Zero-Pay Review
athenaCollector
athenaOne for Hospitals & Health Systems
This page allows you to create a report of all charges that have no balance outstanding and for which no payment or transfer was made. Zero-pay charges occur when an entire balance is adjusted off with an adjustment type of global, contractual, or "other."
On the Main Menu, click Claims. Under CLAIM MANAGEMENT, click Zero Pay Review
The options available on the Zero-Pay Review page for a given user are aligned with the existing user access that your practice configured on these pages:
When you limit a user's access to view certain providers or departments, those providers and departments do not appear in the filter options or search results of zero-pay reports for that user.
By default, the Zero-Pay Review page allows you to see all saved search criteria that any user at your practice created. (The default version of this feature is the community-based approach.)
You can choose to allow individual users to see only the saved search criteria that the user created. To enforce this user-centric version of the Zero-Pay Review page, you must submit a case to the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
- Display the Zero-Pay Review page: On the Main Menu, click Claims. Under CLAIM MANAGEMENT, click Zero Pay Review.
- If you are running a zero-pay report for the first time, enter your data in the following fields. You can save the selected report criteria for later use when you're done.
- To run a new report, click New report.
- To run a report with criteria that you saved previously, select the saved report at the top of the page.
- Payment post start/end date — Enter a date range, or select
a time period from the menu on the right.
Note: You can set the date range to a maximum of three months. If you need to report on zero payments for a period longer than three months, create separate sets of criteria for the relevant months. For example, create one set of criteria for July 1 through September 30 and another set for October 1 through December 31. - Diagnosis code(s) — To filter or group the report by the diagnosis code
of the mispaid/zero-paid charge, enter one or more diagnosis codes. (When you begin to enter the first diagnosis code, another box appears for the second code, and so on.)
Note: You can include up to 20 diagnosis codes in a set of saved report criteria. - Procedure code(s) — To filter or group the report by the procedure code
of the mispaid/zero-paid charge, enter one or more procedure codes. (When you begin to enter the first procedure code, another box appears for the second code, and so on.)
Note: You can include up to 20 procedure codes in a set of saved report criteria. - Exception procedure code(s) — Enter any procedure codes that you want to exclude from the report (charges with these procedure codes will not be included in the report). You can use wildcards or ranges, for example, 992* or 99000-99100.
Note: You can include up to 20 procedure codes in a set of saved report criteria. - Modifier(s) — Select one or more procedure code modifiers from the menu to filter the report results by modifier.
- Other modifier(s) — Enter any additional procedure code modifiers to filter the report results. You can enter up to four modifiers not found in the Modifier(s) list.
- Procedure charge amount — Enter the minimum and maximum charge for procedures included in the report results. Leave the Max $ field blank to include all charges above the minimum amount.
- Adjustments made by — To filter the report by whether adjustments were made by your practice or by athenahealth, select Client or Athena.
- Provider — To filter the report by supervising provider, select one or more providers from the list.
- Service department — To filter the report by service department, select one or more departments from the list.
- Insurance reporting category — To filter the report by insurance reporting category, select one or more categories from the list.
- Insurance package IDs — To report on mispaid/zero-paid charges for specific insurance packages only, enter insurance package
IDs in the fields.
Note: Insurance package is the plan level of insurance, for example, BCBS — HMO blue. - Custom insurance group — If your practice prefers to report on custom insurance groups, select any custom insurance group that your practice configured from the list.
Note: For more information, see Custom Insurance Grouping and Custom Insurance Group Names. - Payment audit flags — Select one or both of these options to flag worklist items marked for removal from the report or marked for further research.
- Only show charges previously marked for removal from report
- Only show charges previously marked for further research
- Click Save as new criteria to save the selected options for later use.
- Criteria name — Enter a name for the set of search criteria.
- Description — Enter any information regarding the search criteria.
- Automate action — To apply the same action to all future charges, select one of these options: Accept adjudication (accept adjudication on zero-pay claims) or Move to HOLD for action (ZPPRAC) (contest zero-pay claims).
Note: When you configure a set of criteria with an automated action, the ZP Dashboard includes an Automated actions section (if this section did not already exist). - Click Save and run criteria.
- Click Run
report.
The ZP Dashboard appears. On the ZP Dashboard, you can review zero-pay claim information and take action on all claims associated with a specific CPT code.
- Display the Zero-Pay Review page: On the Main Menu, click Claims. Under CLAIM MANAGEMENT, click Zero Pay Review.
- Run a report based on saved criteria or run a new report.
The report summary appears.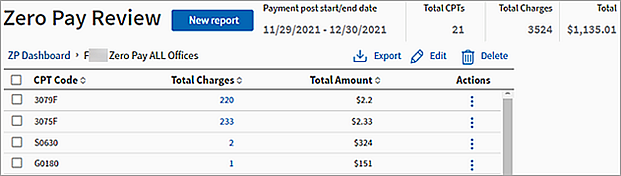
- Click
 Edit.
Edit.
The Edit report criteria page appears. - Edit any necessary data.
- Click Update.
- Display the Zero-Pay Review page: On the Main Menu, click Claims. Under CLAIM MANAGEMENT, click Zero Pay Review.
- Run a report based on saved criteria or run a new report.
The report summary appears.
- Click Export.
The report summary information is downloaded as a .CSV file.
- Display the Zero-Pay Review page: On the Main Menu, click Claims. Under CLAIM MANAGEMENT, click Zero Pay Review.
- Run a report based on saved criteria or run a new report.
The report summary appears.
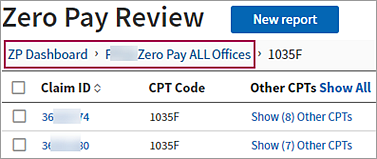
- Click a number in the Total Charges column.
A detailed view of the charges for the CPT code you selected opens and displays the following claim information:- Claim ID
- CPT codes
- Modifiers
- Diagnosis code
- Billed amount
- Paid amount
- Insurance reporting category
- Custom insurance group
- Actions
Note: You can sort the detailed table by a specific column (for example, claim ID or insurance reporting category) by clicking the arrows next to the column heading.
- Click a claim number in the Claim ID column to open a new tab and display the associated claim on the Claim Action page.
- To return to the summary view of the report or to return to the ZP Dashboard, click the name of the saved criteria or click ZP Dashboard above the detailed report.
You can review zero-pay claim information and take action on all claims associated with a specific CPT code from the zero-pay report summary.
- Display the Zero-Pay Review page: On the Main Menu, click Claims. Under CLAIM MANAGEMENT, click Zero Pay Review.
- Run a report based on saved criteria or run a new report.
The report summary appears.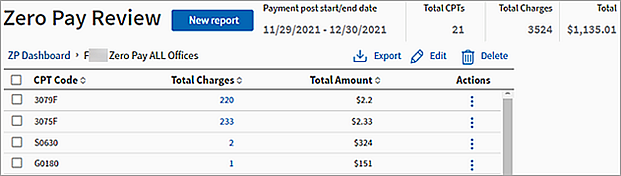
- To take action on a single type of claim, click the action icon
 in the row with the appropriate CPT code.
in the row with the appropriate CPT code. - To take the same action on multiple claims at once, check the box to the left of the CPT Code column for each row that you want to take action on, then click
 Bulk Actions.
Bulk Actions. 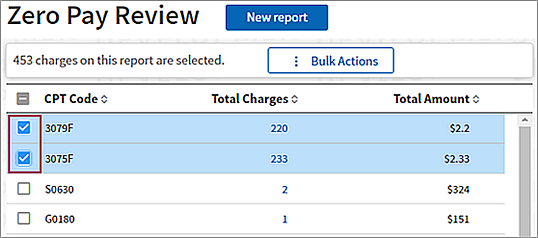
- To take the same action on all claims filtered by your saved search criteria, click ZP Dashboard (above the report summary) to return to your list of saved report criteria. Then, click
 Actions next to the name of the saved criteria that you want to take an action on.
Actions next to the name of the saved criteria that you want to take an action on. 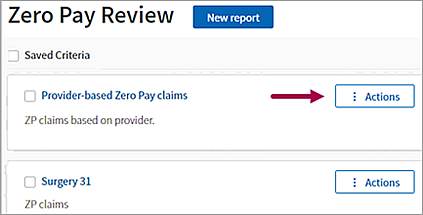
- Select one of the following actions:
- Accept adjudication — Accept all adjudication on associated claims.
- Flag for further research — Mark all associated claims for further review.
Note: You can run a zero-pay report that includes all claims marked for further research. - Clear research flag — Remove the "Mark for further review" flag from all associated claims.
- Move to HOLD for action (ZPPRAC) — Move all associated claims to "HOLD for action (ZPPRAC)" status.
When you select this option, you must add a claim note. Enter your claim note and click Submit. - Send to claims processing wizard — Send all associated claims to athenahealth to be processed.
A small percentage of charges each month are considered "paid" by an insurer, but at zero dollars — in other words, the insurance company did not pay the charge. athenahealth has learned from statistical analysis that a certain percentage of these "zero-pay" claims can be successfully appealed.
athenaOne captures and reports zero-payment information in the Zero-Pay Review. You can focus your search by selecting a specific time frame, procedure code, provider, IRC, procedure charge value, and so forth. You can use the report information to identify claim candidates for appeal, identify payer trends, and identify opportunities for employee training.
The Zero-Pay Review report allows you to view the reason a billed procedure may have received a denial that possibly resulted in a misdirected adjustment and ultimate claim closure. Instead of allowing these claims to remain closed and the denial unchallenged, athenaOne captures the claims as the transaction is posted. The claim containing the zero-paid procedure moves through a series of logic scrubs and ultimately reaches a queue that best explains why it received a zero payment.
For example, you can focus your review on the claims that may only require a correction and resubmission. Therefore, you can first select "Review for appeal: modifier opportunity." This selection shows you all instances where athenaOne used the embedded CCI logic to determine that a procedure could not be billed with another procedure on that claim unless it was accompanied by a modifier.
If you select "Review for appeal: unclear basis for denial," you receive a list of zero-paid procedures that did not meet any clear criteria for why they were not paid. Based on the "scrub" logic, athenahealth believes that these procedures require further research to determine whether they are candidates for appeal.
The selection "Other: Does not follow Physician Fee Schedule logic" lists all zero-paid procedures that have no relative value units (RVUs) assigned within the Medicare National Physician Fee Schedule. athenaOne applies logic only to this set of codes. Examples of what you see in this list are labs, supplies, injectables, or procedures quantified by the local carrier. The procedures that fall into this category are maintained within other fee schedules and assigned RVUs in these schedules.
RVU Report in the Report Library
You can run the RVU Report (on the Other tab of the Report Library) to see relationships between custom, non-standard relative value units (RVUs) and existing procedure codes and report on these combinations. To access the RVU Report, you must be able to view reports in the Report Library.
athenaOne Zero-Pay Logic
The results returned by the Zero-Pay Review report are affected by the following Medicare reimbursement logic factors that are embedded in athenaOne rules.
- Correct Coding Initiative edits (CCI edits) — A list of paired procedure codes that may not be billed together, or may be billed together but only accompanied by an appropriate modifier. CCI edits were created and are maintained by the Centers for Medicare and Medicaid Services (CMS).
- Relative Value Units (RVUs) — Each CPT or HCPCS code used in your practice is assigned a weighted value called an RVU. This numerical value is assigned to a CPT code based on its difficulty and resource consumption. Each RVU is separated into three distinct categories: physician work, practice expense, and malpractice expense. (For more information about RVUs, see Relative Value Units (RVUs).)
RVUs are created and maintained by CMS. Modifications to RVUs appear in the annual revisions of the various national fee schedules, including the National Laboratory Fee Schedule and the Medicare Physician Fee Schedule. The total RVU and the individual category values are shown next to each CPT code listed in the Medicare Physician Fee Schedule sent to your practice each year.
Enhanced zero-pay reporting
athenahealth provides enhanced zero-pay reporting with the Zero-Pay Review. The Zero-Pay Review uses logic based on Medicare payment rules and coding edits (which serve as an industry standard for many payers). These rules and coding edits are defined by the Centers for Medicare and Medicaid System (CMS). This logic helps highlight appealable claims.
Payers sometimes "pay" a claim with $0, meaning that they say "we're not denying this charge, but we're not paying for it either because it's within the global period or it's part of this other procedure performed the same day." athenahealth calls these situations "zero-pays."
athenahealth works such claims for $200 or greater on your behalf by assessing them for "appealability" and submitting appeal letters citing the CCI standards in cases that athenahealth believes have merit. athenahealth first posts the adjustment, and then gathers all the adjustments for assessment. For this reason, you may see zero-paid claims in CLOSED status that may actually still be appealed.
If you find a zero-pay less than $200 that you would like to be appealed, you can tag the claim, and athenahealth will send the appeal. Sometimes you need to provide more information in order for athenahealth to submit an appeal according to CCI, similar to denials.
The Zero-Pay Review report uses logic based on Medicare payment rules and coding edits (which serve as an industry standard for many payers). These rules and coding edits are defined by the Centers for Medicare and Medicaid System (CMS). This logic helps highlight appealable claims. The Medicare-specific payer rules embedded in the wizard focus on:
- Global period rules
- Age/sex compatibility
- Modifier/CPT compatibility
- Correct Coding Edits (CPT combination sets that require modifiers, cannot be billed with a modifier, are mutually exclusive, or are component codes of another CPT)
When a claim is classified as "appealable," it does not mean that athenahealth expects payment. It means that athenahealth believes that further investigation may be warranted.
Sometimes you may disagree with our assessment of the legitimacy of a denial or zero-pay; that is, athenahealth believes that the denial is legitimate, but you do not. In those cases, you may request one courtesy appeal on the claim, which we will prepare and submit for you.
The GLOBALRVW hold status makes it easier to review zero-paid claims for potential appeal or resubmission. Claims move to the GLOBALRVW hold status when the claim or charges on the claim are classified as a global service and result in a zero-paid claim or charge by the payer. athenahealth provides detailed recommendations to resolve the hold in the claim notes.
Note: Only claims with certain procedure code and payer combinations move to the GLOBALRVW hold status. Over time, athenahealth will add more procedure code and payer combinations to give you a more comprehensive review workflow for zero-paid claims and charges.
To view claims in the GLOBALRVW hold status:
- Generate the claims worklist: On the Main Menu, click Claims > Claims Worklists. The View Claims Worklists appear in the Task Bar, with links to worklist categories.
- In the task bar, under HOLD, click By Reason.
The Hold by Reason worklist appears in the Workspace. - In the Reason column of the table, locate the GLOBALRVW hold reason and then click the dollar amount in the Amount column.
The list of claims associated with the GLOBALRVW hold reason appears in the Workspace.
The following kick codes are used to move the zero-paid claims through appeal or resubmission by athenahealth:
- ZPDOC — athenaOne kick code used to move a claim from CLOSED status to practice HOLD. This kick code creates a placeholder for medical documentation that the practice will be requested to upload prior to moving the claim to a new status.
- ZPPRAC — athenaOne kick code used to move a claim from CLOSED status to practice HOLD. This kick code does NOT create a placeholder for document attachments. It is used by athenahealth if documentation is not required but the practice may need to review for appeal or make a correction to the claim for resubmission.
- PLSAPPEAL — Practice kick code used to move a claim from HOLD to CBOHOLD after it is determined by the practice that the claim warrants an appeal. PLSAPPEAL can be used after the practice uploads documentation to support the appeal.
- DRPBILLING — Practice kick code used to re-drop a claim after corrections are made to a claim. If resubmissions to the payer require review for all required information, the claim is routed to CBOHOLD before dropping to the payer.
- RECONSIDERATION — athenaOne kick code used to move the claim from CBOHOLD to BILLED status after an appeal is submitted.
- RVCLOSE — Practice kick code used to manually close a claim if you determine that the claim was processed correctly by the payer and no additional payment is expected.
After documentation is attached, scroll down to the Go to full Claim Note link at the bottom of the Claim Edit page. In the Action taken/note source field, select "Generic Note/From Other Source." In the Kick reason field, enter "PLSAPPEAL" and then click Save to request that athenahealth file an appeal.
The zero-pay kick codes ZPDOC and ZPPRAC appear in your HOLD work queues. Please use the kick codes specified above to re-route the claims back to CBOHOLD or to close the claims.
Appeal filing limits are enforced by payers. Filing promptly increases your chance of a successful appeal.
Note: For all other claims (including zero-pay charges under $500), you should follow the usual appeal process.
Your practice can initiate zero-paid appeals. You can also follow up on zero-payments not included in the current zero-pay follow-up service. If you determine that a zero-pay charge requires an appeal, you can "drill down" into the claim.
The Zero-Pay Review page allows you to view closed charges that have received a zero payment and were adjusted off based on the primary insurer's payment rules. These claims may qualify for an appeal and should be reviewed on a weekly basis to determine whether they were adjudicated correctly and whether an appeal can be made.
athenahealth recommends that you review the zero-pay report to ensure that your practice receives the payment amount for services that it expected to receive.
You can click any table cell with a non-zero number of charges to see the claim ID number and other charge details. You can then click the claim ID number on the charge details page to open claim on the Claim Action page.
You can click any report column to sort the report in ascending or descending order.
| Create report criteria | |
| Payment post start/end date |
Enter a date range for listed charges, or select a time period from the menu on the right. A charge is listed if it had an adjustment posted on or between these dates. Note: You can set the date range to a maximum of three months. If you need to report on zero payments for a period longer than three months, create separate sets of criteria for the relevant months. For example, create one set of criteria for July 1 through September 30 and another set for October 1 through December 31. |
|---|---|
| Diagnosis code(s) |
To filter or group the report by the diagnosis code of the mispaid/zero-paid charge, enter one or more diagnosis codes. (When you begin to enter the first diagnosis code, another box appears for the second code, and so on.) Note: You can include up to 20 diagnosis codes in a set of saved report criteria. |
| Procedure code(s) |
To filter or group the report by the procedure code of the mispaid/zero-paid charge, enter one or more procedure codes. (When you begin to enter the first procedure code, another box appears for the second code, and so on.) Note: You can include up to 20 procedure codes in a set of saved report criteria. |
| Exception procedure code(s) |
Enter any procedure codes that you want to exclude from the report (charges with these procedure codes will not be included in the report). You can use wildcards or ranges, for example, 992* or 99000-99100. Note: You can include up to 20 procedure codes in a set of saved report criteria. |
| Modifier(s) |
Select one or more procedure code modifiers from the menu to filter the report results by modifier. |
| Other modifier(s) | Enter any additional procedure code modifiers. You can enter up to four modifiers not found in the Modifier(s) list. |
| Procedure charge amount |
Enter the minimum and maximum charge for procedures included in the report results. Leave the Max $ field blank to include all charges above the minimum amount. |
| Adjustments made by |
To filter the report by whether adjustments were made by your practice or by athenahealth, select Client or Athena. |
| Provider |
To filter the report by supervising provider, select one or more providers from the list. |
| Service department |
To filter the report by service department, select one or more departments from the list. |
| Insurance reporting category |
To filter the report by insurance reporting category, select one or more categories from the list. |
| Insurance package IDs |
To report on mispaid/zero-paid charges for specific insurance packages only, enter insurance package IDs in the fields. Note: Insurance package is the plan level of insurance, for example, BCBS — HMO blue. |
| Custom insurance group |
If your practice prefers to report on custom insurance groups, select any custom insurance group that your practice has configured from the list. Note: For more information, see Custom Insurance Grouping and Custom Insurance Group Names. |
| Payment audit flags |
Select one or both of these options to flag worklist items marked for removal from the report or marked for further research.
|
| Save as new criteria fields | |
| Criteria name | Enter a name for the set of search criteria. |
| Description | Enter any information regarding the search criteria. |
| Automate action |
To apply the same action to all future charges, select one of these options:
|
| Column headings on the report | |
| CPT Code | The CPT code associated with the zero-paid claims. |
| Total Charges | The total number of zero-paid claims associated with the CPT code. |
| Total Amount | The total dollar amount related to the zero-paid claims. |
| Actions |
Click the action icon
|
| Column headings for detailed report | |
|---|---|
| Claim ID |
The claim identification number. Click the claim ID number to open a new window in which you can edit the claim on the Claim Action page. |
| CPT Code | The CPT code associated with the zero-paid claims. |
| Other CPTs | If the claim includes other CPT codes, you can click Show (n) Other CPTs to display them. |
| Modifier | Any modifiers applied to the claim. |
| Diagnosis Code | The diagnosis codes associated with the claim. |
| Billed Amount | The billed amount in dollars for the claim. |
| Paid Amount | The amount paid to date for the claim. |
| Insurance Reporting Category | The claim's insurance reporting category. |
| Custom Insurance Group | The name of the custom reporting group, if applicable. |
| Actions |
Click the More Actions icon
See below for more detail on what each action does. |
| Actions |
|
| Accept adjudication |
Select this option to remove the selected zero-paid charges from the report. |
| Flag for further research |
Select this option to flag the selected zero-paid charges for further research. Select this option when you aren't completely sure whether an appeal is warranted and just want a simple reminder to review the claim again.
Charges flagged for further research are highlighted in the worklist. |
| Clear research flag |
Select this option to clear any flags from the checked zero-paid charges. |
| Move to HOLD for action (ZPPRAC) Claim note text: |
Select this option to assign the selected zero-paid charges to HOLD status for action ZPPRAC. Note: Claims moved to HOLD are permanently deleted from the zero-pay report.
Select this option when an appeal is warranted. A claim note field and a warning message appear to alert you that athenaOne is about to re-open a closed claim. Click yes to move the claim to HOLD status with the ZPPRAC kick code.
After you research the claim:
|