 User Guide — athenahealth Claim Appeal on Your Behalf
User Guide — athenahealth Claim Appeal on Your Behalf
This guide describes the appeal workflow outside of payer-specific guidelines and requirements. For information about kick reasons that may require an appeal as a corrective action, see How to Correct Claims in Hold Queues.
The athenahealth automated logic determines the type of denial. The denial needs to be addressed by athenahealth under these circumstances:
- If the denial is due to a requirement for supporting documentation, athenaOne inserts a document placeholder (Claim Resolution Rule #2804).
- If the EOB provides clear denial codes and remarks, athenahealth addresses the payer's concerns. The claim is then appealed or resubmitted according to the payer-specific requirements.
- If the EOB provides vague or undefined denial codes and remarks, athenahealth performs the necessary research to determine why the claim was denied by the payer. This research may involve using the payer Web portal or making a call to the payer.
If athenahealth cannot resolve the denial without your input, athenahealth moves the claim to the HOLD or MGRHOLD queue based on the information received. Claim notes provide the necessary information for your staff to address the denial, update the claim, or attach supporting documentation. Claim notes may be provided by our automated system or by an athenahealth user.
- After the required corrections are made, use the kick code DRPBILLING.
Important: After you apply the DRPBILLING kick code, the next action shown may be a CORRECT rule firing. This logic is working as intended; athenahealth is ensuring that all appropriate resubmission information is on the claim. - After you attach the requested documents, use the kick code PLSAPPEAL. The PLSAPPEAL kick code routes the claim back to athenahealth staff to resubmit the claim or appeal the denial.
athenahealth confirms the validity of the appeal request, including (but not limited to) confirmation that the payer accepts appeals, as well as the use of appeal forms. athenahealth performs these functions:
- Reviews the full claim history, the current denial, and your requests.
- Submits the appeal based on payer-specific requirements.
-
In summer 2021, we launched a new appeals process that leverages payer portals instead of paper mail, reducing errors and processing time.
- We kicked off with some of the larger payers and portals, and will add more as we establish secure connections.
- Each time we add a payer or portal, we roll it out to all athenahealth customers in waves, and you’ll receive a notification when a new payer/portal combination is live for your organization.
- Please refer to the Portal Appeals: payers and portals currently live Success Community article for details of which payer/portal combinations we're currently handling appeals with online.
-
When you see claim notes with the kick code PORTALAPPEAL, that means we’ve submitted an appeal through the payer portal, and you’ll find a confirmation number in the note to help track the claim.
If you want to appeal a claim, you must correct the claim as required, or you must attach (or fax) supporting documentation (medical records, labs, etc.). Finally, use the Claim Action or Claim Edit page as follows.
Note: To display the Claim Action page, select a claim in HOLD or MGRHOLD status from any of these pages: Workflow Dashboard, View Claims Worklists, Claim Inbox, non-clinician home page, A/R Aging Wizard, Activity Wizard, Zero-Pay Review, Fully Worked Receivables, or click Claim Action Page on the Claim Edit page.
You can appeal a claim denial after the claim has been submitted to the payer (the Hold Summary status is "Post-Bill").
- Display the Claim Action page: Select a claim from the Workflow Dashboard, Claim Worklist, or click the Claim Action Page link on the Claim Edit page.
- Review the claim information and existing documentation.
- Actions — Select Resubmit to Payer from the menu.
The Resubmission request page appears.
Note: You can only submit one resubmission request at a time. If you have an on-going request, you cannot access the resubmission workflow until the pending one is resolved. - Applies to — Select the payer whose denial you are appealing: Primary Insurance or Secondary Insurance.
- Resubmission type — Select a resubmission type from the menu.
- Under Optional information, enter the following information if applicable for your resubmission request:
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
Notes:- Documents that are already attached to the claim appear in the Existing Attachments section. These documents are available for athenahealth teams to use when constructing a resubmission, and do not need to be reattached via this workflow.
- You can upload only one document via the resubmission workflow. To upload multiple documents, please complete that workflow on the claim itself before coming to this page. Uploading the documents prior to completing the new resubmission workflow allows those documents to be part of the documentation that athenahealth teams select from.
- The Attachment type field sets the type of document you are attaching; it does not filter the medical documentation check boxes located in the Documents section.
- Mail-to address — Click Choose a mail-to address to expand the section. If you don’t see the appropriate address, click add a new mail-to address and enter a new address.
Best practice: To look for additional addresses, search for the address in the Find address field. - Reason for resubmission — Enter the reason for resubmitting the claim.
Note: This field has a 2000-character limit. - Claim note — Click Include claim note (internal) to expand the section. Enter any internal notes for your athenaOne practice users. Describe the reasons why the claim should be appealed, list facts to support the appeal, and indicate whether you attached any supporting documentation or faxed any documentation to athenahealth (you may want to do so).
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
- Click Submit request. This action applies the PLSPPEAL kick code and moves the claim to athenahealth to review for payer-specific requirements.
A message appears indicating that the resubmission was successfully submitted to athenahealth.
Important: We've built automation for highly predictable resubmission scenarios: When the claim is kicked with PLSAPPEAL, athenaOne automatically executes a resubmission based on the appropriate scenario. (We’re actively building tools that limit the effects of this automation by resubmission type. If you disagree with athenaOne’s automation for the resubmission, submit a case via the Success Community: Main Menu > Support > Contact Client Support Center > Billing & Claims > Correct/Resubmit Claim > Create Online Case.) - An address validation window may appear if the address you entered could not be verified. Choose the address you want to use by selecting either Correct Address or You Entered, and then Confirm address.
When you appeal a claim, attach or fax supporting documentation (medical records, labs, etc.) and follow these steps.
Note: For instructions on attaching documents to claims, see the Manage Attachments page.
- Display the Claim Edit page:
 In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions..
In the text box at the top right of your screen, enter the claim number and select Claim ID from the menu. The Find tool looks for an exact claim ID match. To search for claims, you must have claim billing user permissions.. - Review the claim information and existing documentation.
- In the Add note section, click Resubmit to Payer.
The Resubmission request page appears.
Note: You can only submit one resubmission request at a time. If you have an on-going request, you cannot access the resubmission workflow until the pending one is resolved. - Applies to — Select the payer whose denial you are appealing: Primary Insurance or Secondary Insurance.
- Resubmission type — Select a resubmission type from the menu.
- Under Optional information, enter the following information if applicable for your resubmission request:
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
Notes:- Documents that are already attached to the claim appear in the Existing Attachments section. These documents are available for athenahealth teams to use when constructing a resubmission, and do not need to be reattached via this workflow.
- You can upload only one document via the resubmission workflow. To upload multiple documents, please complete that workflow on the claim itself before coming to this page. Uploading the documents prior to completing the new resubmission workflow allows those documents to be part of the documentation that athenahealth teams select from.
- The Attachment type field sets the type of document you are attaching; it does not filter the medical documentation check boxes located in the Documents section.
- Mail-to address — Click Choose a mail-to address to expand the section. If you don’t see the appropriate address, click add a new mail-to address and enter a new address.
Best practice: To look for additional addresses, search for the address in the Find address field. - Reason for resubmission — Enter the reason for resubmitting the claim.
Note: This field has a 2000-character limit. - Claim note — Click Include claim note (internal) to expand the section. Enter any internal notes for your athenaOne practice users. Describe the reasons why the claim should be appealed, list facts to support the appeal, and indicate whether you attached any supporting documentation or faxed any documentation to athenahealth (you may want to do so).
- Documents — Select medical documents or upload a new attachment to expand the section. Select the type of documentation to add. This documentation should support your appeal.
- Click Submit request. This action applies the PLSPPEAL kick code and moves the claim to athenahealth to review for payer-specific requirements.
A message appears indicating that the resubmission was successfully submitted to athenahealth.
Important: We've built automation for highly predictable resubmission scenarios: When the claim is kicked with PLSAPPEAL, athenaOne automatically executes a resubmission based on the appropriate scenario. (We’re actively building tools that limit the effects of this automation by resubmission type. If you disagree with athenaOne’s automation for the resubmission, submit a case via the Success Community: Main Menu > Support > Contact Client Support Center > Billing & Claims > Correct/Resubmit Claim > Create Online Case.) - An address validation window may appear if the address you entered could not be verified. Choose the address you want to use by selecting either Correct Address or You Entered, and then Confirm address.
- On the Claim Edit page, scroll down to the Claim Notes section at the bottom of the page.
- Review the claim notes.
- If athenahealth has researched the denial with the payer, a detailed description is included.
- If there is an EOB or letter from the payer, click the link to review it.
- Scroll down to the Add Note section.
- Applies to — If needed, select the payer type for the claim note: Primary Insurance or Secondary Insurance.
- Status — Do not change the status.
- Kick reason — Enter PLSAPPEAL.
- Note — Enter a note about the appeal.
Important: To assist athenahealth users who are finalizing your appeal package, please clearly label and differentiate between your appeal note (payer facing) and your internal claim note, for example: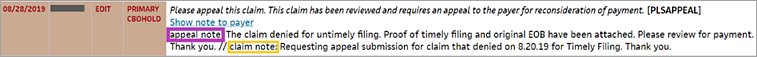
- Click Save.