Claim Edit page, under Attachments, click Add attachments.
- Click Add New Attachment. The Add New Attachment view appears.
- Type — Select No Surprises Act Consent.
- File — Click Choose file and navigate to the signed consent form on your computer.
- Notes — Enter a note if needed.
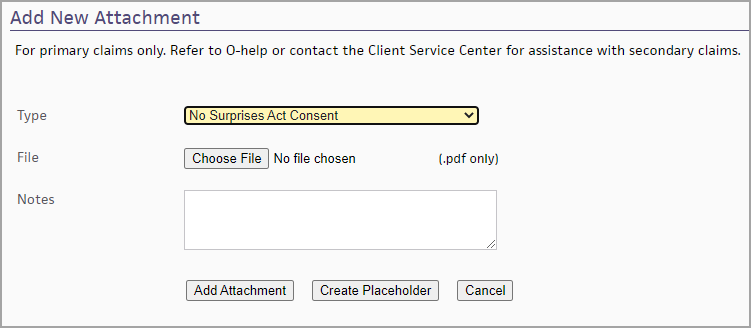
- Click Add Attachment. athenaOne saves the attachment to the claim.
- athenahealth submits the signed patient consent form as a claim attachment along with the claim that goes to the Payer.
Note: If you entered a consented amount but you do not attach a signed consent form to the claim using the No Surprises Act Consent attachment type, a rule (Rule ID: 19709) fires, holding the claim.
-
Claim Note: "Patient consent for the No Surprises Act has not yet been attached to the claim. If the patient consented, then attach the signed consent form to this claim. If not, then remove the consented amount from the No Surprises Act Consent service type add-on."
-
The claim is not submitted to the payer until the signed No Surprises Act Consent form is attached.
The athenaOne Posting Engine references your Patient Billing Settings for Out-of-Network Providers when posting the claim adjudication found on an EOB, to determine:
- When to HOLD a claim for practice review
- When to transfer the balance to the patient without a review
When attempting to post a balance transfer, the athenaOne system reviews the following claim details:
- Billing Provider
- Insurance
- Date of Service
- Department
The athenaOne system will move the claim to HOLD if the following conditions are true:
- The No Surprises Act Consent setting is turned ON for the department on the claim.
- The billing provider is included in an existing out-of-network payer/provider configuration on the Patient Billing Settings for Out-of-Network Providers page, for insurance against which transactions are being posted, and the out-of-network arrangement was in effect on the date of service indicated on the claim.
- A reason code is present on the remittance indicating that the provider is out-of-network for the payer.
Claims are moved to HOLD for practice review, using the kick codes for No Surprise Billing review.
- The kick codes appear in the Claim Notes section.
- The CONTRACTUAL code is used at the charge level.
If the claim does not meet any of the criteria, the athenaOne system transfers the balance to the patient.
If athenahealth manually posts a balance transfer to a patient, we move the claim to HOLD for practice review if the above conditions are true.
- On the Claim Edit page, a message appears to alert the user if the provider was out-of-network for the payer on the service date.
- On the Post Payment page, a message appears to alert the user that the provider was out-of-network for the payer on the service date and the claim will be put on Hold for review.
This is the list of kick codes used to support compliance with the No Surprises Act.
For more information:
- Patient Billing Settings for Out-of-Network Providers
- User Guide — athenaOne Support for Compliance with No Surprise Billing Legislation
| Kick Code | Description |
|---|---|
|
SURPRISEBILLRVW |
This kick code is used by the athenaOne system to HOLD the claim for practice review based on configuration in the Patient Billing Settings for Out-of-Network Providers |
|
SURPRISEBILLADJ |
Use this kick code to adjust off the remaining balance on the claim, after the claim has been reviewed and outstanding charges are not patient responsibility, per No Surprise Billing guidelines.
This kick code is also used by the athenaOne system to automatically adjust off a remaining balance on a claim based on your configuration in the Patient Billing Settings for Out-of-Network Providers |
| SURPRISEBILLPTBAL |
Use this kick code to transfer the balance to the patient, after the claim has been reviewed and approved for patient billing per No Surprise Billing guidelines. |
| SURPRISEBILLXFR |
This kick code is used by the athenaOne system when the claim is being transferred to the secondary payer per No Surprise Billing guidelines |
- Display the Claim Inbox or the Hold By Reason Worklist: On the Main Menu, click Claims and then click Claim Worklists.
The worklist appears in the Task Bar, with links to worklist categories.
Under My Worklists:- Click Claim Inbox (if enabled for your practice)
or - Under HOLD, click By Reason (if using the default claim worklist instead of Claim Inbox)
- Click Claim Inbox (if enabled for your practice)
-
Review claims with the kick code: SURPRISEBILLRVW.
This functionality is available if the No Surprises Act Consent feature has been enabled for your practice. For reference, see the User Guide — athenaOne Support for Compliance with No Surprise Billing Legislation.
- Determine the appropriate action for each claim.
- To complete a full adjustment of the remaining balance on the claim:
- Applies to — Select Patient.
- Select the check boxes for charges you want to adjust off
- Kick reason — Enter SURPRISEBILLADJ.
- To complete a transfer of the balance to the patient:
- Kick reason — Enter SURPRISEBILLPTBAL
- To complete a full adjustment of the remaining balance on the claim:
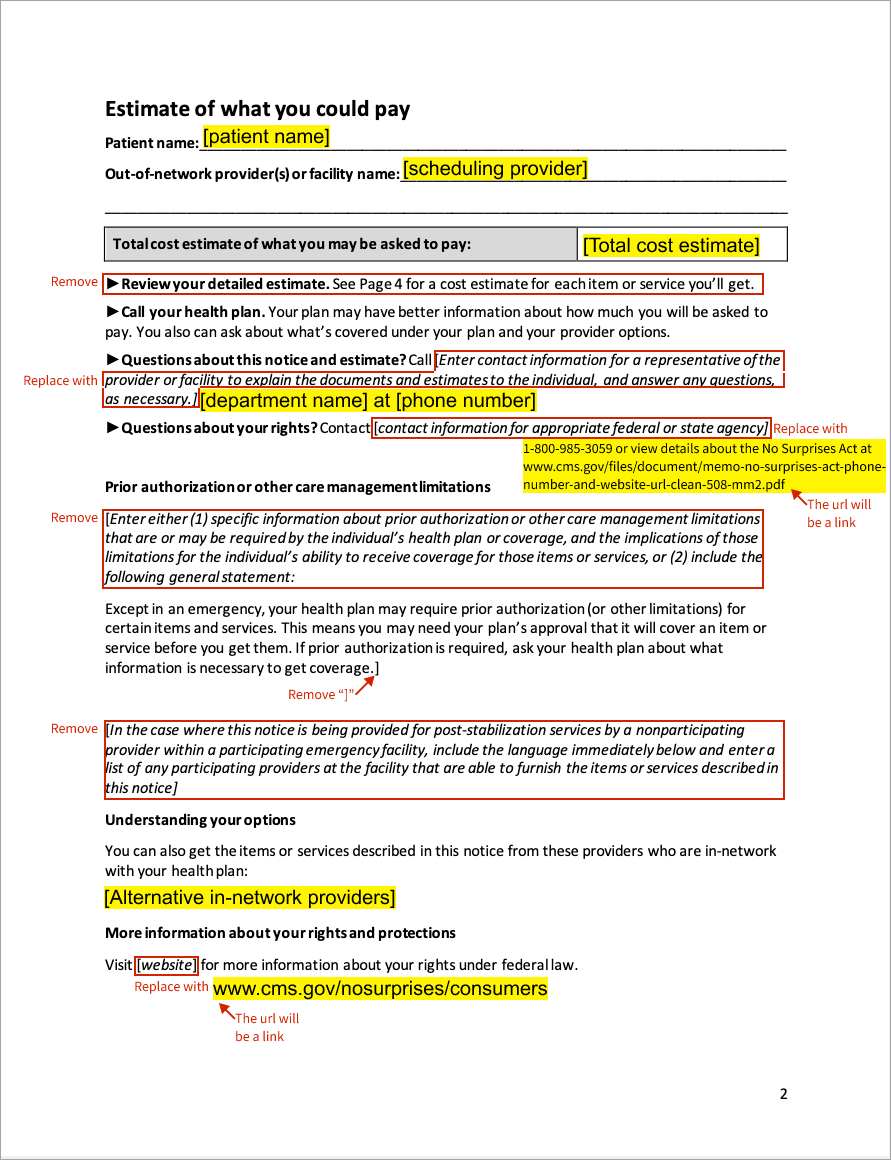
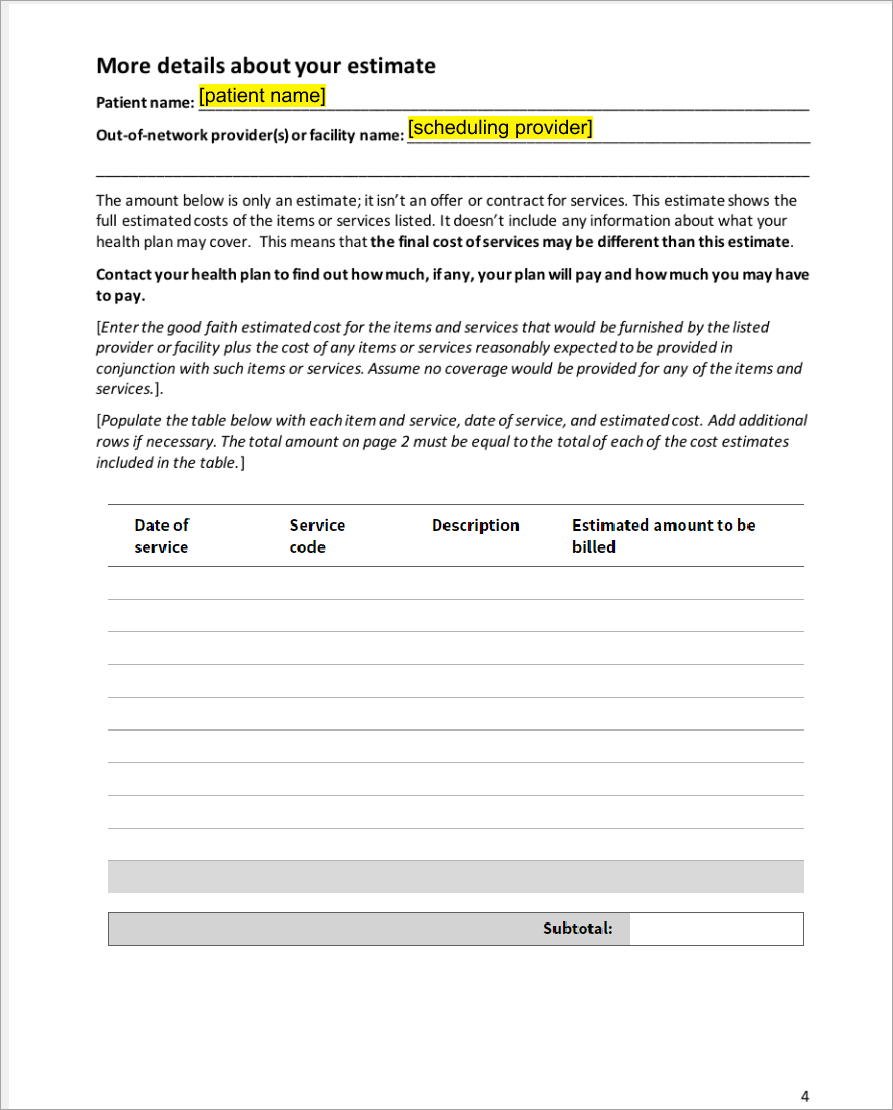
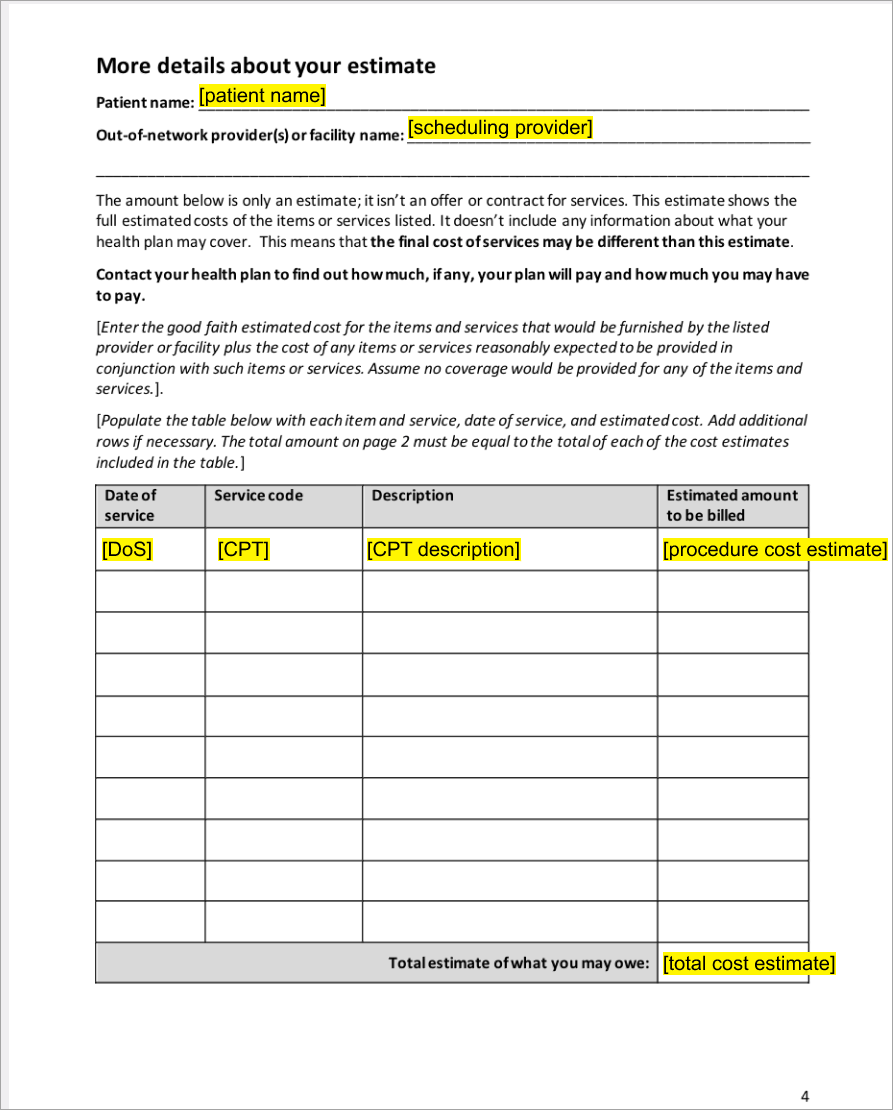
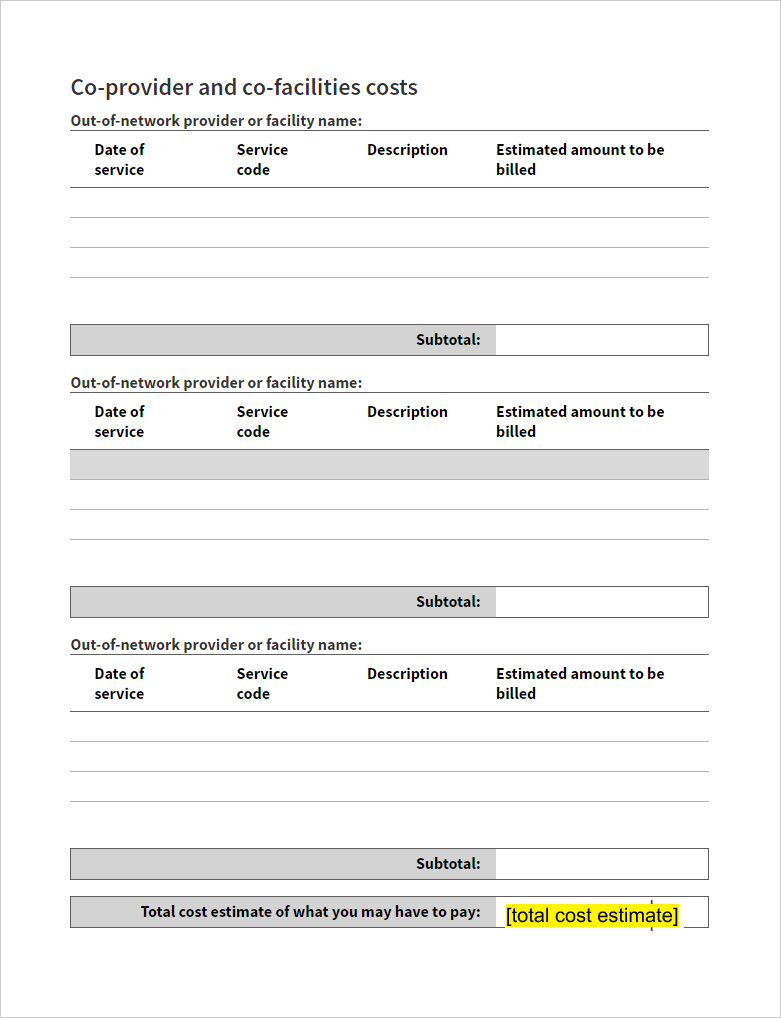
Using the standard Surprise Billing Protection notice and consent form provided by the Department of Health and Human Services (HHS), athenahealth populates the following, based on the patient’s appointment data and the expected procedures and cost estimate entered by your practice:
| Field or text on HHS Form | Populated with athenaOne data | Notes for athenahealth's digitized version of the HHS form |
|---|---|---|
| Patient name | [patient name] | N/A |
| Out-of-network provider(s) | [scheduling provider] | From appointment |
| Out-of-network facility name | [department] | From appointment |
| Total cost estimate of what you may be asked to pay | [total cost estimate] | From Out-of-Network Billing Consent pop-up window |
| “Review your detailed estimate. See Page 4 for a cost estimate for each item or service you’ll get” | N/A | REMOVED in athenaOne form |
|
Questions about this notice and estimate? Call [Enter contact information for a representative of the provider or facility to explain the documents and estimates to the individual, and answer any questions as necessary] |
[department name] at [phone number] | [Enter contact information…] REPLACED with Dept name and phone number from appointment |
| [contact information for appropriate federal or state agency] | N/A |
REPLACED with “1-800-985-3059 or view details about the No Surprises Act at www.cms.gov/files/document/memo-no-surprises-act-phone-number-and-website-url-clean-508-mm2.pdf” |
| [(Enter either (1) specific information about prior authorization or other care management limitations that are or may be required by the individual’s health plan or coverage, and the implications of those limitations for the individual’s ability to receive coverage for those items or services, or (2) include the following general statement:] | N/A | REMOVED in athenaOne form |
| [In the case where this notice is being provided for post-stabilization services by a nonparticipating provider within a participating emergency facility, include the language immediately below and enter a list of any participating providers at the facility that are not able to furnish the items or services described in this notice] | N/A | REMOVED in athenaOne form |
| You can also get the items or services described in this notice from these providers who are in-network with your health plan: | [Alternative in-network providers] | From Out-of-Network Billing Consent pop-up window |
| Visit [website] for more information about your rights under federal law | N/A | [website] is REPLACED with www.cms.gov/nosurprises/consumers |
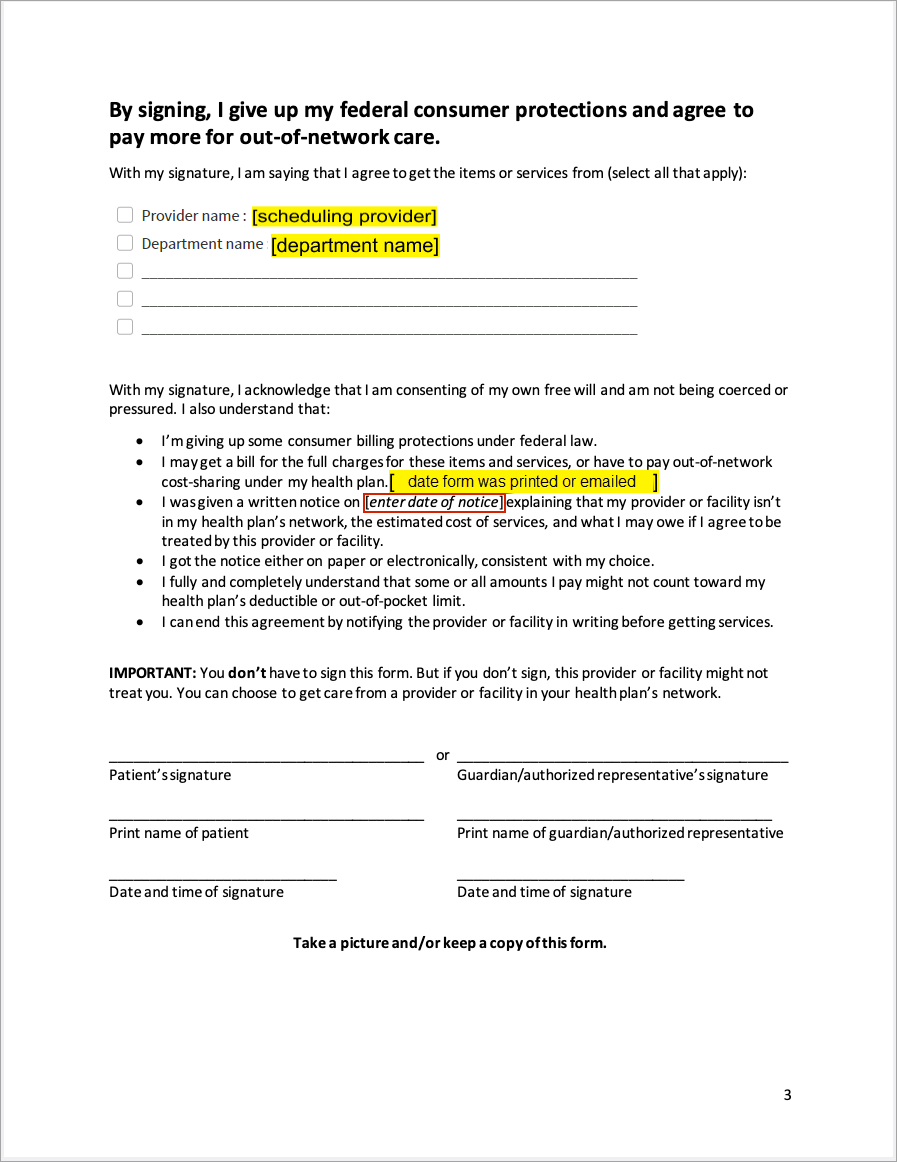
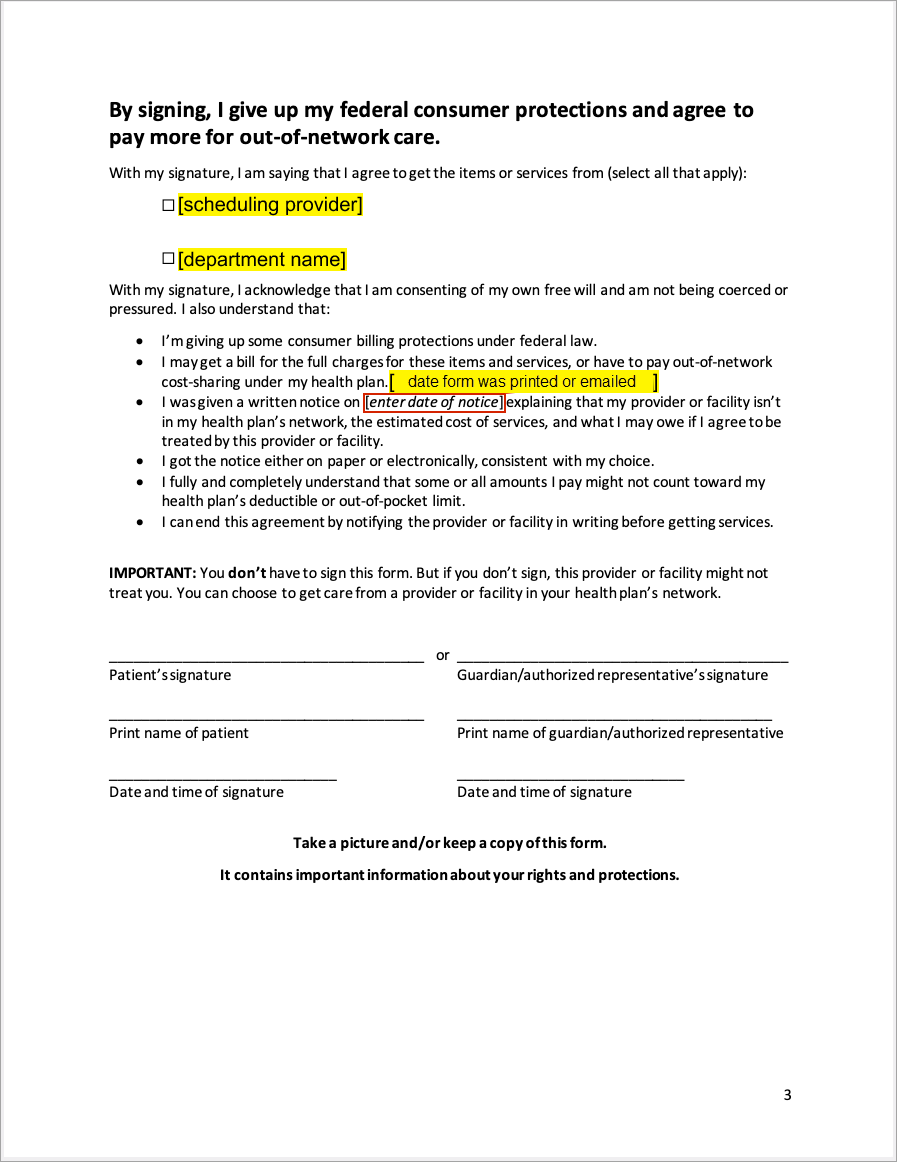
| [enter date of notice] | Date form was printed or emailed | |
| If estimate does NOT include co-providers and/or co-facilities: | ||
| Date of service | [DoS] | From appointment |
| Service Code | [CPT] | From Out-of-Network Billing Consent pop-up window > Itemized Costs |
| Description | [CPT description] | From Out-of-Network Billing Consent pop-up window > Itemized Costs |
| Estimated amount to be billed | [procedure cost estimate] | From Out-of-Network Billing Consent pop-up window > Itemized Costs |
| If estimate includes co-providers and/or co-facilities: | ||
| Out-of-network provider or facility name | N/A | You are responsible for writing in the services and subtotal for each provider and facility. |
| Date of service | ||
| Service Code | ||
| Description | ||
| Estimated amount to be billed | ||
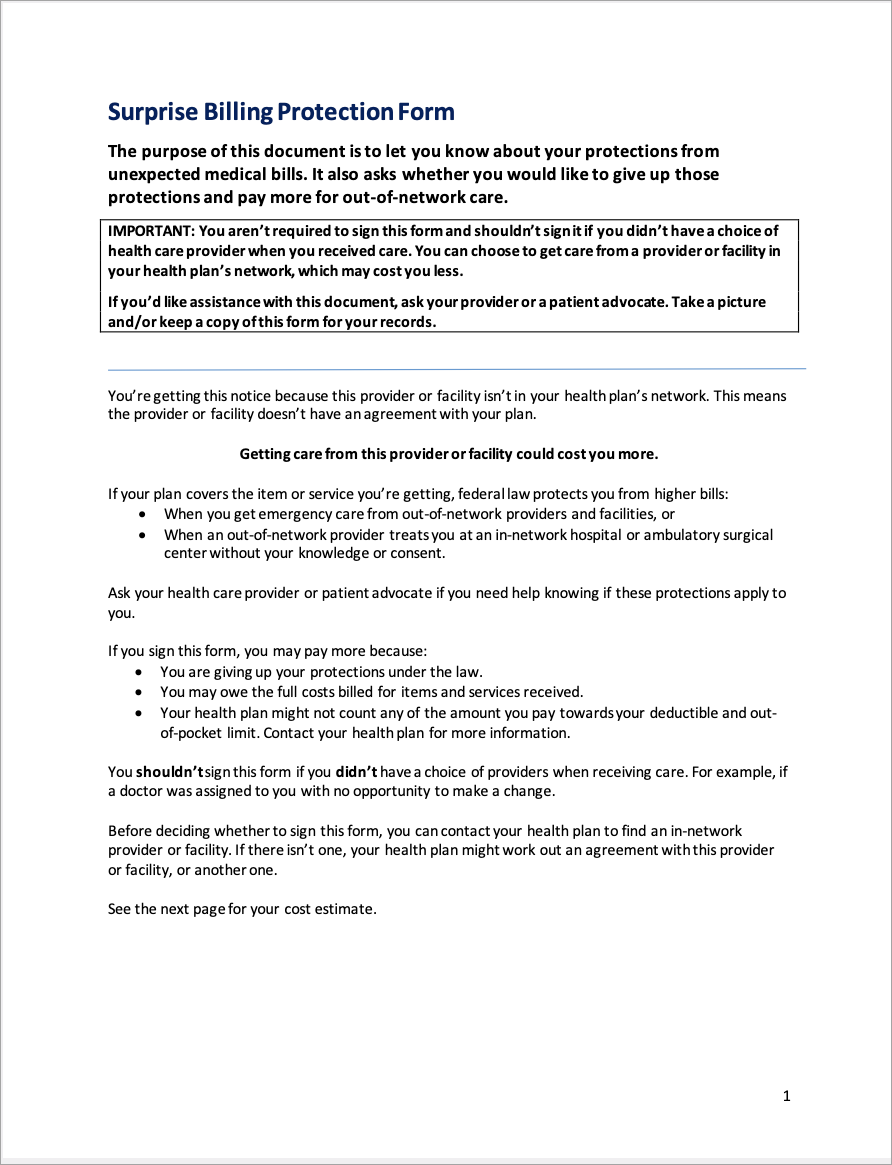
athenahealth's digitized version of the HHS Consent Form
Tip: Click on an image to see an expanded view
Page 1
Page 2
Page 3 (if estimate includes co-providers and/or co-facilities)
Page 3 (if estimate does NOT include co-providers and/or co-facilitiest)
Page 4 (if estimate includes co-providers and/or co-facilities)
Page 4 (if estimate does NOT include co-providers and/or co-facilities)
Page 5 (if estimate includes co-providers and/or co-facilities)
Limitations:
- athenahealth is providing enhancements to help support compliance, but each practice will need to determine if the No Surprises Act obligations impact their organization, how to configure adjudication, and which new options they will use.
- Additional requirements, such as state laws on balance billing, may be applicable to your practice.
- We’ll continue to work closely with our customers to determine where additional enhancements in the athenaOne system can support compliance with any new requirements.