Self-Pay Reminder Messages
This page allows you to view the Self-Pay reminder messages sent to patients and guarantors, as well as the reminder schedule configured for each dunning level. Self-Pay messages are sent via phone calls, email messages, text messages, and the Patient Portal, based on the practice or provider group configuration.
Note: The wording of the Self-Pay messages (phone, email, and text) has been vetted by athenahealth and cannot be edited.
Important: [PRACTICENAME] pulls from the Content Management page. [PRACTICEURL] and [WEBPORTALURL] pull the following items from the Communicator Branding page, respectively: Patient Portal URL and website URL.
On the Main Menu, click Settings![]() >Communicator. In the left menu,under Practice Links — Self-Pay, click Self-Pay Reminder Messages
>Communicator. In the left menu,under Practice Links — Self-Pay, click Self-Pay Reminder Messages
To access this page, you must have the Communicator Admin or Communicator: Self-Pay Messages permission.
The Self-Pay Reminder Messages page displays the Self-Pay reminder messages sent to patients and guarantors, as well as the reminder schedule configured for each dunning level. Self-Pay messages are sent via phone calls, email messages, text messages, and the Patient Portal, based on the practice or provider group configuration.
Note: The wording of the Self-Pay messages (phone, email, and text) has been vetted by athenahealth and cannot be edited.
To access this page, you must have the Communicator Admin or Communicator: Self-Pay Messages permission.
- Display the Self-Pay Reminder Messages page: On the Main Menu, click Settings
 >Communicator. In the left menu,under Practice Links — Self-Pay, click Self-Pay Reminder Messages.
>Communicator. In the left menu,under Practice Links — Self-Pay, click Self-Pay Reminder Messages.
Your Self-Pay reminder message settings appear at the top of the page. - Provider Group — If your practice uses provider groups, select a provider group from the menu.
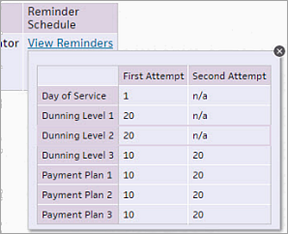
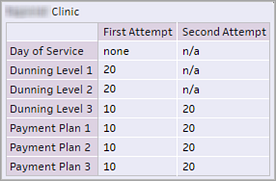
- To see the reminder schedule configured for each dunning level, click the View Reminders link in the Reminder Schedule column.
A pop-up box displays your reminder schedule for each dunning level. For Dunning Level 1 and Dunning Level 2, athenaOne sends only one Self-Pay reminder message, no earlier than 20 days after the first or second patient statement is sent.
To adjust these settings, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
To set the greeting for all athenaCommunicator messages, including Self-Pay reminder messages, use the Greetings page. Self-Pay reminder messages use the greeting configured at the practice level and, if your practice uses Communicator Brands, the greetings configured at the brand level.
Note: To see the phone messages sent by the Self-Pay reminder service, see "Example of a Self-Pay phone call" on the the Self-Pay Reminder Messages page.
- Display the Patient Communication Activity page: On the Main Menu, click Quality > Under REPORTS, click Patient Communication Activity.
- Criteria — Accept the default option: Past activity by communication date.
- Date range — Enter the date range for the report. You can also click the calendar icon
 and select the dates, or use the menu to select a time frame.
and select the dates, or use the menu to select a time frame. - Services — Select the SelfpayCall option. Deselect all other selected options.
- Message results — Click All to select all message results, or click Selected and then select the message result types to include in your report. You can select message types from these categories: Phone, SMS, Email, and ResultsCall.
- Departments — Click All to select all departments, or click Selected and then select the departments to include in the report.
- Providers — Click All to select all providers, or click Selected and then select the providers to include in the report.
- Report type — Select Summary to display a count of how many times each action was completed, or select Detailed to display a list of each action with the date and time.
- Report format — Select View as HTML page to display the report in athenaOne, or select Export CSV file to view the report in Excel.
- Click Run Report.
Note: To see the actual text or email message sent to a patient, locate the message in the Detailed report results and, in the View column, click the information icon ![]() . The text or email message sent to the patient is displayed. This can only be done when "View as HTML page" is used as the Report Format.
. The text or email message sent to the patient is displayed. This can only be done when "View as HTML page" is used as the Report Format.
Note: To see the phone messages sent by the Self-Pay reminder service, see "Example of a Self-Pay phone call."
Using the Patient Communication History report, you can display a specific patient's Self-Pay reminder messages.
- Display the patient Quickview.
- Display the Patient Communication History page: On the Patient Actions Bar, click Communicator, and then click Patient Communication History.
- Show services — Select SelfpayCall.
The summary results appear automatically. - To display detailed results about the Self-Pay reminder messages sent to this patient, click Detailed in the Report types field.
- To display the actual email or text message that the patient received:
- Locate the message that you want to view in the detailed report results.
- In the View column, click the information icon
 .
.
The email or text message sent to the patient is displayed. - When you're done viewing the message, click the X in the upper right corner.
Self-Pay reminders are available to all organizations that use the athenaCommunicator service at no additional fee. The Self-Pay reminder service automates the delivery of billing reminders to patients and guarantors via phone call, email, and text message. This service provides the following benefits:
- More revenue — It's easier for your practice to collect patient balances, increasing your yield on self-pay collections.
- Faster revenue — Automated payment reminders help your practice collect patient payments earlier in the revenue cycle.
- Less work — Patients receive payment reminders automatically, without practice intervention. If your practice is enrolled in Credit Card Plus, your patients can also make payments via the Patient Portal or over the phone with live operators.
- Less direct cost — Improved payment collection reduces potential collection agency expense.
To send Self-Pay reminder messages, your organization must use these athenahealth services:
To enable patients to pay their balance via the Online Statement-based Experience (formerly QuickPay Portal), the Patient Portal, or the Guest Payment service, and to allow live operators to accept patient payments over the phone, your practice must also have Credit Card Plus.
Note: For more information about the Live Operator service, see Automated Messaging Feature.
Self-Pay reminder messages work with patient statements as follows.
- Patients with an outstanding balance receive their first patient statement as usual: either as a paper statement via U.S. mail or as an electronic statement via the Patient Portal.
- If the patient balance is still outstanding 20 business days after the first statement date, the patient receives Self-Pay reminder messages.
- If the patient balance is still outstanding, the patient receives the second statement around Day 35, followed by Self-Pay reminder messages 20 business days after the second statement date.
- If the patient balance is still outstanding, the patient receives the third statement, followed by Self-Pay reminder messages 10 and 20 business days after the third statement date.
Note: If you want to change or delete the intervals after a statement is sent, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Dunning levels are used to evaluate the delinquency of a patient account. Patients progress through dunning levels if they have a patient charge or payment plan charge that is not closed (neither paid nor adjusted).
Note: Your practice can define the dunning messages that are printed on patient statements using the Dunning Messages page.
For Self-Pay reminder messages, athenahealth specifies three dunning levels for patients who do not have payment plans and three dunning levels for patients with payment plans. The default configuration for both types of dunning levels is as follows.
To adjust these settings, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Day of Service messages
Day of Service messages are disabled by default. When Day of Service messages are enabled, patients who do not pay their copay at the time of service receive a call or email the following day to remind them about the outstanding balance. If you would like to enable Day of Service Self-Pay messages, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Note: Day of Service phone calls cannot be transferred to live operators.
Dunning Level 1 and Dunning Level 2
For Dunning Level 1 and Dunning Level 2 (no payment plan), athenaOne sends only one Self-Pay reminder message, no earlier than 20 days after the first or second statement is sent.
Dunning Level 3 and Payment Plans 1 to 3
For Dunning Level 3, athenaOne sends Self-Pay reminder messages 10 days (first attempt) and 20 days (second attempt) after the third statement is sent. This schedule also applies to all statements for patients with payment plans.
By default, patients with outstanding balances of $9.99 or more receive Self-Pay reminders, unless your practice excludes them from the service or is holding their statements.
Note: You can ask the CSC to change the minimum outstanding balance amount, but that amount cannot be less than $9.99.
If your practice is enrolled in Credit Card Plus, Self-Pay reminders instruct patients to pay via their Patient Portal account or on the phone with live operators. If your practice is not enrolled in Credit Card Plus, Self-Pay reminders instruct patients to contact your office to make a payment.
These patients are automatically excluded from Self-Pay reminders:
- Patients with companies as guarantors.
- Minor patients with a designated guarantor on the Registration page (Self-Pay reminders for minor patients go to their designated guarantors).
- Patients who have Credit Card Plus card-on-file agreements with your practice. These patients have an agreement with your practice to charge their credit card when they have an outstanding balance.
- Patients who are signed up for the Credit Card Plus Bill on EOB feature.
Note: Patients on payment plans receive Self-Pay reminders only if they are behind on their payments (see the Reminder Schedule for payment plans at the top of the Self-Pay Reminder Messages page).
You can exclude patients from Self-Pay reminders as follows:
- Hold their statements. These patients will not receive Self-Pay reminders until you release their statements.
- On the patient's Privacy Information page, under Communicator Automated Messaging Preferences, deselect the Billing option. The patient will continue to receive statements but will not receive Self-Pay reminders.
- Exclude specific departments or providers from Self-Pay reminders. Patients with these departments or providers do not receive Self-Pay reminders. To enable this option, contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
By default, patients receive Self-Pay reminders via phone call, email message, and text message. Self-Pay reminder messages also appear on the Patient Portal. Self-Pay reminder phone and text messages are sent from 10:00 a.m. to 8:00 p.m. Patient Portal messages are sent early in the morning, typically before 6:00 a.m. Self-Pay reminder emails are sent between 8:00 a.m. and 9:00 p.m.
Note: If your practice uses the Live Operator service, the message window for phone calls must be within the calling window available for this service — that is, 10:00 a.m. to 8:00 p.m. local time, Monday through Friday (excluding major holidays). For more information about the Live Operator service, see Automated Messaging Feature.
You can review your calling window information at the top of the Self-Pay Reminder Messages page. To change the message types or the times that the messages are sent to patients, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
athenaCommunicator services do not place phone calls of any kind on the following holidays. Calls scheduled for these holidays go out one calling day earlier, based on the practice settings for calling days:
- New Year's Day
- Memorial Day
- Independence Day (July 4th)
- Labor Day
- Thanksgiving Day
- Christmas Eve
- Christmas Day
- New Year's Eve
For ReminderCall, GroupCall, ResultsCall, and Self-Pay reminders, the calling system adds a day to the calling window for the day before a holiday.
Email and text messages
For the holidays listed above, athenaCommunicator services send email and SMS text messages except for these GroupCall campaigns:
- Immediate Cancellation
- Weather
- Same-day custom campaigns
If messages for these campaigns are configured to be sent on the holiday (or after the message window closes on the day before the holiday), email and text messages are not sent until the next (non-holiday) business day.
Note: For more information about message windows, see Message Windows for athenaCommunicator Automated Messages.
Self-Pay Reminders and Bank Holidays:
For Self-Pay reminders, athenaCommunicator observes bank holidays, and on the following days, we do not send any Self-Pay reminders (calls, emails, or text messages):
-
Martin Luther King Day
-
President's Day
-
Juneteenth
-
Columbus Day (Indigenous People's Day)
-
Veteran's Day
Messages scheduled for bank holidays go out one day earlier, based on the practice settings for message days.
If your practice uses provider groups, you can transfer Self-Pay reminder calls to live operators by provider group (instead of by practice) if the provider group has Credit Card Plus. With Credit Card Plus, the live operator can accept a payment over the phone.
To take advantage of transfers to live operators, the practice or provider group must use Credit Card Plus and have a transfer number set up so that live operators can take payments when a call is redirected. To enable transfers to live operators for Self-Pay reminder calls, please contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
For the most up-to-date versions of Self-Pay messages, visit this link on the Success Community.
In the following examples, text in brackets (for example, [PATIENTNAME]) indicates a variable that is replaced with your information. For example [GREETING] is replaced by the greeting that you configured on the Greetings page.
[GREETING]. The following is an important message for [PATIENTNAME]. You have received a message from [PRACTICENAME] regarding your recent bill. Please view this message by accessing your patient portal account on our website at [PRACTICEURL]. If you have not yet registered for our online patient portal, please visit our website to register.
Note: The caller ID that patients see when they receive a Self-Pay reminder call is the phone number configured for the practice or brand (if you use Communicator brands) on the Patient Communication Content Management page. If a different billing phone number is configured on the Patient Communication Content Management page, that number is the caller ID number for Self-Pay reminder calls.
To edit this page, you must have one of these permissions:
- Communicator Admin
- Communicator Admin: Greetings
- Click the Settings icon
 . Under ADMIN, click Communicator. In the Task Bar, under PRACTICE LINKS — Greetings and Instructional Messages, click Greetings.
. Under ADMIN, click Communicator. In the Task Bar, under PRACTICE LINKS — Greetings and Instructional Messages, click Greetings. - Click the provider, department, or brand on the left side of the page, or filter by department or provider.
- Select the Use custom greeting radio button.
- Click Update.
Note: If you are creating a custom greeting for the first time, click Create . The Editing Greetings menu appears. Select Text-to-speech, if it is not already selected. - Scroll down to Spanish Greeting and check Enable Spanish if it isn't already selected.
- For a provider greeting, you must select Provider name. You can also select Department name, Department address, or both.
- For a department greeting, you must select Department name. You can also select Department address.
- Click Listen to play the complete TTS greeting. (You must listen to the greeting before you can activate it.)
- Click Save.
Notes:
- Spanish greetings must be checked on the Self-Pay Settings page. You can do so by clicking the Settings icon
 . Under ADMIN, click Communicator. In the Task Bar, under PRACTICE LINKS — Self-Pay, click Self-Pay Settings.
. Under ADMIN, click Communicator. In the Task Bar, under PRACTICE LINKS — Self-Pay, click Self-Pay Settings. - The Language field on the Quickview does not have any effect on ReminderCall phone calls.
- During the Self-Pay call, the option to press 8 will be spoken in Spanish.
Subject: Please view your statement and make a payment today.
[PATIENTNAME], you have a payment due
Your health insurance provider has paid their part of the cost for your medical care from [PRACTICENAME] and the balance is your responsibility.
VIEW STATEMENT
Which part of these costs are my responsibility?
If you have insurance, you may be responsible for copays, deductibles, and coinsurance related to your care--how much is determined by your unique policy.
If you don't have insurance, you are responsible for any costs related to your care.
But, I already made a payment.
It may take time for the payment to process and reflect in your account. If you paid in full, no further action is needed.
If you have questions about your bill, please contact us directly, or read the FAQs. For more information about your unique insurance coverage, contact your insurance provider.
Subject: Por favor, ve tu estado de cuenta y haz un pago hoy
[PATIENTNAME], tienes un pago pendiente
Tu proveedor de seguro medico pago su parte del costo de tu atencion medica de [PRACTICENAME] y el saldo restante es tu responsabilidad.
REVISAR ESTADO DE CUENTA
Que parte de estos costos son mi responsabilidad?
Si tienes seguro, es posible que seas responsable de los copagos, deducibles y conseguros relacionados con tu atencion; la cantidad depende de la poliza especifica de tu seguro.
Si no tienes seguro, eres responsable de los copagos, deducibles, y conseguros relacionados con tu atencion.
Pero, ya hice un pago.
Es posible que nos lleve tiempo procesar tu pago y reflejarlo en tu cuenta. Si ya hiciste el pago completo, gracias, no tienes que hacer nada mas.
Si tienes preguntas sobre tu factura, contactanos directamente o lee las Preguntas Frecuentes. Para obtener mas informacion sobre to cobertura especifica, contacta con tu proveedor de seguro.
Your bill is ready to view and pay. Visit [SMSPRACTICENAME] portal at [SMSPRACTICEURL] for details. Reply STOP to opt out.
Tu factura con [SMSPRACTICENAME] esta lista. Revisa aqui: [SMSPRACTICEURL]. Responde STOP para rechazar.
[FIRSTNAME],
We appreciate your business and the opportunity to be your partner in health.
Thank you for your recent visit. [PRACTICENAME] is pleased to offer you an easier, faster, and secure way to view and pay your bill online.
Please [PAYNOWLINK] to make your secure payments via credit or debit card. You may also visit the Billing section found on this portal to review specific charges and any explanation of benefits provided to us by your insurance carrier.
If you feel like this notice is inaccurate, please reply to us with a message. Thank you again for your business and for your prompt attention to this matter.
[FIRSTNAME],
We appreciate your business and the opportunity to be your partner in health.
Our records indicate that you have a current balance of [SELFPAYBALANCE] and per the terms of our financial arrangement a payment toward this balance is now due. This balance represents co-payments and or charges that you are responsible for not covered by your insurance carrier.
Please [PAYNOWLINK] to make your secure payment via credit or debit card. You may also visit the Billing section found on this portal to review specific charges and any explanation of benefits provided to us by your insurance carrier.
If you feel like this notice is inaccurate please reply to us with a message. Thank you again for your business and for your attention to this matter.
| Column Headings | |
|---|---|
| Provider Group | If your practice uses provider groups, this column displays the provider group to which the Self-Pay messages apply. |
| Departments |
Departments to which the Self-Pay messages apply. |
| Providers |
Providers to which the Self-Pay messages apply. |
| Minimum Balance |
Minimum patient balance required to generate the Self-Pay messages. The minimum patient balance for Self-Pay reminder messages is $9.99; this balance is the default value. |
| Message Type | Self-Pay reminders can be sent as one or more of the following message types: phone calls, email messages, text messages, or Patient Portal secure messages. |
| Call Times | Days and times when Self-Pay reminder messages are sent. |
| Transfers | This column shows whether call transfers to live operators or to your practice are enabled. |
| Reminder Schedule |
Click the View Reminders link to see the reminder schedule configured for each patient statement dunning level. |
| Phone Calls | |
| Patient Message | Script of the message that the patient receives via phone call. |
| Guarantor Message | Script of the message that the guarantor receives via phone call on behalf of the patient when the patient has a guarantor on the Patient Registration page. |
| Emails | |
| Patient Message |
Script of the message that the patient receives via their regular email account. |
| Guarantor Message | Script of the message that the guarantor receives via their regular email account on behalf of the patient when the patient has a guarantor on the patient Registration page. |
| Text Messages | |
| All Messages | Script of the message that the patient or guarantor receives via SMS text message. |
| Patient Portal Messages | |
| Day of Service Message |
Script of the message that the patient receives on the day of service via secure email on the Patient Portal. |
| Dunning Levels 1-3 Message | Script of the message that the patient receives for Dunning Levels 1 through 3 via secure email on the Patient Portal. |
| Dunning Levels 5-7 Message | Script of the message that the patient receives for Dunning Levels 5 through 7 via secure email on the Patient Portal. |