 User Guide — Billing Overview
User Guide — Billing Overview
The billing workflow starts with charge entry — that is, entering the charges into athenaOne from the billing slip and creating the claim. The billing slip can be an encounter form or a super-bill.
You can accomplish charge entry as follows:
- During the Checkout stage of the 5-stage patient encounter (preferred method)
- In batch mode
- From the Quickview
In general, athenahealth recommends that you enter charges during the Checkout stage of the 5-stage patient encounter using the Claim: Charge Entry tab. Ideally, you should enter charges while the patient is still in the office, in case you have a question that can be quickly resolved by asking the patient.
But if this process does not suit your practice, you can also accomplish charge entry by collecting the day's billing slips and entering charges for all the appointments at the end of the day or shift. This is known as charge entry in batch mode.
Refer to Charge Entry — Batch Mode for more information.
After charge entry is accomplished, the claim is instantly checked by the athenaOne Rules Engine for errors. After the claim is "scrubbed" by the Rules Engine, it is assigned a claim status.
When you click Create Claim on the Charge Entry tab, athenaOne displays the Claim Preview page, where you can check the new claim's status. If the claim is not in DROP status, read the notes in the Claim Notes section at the bottom of the Claim Preview page and follow the instructions to correct the claim. If you cannot move the claim to DROP status using the Claim Notes section of the Claim Preview page, you can click the Go to Claim link to display the Claim Action page. On the Claim Action page, make the needed corrections and save the claim.
What happens when you correct a claim?
When you correct a claim error, the athenaOne Rules Engine automatically rescrubs the claim, then updates the claim status to reflect the correction. If there are no errors (a "clean scrub"), athenaOne automatically assigns DROP status to the claim. But suppose a claim has two errors:
- The claim has an expired policy, a scrub error that normally places a claim in HOLD.
- The claim's department is missing a place of service type, a scrub error that normally places a claim in MGRHOLD.
If you correct the second error, then save the claim, athenaOne immediately assigns the claim to HOLD status because the first error is still valid. If possible, you should continue to edit and save the updated claim until the claim is assigned DROP status.
Make every effort to achieve DROP status for the claim: you may have to edit the claim more than once, because a claim may contain multiple errors. To learn about claim status, refer to the Claim Status page; for help with kick reasons, see the View Kick Reasons page.
When a claim contains errors or has been denied by the payer, athenaOne provides several avenues for billing follow-up (for more information, see Billing Follow-Up).
Billing follow-up includes reading claim notes and taking the appropriate corrective action. The Claim Notes section provides you with guidance for correcting claim errors. Claim notes track follow-up actions performed for each claim. Active claim errors appear in red. The Claim Notes section appears on the Claim Action page, the Claim Edit page, and the View Claim History page.
Using View Claims Worklists for claim follow-up
You can use the View Claims Worklist page to view worklists of claims sorted by various categories, so you can systematically work down the list to correct the claims. You can display the View Claims Worklist and click any of the category links (By Outstanding Amount, By Payer, By Reason, etc.) to display a list of claims in that category.
When you click on any linked claim, the Claim Action page for that claim appears in the Workspace. On this page, you can review the Claim Notes section to determine the corrective action and make the necessary changes.
Each claim appears only once in the list, under a single kick reason — even if the claim has more than one active kick code. The kick reason reflects the current status of the claim. This single listing for each claim reveals the actual cause of the claim's current status and allows a billing manager to evaluate trends and to facilitate routing of work among the staff members responsible for different types of claim issues. A billing manager can use the worklists to assign various error reasons to different staff members without assigning redundant work.
See View Claims Worklist for more information about this worklist.
Payers process claims in a standard amount of time and reject claims that are filed beyond their specified deadlines. athenaOne uses two "claim alarm" statuses to ensure that no claim expires before it is paid.
ATHENADROP — athenaOne automatically assigns this status to any unsubmitted claim 15 days before the payer's filing deadline, regardless of the claim's current status. After the claim is submitted, the claim reverts to its previous status. This status is not available for athenaCollector (No Posting) clients.
Note: To comply with Minnesota Statute § 62J.536, athenahealth will not force the electronic submission of Minnesota-based paper claims approaching timely filing limits.
FOLLOWUP — athenaOne automatically assigns this status to any billed (submitted) claim that had no action from the payer within a designated, payer-specific period of time. athenaCollector (No Posting) and athenaCollector (No Follow-Up) clients are responsible for claims in FOLLOWUP status.
athenahealth reviews all athenaCollector claims in FOLLOWUP status, and takes appropriate action. This usually means that athenahealth contacts the payer by telephone to determine the cause of the delay and to take any action necessary to ensure a remittance (e.g., a payment or a denial) from the payer. See also: Claim Alarms.
(This service is not performed for "No Posting" and "No Follow-Up" clients.)
Billing follow-up also includes monitoring the progress of all BILLED claims, taking follow-up action based on established payer-specific waiting periods, and writing claim notes regarding claim status as claim issues are identified and addressed. athenahealth performs follow-up for athenaCollector clients' claims in BILLED status. athenaCollector (No Posting) and athenaCollector (No Follow-Up) clients are responsible for their own BILLED claims follow-up.
Refer to Billing Follow-Up to learn about billing, claim status, and co-sourcing responsibilities.
athenahealth reviews certain types of claim denials and resolves the denials when possible. If athenahealth is unable to resolve and resubmit the denied claim, or if the denied codes are not expected to be paid if resubmitted, we return the claim to you with claim note advice.
If your organization uses both athenaCollector and athenaClinicals, athenahealth reviews coding-related back-end denials for claims that have been denied with the following codes.
- AGECPTMATCH
- AGEDXMATCH
- CPT
- CPTCHANGE
- DIAGNOSIS
- DXCPTMATCH
- GENDERCPTMATCH
- GENDERDXMATCH
- MODCPTMATCH
- MODIFIER
- POS
- POSCPTMATCH
If a claim has one of these coding denials and has clinical documentation in the patient chart, athenahealth assigns the claim to CBOHOLD status. After we review the claim, we mark it with one of the following tags:
- **CODING ADVICE** — If a claim needs a coding correction, we add claim note advice and return the claim to you. After you make the necessary changes and apply the DRPBILLING kick code, athenahealth resubmits the claim.
- **ADVICE TO ADJUST** — If a claim is unlikely to be paid due to payer billing requirements, we may add advice for adjustment and return the claim to you.
- **DOCUMENTATION REQUEST** — If a claim has insufficient clinical documentation to support billing, we return the claim to you with a claim note. After you add or update the clinical documentation, we will review it.
If we find that the payer erroneously denied a claim, athenahealth resubmits the claim after reviewing the billing and supporting clinical documentation.
If your organization uses both athenaCollector and athenaClinicals, athenahealth reviews denials related to medical policies and insurance benefits for claims that have been denied with the following codes:
- MEDPOLICY — athenahealth reviews the claim and available medical records to verify insurance package selection.
- NCPREVIEW — athenahealth reviews the claim and available medical records to verify insurance package selection.
- MP — athenahealth reviews the claim and available medical records to verify insurance coverage.
- SERVICEMAX — athenahealth reviews the claim and available medical records to verify insurance coverage.
- NMN — athenahealth reviews the claim and available medical records to verify medical necessity.
When athenahealth reviews these denials, we assign the claim to CBOHOLD status and attempt to resolve and resubmit the claims to the payer. If we are unable to resolve the issue and resubmit the claim, or if the denied codes are not expected to be paid if resubmitted, we return the claim to you with clear coding or adjustment advice or we request additional medical records.
Note: athenahealth is assuming this work gradually, through 2019. When this feature becomes available to your organization, you will receive an athenaNetwork posting.
athenahealth reviews denials with an IPN or NEREVIEW kick code for claims with or without an insurance card on file in athenaOne. These denials indicate that the patient's insurance information is incorrect (IPN kick code) or that the patient's eligibility is in doubt (NEREVIEW kick code).
If a claim has one of these patient insurance denials with no associated insurance card image, we assign the claim to CBOHOLD status and attempt to resolve and resubmit the claim to the payer.
Note: For information about other insurance-related denials, see Eligibility-related denials.
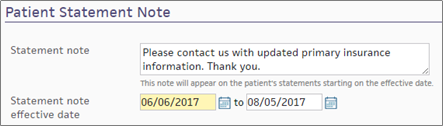
If athenahealth is unable to resolve the issue and resubmit the claim, we send a statement to the patient with a note asking the patient to contact you to provide updated insurance information. (This note appears in the Patient Statement Note section of the Patient Account View page.)
If athenahealth cannot resolve the patient insurance issue and the patient cannot be billed, the claim may be returned to you for review.
Note: athenahealth is assuming this work gradually, through 2019. When this feature becomes available to your organization, you will receive an athenaNetwork posting.
athenahealth automatically reviews claims that have been denied with the following codes:
- INDICATOR — athenahealth makes claim formatting corrections.
- NDCNUMB — athenahealth corrects the National Drug Code (NDC) number based on claim coding and medical records.
- PRACCHGRVW — athenahealth corrects posting issues.
When athenahealth reviews these denials, we assign the claim to CBOHOLD status and attempt to resolve and resubmit the claims to the payer. If we are unable to resolve the issue and resubmit the claim, we return the claim to you with clear instructions for next steps based on our research.
Note: athenahealth is assuming this work gradually, through 2019. When this feature becomes available to your organization, you will receive an athenaNetwork posting.
Beginning in April 2025, we're automating some low dollar amount athenahealth denials management tasks for charges that are unlikely to be paid.
Benefits:
- Automated tasks for faster turnaround time
-
Improved claim note format that is easier to read
- Reduced volume of claims that need resubmission
-
Focused coder intervention only where coding corrections are actually needed
- Reduced manual work for practice staff and athenahealth Denials Management team
Note: This automation only applies to CBOHOLD denials that are reviewed by the athenahealth Denials Management team.
What's automated?
- The athenahealth AI technology reviews the claim.
-
Using advanced machine learning techniques and continuous data analysis, the model identifies charges that are highly unlikely to be paid upon resubmission (based on historical payment trends and payer guidelines).
-
The athenahealth AI technology adds a claim note with details specific to the denied charges.
Will the AI-generated claim notes look different?
-
The claim note added by the athenahealth AI technology will look very similar to the claim note that is manually added by the athenahealth Denials Management team.
-
Both the manually added note and the automatically added note will have:
-
Specific details about the denied charges
-
Action: NOTE
-
Claim Status: MGRHOLD
-
- The User on the claim note will be different:
Manually added claim notes have User: <athenaOne username>
AI-generated claim notes will have User: AI Insight
| athenaOne release date | Type of Denials | Automated claim note/ kick code |
|---|---|---|
| April 2025 | Coding, Medical policy, and Benefit coverage denials |
"Advice to Adjust" / [ADJUST] kick code |
| June 2025 | Unspecified denials – When the payer has not provided a denial code, or when the payer has provided a denial code that does not indicate any helpful or guiding information. The denial requires additional research or payer contact. |
"Advice to Adjust" / [ADJUST] kick code |
| June 2025 | Coding denials that might be resolved with coding-related changes |
"CODING ADVICE" / coding-related kick code |
| October 2025 |
Coding denials with no coding changes needed
|
"Advice to Adjust" / [ADJUST] kick code |
Your practice can continue to use your existing workflow for handling claims on MGRHOLD with "Advice to Adjust" or "CODING ADVICE".
We plan to expand to other types of denials in upcoming releases. The updates will be communicated to you in future release notes.
For athenaCollector and athenaCollector (No Follow-Up) clients, athenahealth posts all payments received for your practice.
For athenaCollector (No Posting) clients, the billing workflow includes payment posting. You can use the Post Payment page to accomplish this.
athenahealth recommends that your practice use the Daily Batch Header Appts page on a daily basis to:
- Process any appointments that have not been checked in, checked out, or had charges entered
- Ensure that all pending claims achieve DROP status
The page displays the new patients registered during the day (if any), followed by the day's appointments (in billing slip order), with patient name, phone number, and the current appointment or claim status.
- Display the Daily Batch Header Appts page: On the Main Menu, click Calendar. Under APPOINTMENTS, click Batch Header Appointments
- Scan the list of patient appointments. For every appointment that is not in DROP, CLOSED, or CANCELLED status:
- Click on the patient name. The appropriate page appears (Appointment, Check-in, Checkout, Charge Entry, or Quickview).
- Take any actions needed to produce a claim in DROP status.
- You can click the Batch header appts link at the top of the Today's Appointments worklist to refresh the list.
Completing the appointment batch header means that all patient encounters are accounted for at the end of each day. Any unfinished tasks appear on the Workflow Dashboard the following day.
athenahealth recommends that practice managers ensure that the Workflow Dashboard Missing column contains 0 at the end of each day. athenahealth has learned from statistical analysis that for every day a claim goes unentered (and so not submitted to a payer), it loses an average of 0.6 percent of its value. Therefore, charge entry should be completed within 24 hours of service for office visits and within 2 to 3 days for surgical and hospital-based claims.
When you click any linked dollar amount on the Workflow Dashboard, the corresponding list of claims appears in the Task Bar. You can then click the claims in the list to access the Claim Action page and perform the necessary follow-up actions.
Ideally, the Hold, Mgr Hold, and Missing Slips columns in the Workflow Dashboard for all departments in your practice should contain $0 at the end of each day. For athenaCollector (No Posting) clients, the CBO Hold column should also contain $0. Using the Workflow Dashboard in this way can help billing managers attain and maintain a low DAR for their practice.