How UDS Reporting Identifies a UDS visit
athenaCollector + athenaClinicals
This is a topic that focuses on Uniform Data System (UDS) reporting. Use this topic to determine how a UDS visit is indicated for UDS reporting using the default logic as determined in the UDS Reporting — CPT Inclusion-Exclusion List.
This topic also reviews the UDS overrides a practice may use through the Fee Schedule or Clinical Add-Ons section in the encounter or the claim.
- UDS Reports (user guide)
- Run UDS Reports
- QA UDS Table 3A
- QA UDS Table 3B
- QA UDS Table Patients by Zip
- QA UDS Table 9D
- QA UDS Table 6A
- QA UDS Table 5
- QA UDS Table 5 – Selected Services Detail Addendum
- QA UDS Table 4
- QA UDS Tables 7B and 7C
- QA UDS Table 7A
- QA UDS Table 6B
- UDS Provider Type Mapping
- UDS Reporting Overview — CPT Inclusions and Exclusions
-
I am billing for a visit I marked as a UDS visit, but patient/visit is not pulling into the UDS tables.
-
Why isn’t this UDS visit showing in the Quality Tables?
-
I have marked the encounter as a UDS visit, but the patient/visit is not on the Quality Tables.
-
I have updated my Fee Schedule to indicate procedure code is a UDS visit, but the patient/visit is not in the Quality tables.
-
I am billing this visit as a UDS visit, why isn’t it showing in the UDS tables?
UDS is used by FQHCs for reporting purposes. Encounters and claims can be marked with UDS indicators so practices can report on service utilization.
UDS visits are identified using procedure codes billed on the claim associated with an encounter or on the encounter itself. An encounter must be identified as a UDS visit for the patient/encounter to show in UDS reporting. The list of CPT codes that are automatically included or excluded from the logic are in the CPT Inclusion-Exclusion list. This will be referred to as the default logic.
Order Groups, or orders-only encounters, are excluded from counting as a UDS Visit. For more information, read the Order Groups topic.
-
From the topic UDS Reporting — CPT Inclusion-Exclusion List, choose the table with the applicable year (Tab selection/order may vary based upon the year).
-
Search for the procedure code in each of the tables by using CTRL-F function of your browser window or by manually searching.
- Tables indicating Inclusion and Telehealth: Identifies which procedure codes qualify an encounter as a UDS visit.
- If the procedure code is in this table but is not pulling into your tables, please create a case via:
- Navigate to Support > Create a Case or Call, select Quality Management, and click on Quality Management/P4P.
- Be sure to include the following in your case:
- Program UDS
- Patient and/or claim examples
- Billing codes
- Tables/reports and measures affected (Some tables have multiple measures)
-
Table indicating Exclusion: Identifies procedure codes that will not be identified as a UDS visit (this list may not be exhaustive. For instance, state-specific CPT codes, such as California Z-codes, are not included. However, if the procedure code cannot be found in any of the tabs, it is safe to assume that it will not automatically be identified as a UDS visit.)
-
Please proceed to Steps to Override the Default Logic to determine who to ensure the code is included if you believe it should be captured.
A practice may override default functionality using the Fee Schedule in Billing Admin or through use of Clinical Add-Ons Section in the encounter or the Service Type Add-ons section in the claim. Changing the fee schedule will affect all encounters and claims from the beginning of the calendar year onward with the overridden procedure code, or the beginning of the previous year if you make the change before April 1st Fee schedule overrides take effect overnight. The Clinical Add-On and Claim Service Type Add-on allow for Clinician discretion per encounter and can be seen in reports immediately. Please consult the appropriate O-help articles listed below for more information on this functionality.
Manually including or excluding a visit as a UDS visit will appropriately include or exclude the patient for that encounter in the reportable patient population. However, Quality measures (as found in the Quality Management Report and the Quality Tab of the patient chart) may not be impacted because measure specification logic must also be satisfied. Individual Quality Measures have their own set of eligible CPT codes which are independent of the CPT Inclusion-Exclusion List and are not impacted by the Fee Schedule override.
-
A practice may add new or edit existing procedure codes in the Fee Schedule. There is a UDS visit field which can be modified, as needed.
-
To access Fee Schedule, navigate to Settings > Admin > Billing > Fee Schedule.
-
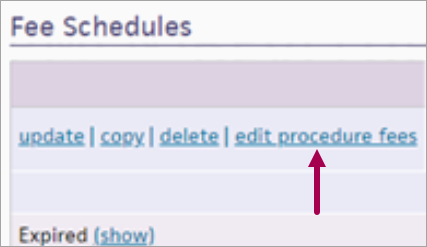
Click on edit procedure fees.
-
Enter the code into the Procedure Code Look Up and Filter
-
Click on Update
-
Scroll to UDS visit
-
Is UDS Visit set to No? Encounters associated with this procedure code will not be identified as UDS visits.
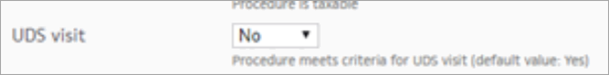
-
If you’ d like to update the drop-down, please note it will affect all claims and associated encounters using the selected Fee Schedule.
-
Choose new drop-down to No
-
Click Save
-
Is UDS Visit set to Default? Encounters associated with this procedure code will use the default logic. You can see this default value in the dropdown description: (default value: Yes or No).
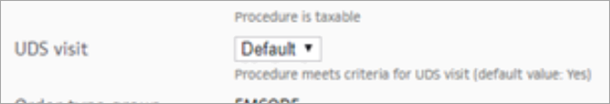
-
If the CPT code is on the Exclusion List, then it would not be considered a UDS visit.
-
If the CPT code is on CPT Inclusion List or Inclusions Based on Provider and is not showing on your UDS reports please open a case via:
-
Navigate to Support > Create a Case or Call, select Quality Management, and click on Quality Management/P4P.
-
Be sure to include the following in your case:
-
Program UDS
-
Patient and/or claim examples
-
Billing codes
-
Tables/reports and measures affected (Some tables have multiple measures)
-
-
-
Is UDS Visit set to Yes? Encounters associated with this procedure code will be identified as UDS visits.
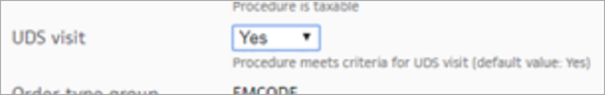
-
If the procedure code is set to Yes and the visits are not pulling into UDS reporting, create a case via:
-
Navigate to Support > Create a Case or Call, select Quality Management, and click on Quality Management/P4P.
-
Be sure to include in your case:
-
Program UDS
-
Patient and/or claim examples
-
Billing codes
-
Tables/reports and measures affected (Some tables have multiple measures)
-
-
Note:
-
You can override procedure codes with modifiers and treat them separately from the base procedures code. In other words, if you wish to tread 99213 different from 99213,XX you can do so. Please see this release note for detailed instructions.
-
Adding or removing a UDS Fee Schedule override takes effect overnight. Your UDS reports will not change until then. You may run reports with the Run Offline checkbox selected, and they will have the updated CPT codes when they’re run overnight.
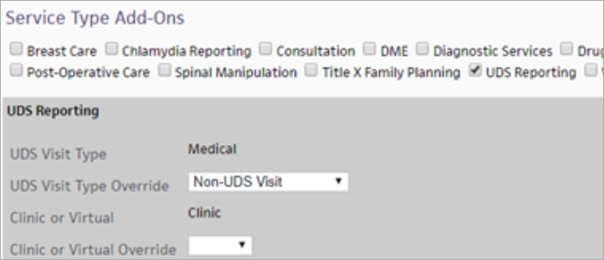
Provider adds UDS reporting as a Clinical Add-On in either the Intake or the Exam Review in the encounter. This action can be seen by viewing Service Type Add-Ons on the associated claim and the on the Billing Tab of an encounter prior to claim creation.
When troubleshooting from a claim:
-
Search for claim by patient or by claim number
-
View the claim
-
Scroll to find Service Type Add On - see O Help article Clinical Add-Ons Section for more information
-
Find the UDS Reporting checkbox:
-
UDS Reporting unchecked: the visit will use the default logic as indicated in the CPT Inclusion-Exclusion Report.
-
-
UDS checkbox is checked and the drop down is Non-UDS Visit: The visit will not be identified as a UDS visit.|
-
If the UDS checkbox is checked and a value is entered in the Visit Type dropdown: The visit will be identified as a UDS visit.
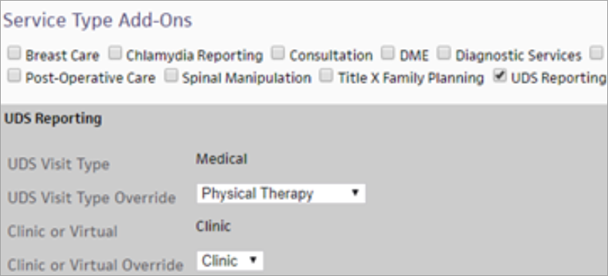
Note: This functionality depends upon an encounter having an associated claim, otherwise the encounter will default to the UDS CPT Inclusion-Exclusion List logic. -
If the visit is marked on the claim as a UDS visit, and is not in UDS reporting, create a case via:
-
Navigate to Support > Create a Case or Call, select Quality Management, and click on Quality Management/P4P.
- Be sure to include in your case:
- Program UDS
Patient and/or claim examples
Billing codes
Tables/reports and measures affected (Some tables have multiple measures)
-