Claim: Charge Entry Tab — Basic
athenaOne for Hospitals & Health Systems
This tab allows you to enter charges and create a claim for services provided to a patient during an appointment.
|
The charge entry tab described on this page is being replaced by an enhanced charge entry tab. See the O-help page about the redesigned charge entry tab. Note: The classic Charge Entry tab is still available for ambulatory departments of organizations that use athenaOne for Hospitals, as well as for anesthesia claims created using time sheets (see Anesthesia Billing Using Time Sheets). You can click the Classic Charge Entry link to open the classic Charge Entry tab. |
Note: If the appointment has not yet been checked out, creating a claim automatically completes checkout and moves the appointment to status 4.
- athenaClinicals: From the Claim: Billing tab, click Save & Enter Charges to display the Claim: Charge Entry tab.
athenaCollector: From the Checkout stage, click the Claim: Charge Entry tab.
Patient and provider fields
- Note that the billing slip number, date of service, and the insurance policy used for this claim appear at the top of the page. Note that the Post date is set to the current date, and the patient's name and date of birth appear in bold green type.
- Scheduling provider — Verify or select the scheduling provider. This provider was originally scheduled for this appointment.
- Rendering
provider — Verify or select the rendering provider.
This provider actually provided the services during the appointment.
Note: This provider typically does not appear on the claim form. - Supervising
provider — Verify or select the supervising provider.
Note: This provider typically appears as the rendering provider on the claim form. - If the selected rendering provider does not require a supervising provider, the supervising provider field is auto-populated.
- If the selected rendering provider requires a supervisor and if the rendering provider has a "usual supervising provider" defined in athenaOne, you can click the linked provider username that appears to the right of the Rendering provider field, or you can ignore the hint and select an alternative. (You can update a provider type and usual supervising provider using the Providers page.)
- Patient department — Verify or select the patient department. The default is the patient's primary department (from the Quickview page).
- Service department — Verify or select the service department.
- Current illness date — If applicable, enter or select the date of onset of the current illness.
- If applicable, click Choose/view to access the Referring Provider Lookup, then select the referring provider.
- Authorization — If applicable, you can select the authorization number from the list.
- Or manually enter auth # — If the authorization number does not appear in the Authorization menu, you can enter it in this field.
Note: You can enter additional information about a new authorization on the Quickview.
Service Type add-on fields
- Click the down arrow to the left of the service type add-on. The additional claim fields appear.
- Abortion — Check if the claim relates to abortion where the mother's life was endangered.
- Anesthesia — Check if the claim is for anesthesia services and you do not use anesthesia time sheets to create anesthesia claims.
- Breast Care —
- Consultation — Check if the claim is for a "second opinion" consultation.
- Corporate Billing — Check if your practice uses corporate billing for this payer.
- COVID-19 — Check if the claim is for services related to COVID-19 care. The COVID-19 service type add-on appears on claims created with or without an appointment.
- Diagnostic Services — Check if the claim includes diagnostic testing you have purchased from an outside vendor.
- Dialysis — Check if the claim is for Epoetin (EPO) therapy for a patient on dialysis.
- DME — Check if this claim is for durable medical equipment.
- Drug/Injectables — Check if the claim's payer requires patient weight in conjunction with drug or vaccine administration.
- Foreign System Identifier —
- Hearing/Vision — Check if the claim is for hearing aids or vision lenses.
- Hospice — Check if the claim is for palliative care or for supportive care for a terminally ill patient in the home.
- Immunization — Check if your state requires the serum batch number on a claim for immunizations.
- Maternity — Check if your state law requires you to report the determination of pregnancy, and for claims that require EDD and LMP.
- Miscellaneous Fields — Check if the claim requires service authorization exception codes.
- NDC — Check if the claim includes charges for J drug codes.
- Newborn Care — Check if the claim requires newborn patient's weight.
- Paperwork — Check to charge for additional paperwork.
- PT/OT — Check if the claim is for occupational, speech, or physical therapist services.
- Ordering Provider — Check if the claim is for services ordered by another provider, and the payer requires you to report the ordering provider.
- Podiatry — Check if the claim is for services related to routine foot care.
- Post-Operative Care — Check for a claim that covers surgical patient care that is shared between two providers (the surgeon and the post-operative care provider).
- Reference Lab —
- Rehabilitation Services — Check if the claim is for in an accredited rehabilitation facility and the ordering provider is required by the claim's payer.
- Spinal Manipulation —
- Telehealth — Check if the claim is for a telehealth appointment. The Telehealth service type add-on appears only when the claim is created without an appointment. If an appointment is associated with the claim, the appointment should have the Telehealth Distant Site Visit appointment type class applied (see To add Telehealth Distant Site Visit to your available appointment types).
- Well Child Care — Check if the claim is for services provided to children as part of a Child Preventative Medicine Program (e.g., EPSDT, Health Check).
- Enter the appropriate data in the additional fields.
Procedure and diagnosis codes
- Procedures column — Enter the first procedure code.
- If you enter an unknown procedure code, a note appears just above the Create Claim button; check the code for accuracy, then re-enter it.
- If you are not sure of the code, enter a period to activate the Procedure Lookup tool.
- As an alternative, you can use the athenaCodesource Code and Knowledge Base tool to locate or verify the procedure code.
- Diagnoses column — Enter the primary diagnosis code. You can also enter a secondary diagnosis code in the box to the right. (Enter only one code per text box.)
- If you enter an incomplete or unknown diagnosis code, a note appears just above the Create Claim button; check the code for accuracy, then re-enter it.
- If you are not sure of the code, enter a period to activate the Diagnosis Lookup tool. (If you have entries in the "My Diagnoses" list, they appear at the top of the Diagnosis Lookup tool.)
- As an alternative, you can activate the athenaCodesource Code and Knowledge Base tool to locate or verify the diagnosis code.
- Repeat steps 14 and 15 if you need to enter additional procedure and diagnosis codes.
- Enter procedure codes that share the same diagnosis codes, horizontally along the same row.
- Enter procedure codes that do not share the same diagnosis codes in the next row.
- You should click
Validate Codes to check the validity
of procedure and diagnosis code combinations. When
you click
Validate Codes,
all the diagnosis and procedure codes on the claim are automatically passed into the "Part B" form.
Note: The appropriate state and CCI version corresponding to the date of service are also selected automatically. - Click Create
Claim to submit the claim.
The Claim Review page appears, showing you the status of the claim, and summary information.
Entering more than 12 diagnosis codes on a claim
You can enter up to four diagnosis codes per procedure code and up to 12 diagnosis codes per claim. If you enter more than 12 diagnosis codes associated with the procedures billed on the claim, athenaOne automatically generates an additional claim to accommodate the additional codes after you click Create Claim (this is called "splitting" the claim).
However, if the total number of diagnosis codes exceeds 12 and the additional diagnosis codes are not associated with a procedure, athenaOne does not send all the codes entered in this section on the claim. After you click Create Claim, athenaOne creates a new claim note to indicate which codes it was not able to add to the claim and moves these diagnosis codes to the Internal Use - Other Diagnoses section, so that you can review them on the Claim Edit page.
If you enter more than six procedure codes and the claim is generated on paper, athenaOne also splits the claim and generates an additional claim (or claims) to accommodate the charges (paper forms do not allow more than six procedure codes). See Paper Claims to learn more about diagnosis pointers and paper claims.
athenaOne supports claim splitting for claims with more than 12 diagnosis codes when the reporting charges are $0.
You can enter up to 12 diagnosis codes per claim. If the total number of diagnosis codes exceeds 12, athenaOne automatically generates additional claims to accommodate the excess diagnoses which are not associated with a procedure billed on the claim, and links the diagnoses to placeholder procedure code 99499.
The increased claim limit helps you better report all related diagnosis codes when submitting claims for value-based care programs.
After you click Create Claim, athenaOne automatically splits the claim and you can see a note automatically appear on Claim Edit.
When this feature creates a claim with related claims, the athenaOne system holds all claims together (and releases them together as well).
Ask athenahealth to enable the Automatically Split Claims with Excess Diagnoses Codes setting. Contact the CSC or your onboarding project team. On the Main Menu, click Support > Success Community > Contact Client Support Center.
To have the reporting charges as $0 on the claim, 99499 should be added to your fee schedule with a value of $0.00. If you use a value greater than $0.00 and less than $1.00, splitting will still happen but the charge will not be set to $0.00. For more information about Fee Schedules, see Fee Schedules in O-help.
Important: If the placeholder procedure code 99499 is in your fee schedule with a cost value of $1.00 or greater, or if you set the value to $0.00 but do not set Primary Print Zero Dollar Charges to YES:
-
You’ll see an error when the athenaOne system tries to automatically split a claim.
-
The claim will be created with a claim note explaining that overflow diagnoses were dropped.
- athenaClinicals: From the Claim: Billing tab, click Save & Enter Charges to display the Claim: Charge Entry tab.
athenaCollector: From the Checkout stage, click the Claim: Charge Entry tab. - Select the reason that the appointment should not result in a claim from the Reason menu located at the bottom of the page.
- Click Mark
Appointments As Not Requiring Charge Entry. (This option appears only for
claims generated as a result of an appointment.)
The appointment is removed from the MISSING list and moves directly to status 4. The appointment checkbox is disabled and unavailable for subsequent marking.
Note: All appointments that the patient has scheduled for this day also appear listed at the bottom of the page, with checkboxes. The current appointment appears in bold.
If charge entry is accomplished at checkout time
If the patient has more than one appointment scheduled for the same day, or if this is a multi-resource appointment, you should follow the parent appointment (the one scheduled for the billable provider) all the way through to the Charge Entry page to ensure that the correct billable provider information is copied into the claim. Then you can enter all the charges on the parent appointment, and mark the other appointments as not requiring charge entry.
If charge entry is accomplished in batch mode
You can still mark other appointments as not requiring charge entry by selecting the appropriate appointments and then clicking Mark Appointments As Not Requiring Charge Entry.
The Claim Validation feature helps you validate charge entry data before claims get created. See Validate Charge Entry Data Before Claim Creation with Claim Assistant to learn more.
The Claim: Charge Entry tab has two views (this is the basic view).
For most claims, you can use the Basic view. But you must use the Advanced view if:
- You need to enter more than four rows of procedure codes.
- You need to create a claim that requires additional information (for example, claims for services related to employment, an auto accident, an accident where a third party is responsible, hospitalization, or a test/specimen number).
- You need to use corporate billing.
athenaOne automatically checks the claim date of service against the earliest date of service for your practice. A warning message appears if you enter a claim that has charges with dates of service prior to the earliest date of service on file. The earliest date of service is recorded in the Earliest Date Of Service practice setting.
If the claim includes purchased service components, use modifier 90 to indicate purchased services.
For self-pay patients, you can use the Check Fee Schedule page as a quick reference tool to look up fees for procedure codes.
On the Claim Edit and Charge Entry pages, you can type an equal sign (=) or the letter "s" in any diagnosis or procedure code field to copy the codes from the previous line.
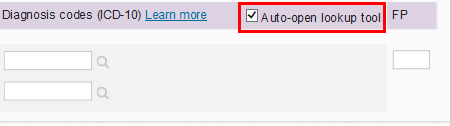
On the Charge Entry page, you can prevent the diagnosis code lookup tool from automatically opening. In the Charges area, clear the Auto-open lookup tool checkbox. The diagnosis code lookup tool is still available by clicking the magnifying glass or by typing "." or "?" in the field.
| UB-92
form (appears only if the UB‑92 custom form feature is enabled) |
|
|---|---|
| Internal Control Number |
The internal control number (ICN) or document control number (DCN) assigned to the original bill by the primary payer. Corresponds to FL 37 of the UB-92 claim form. |
| Frequency Of Bill |
The value selected populates the 3rd digit of the Type of Bill code reported in FL 4 of the UB-92 claim and/or its electronic equivalent in the 837I. The third digit represents the sequence of the bill for a specific episode of care. Note: The first 2 digits of the Type of Bill field are derived from the Department assigned to the claim. You can administer the first 2 digits using the Type of Bill drop-down selection on the Departments page. The two digits represent the type of facility and the type of care being billed (bill classification). |
| Admission Source |
The source of the admission or outpatient services. Corresponds to FL 20 of the UB-92 claim form. This field is used to identify the source or origin of the admission (for example, was the admission the result of a physician referral, transfer from an SNF, etc.?) The code selected in this field of information is reported in FL 20 of the UB-92 or Loop ID 2300, CL102 of the 837I. |
| Admission Type |
Indicates the priority of a patient admission. Admission type information is reported in FL 19 Type of Admission/Visit of the UB-92 or its electronic equivalent. |
| Admission Hour |
Indicate the admission hour of a patient encounter form the UB-92 charge entry form. Information recorded in the Admission Hour field is reported in FL 18 of the UB-92 or its electronic equivalent. |
| Discharge Hour |
Indicate the discharge hour of a patient encounter from the UB‑92 charge entry form. Information recorded in the Discharge Hour field is reported in FL 21 of the UB‑92 or its electronic equivalent. |
| Patient Status |
The patients disposition as of the ending date of service for the period of care reported. Corresponds to FL 22 of the UB-92 claim form. |
| Attending Provider |
For outpatient claims, the provider who requested the surgery, therapy, diagnostic tests, or other services. If unspecified, will be set to the rendering provider on the claim. Corresponds to FL 82 of the UB-92 claim form. |
| Condition Codes |
Codes identifying conditions that may affect payer processing of this claim. These codes help determine patient eligibility and benefits and are used to administer primary and secondary insurance coverage. Corresponds to FL 24-30 of the UB-92 claim form. |
| Occurrence Codes/Dates |
Codes and associated dates defining a specific event related to this bill that may affect payer processing. These codes are used to determine liability, coordinate benefits and administer benefit programs. Corresponds to FL 32-35 of the UB-92 claim form. |
| Occurrence Span Codes/From/To |
Codes and associated date ranges identifying an event that relates to payment of this claim. These codes identify an event that occurs over a span of time. Corresponds to FL 36 of the UB-92 claim form. |
| Value Codes/Amounts |
Codes identifying monetary data required for processing claims. The information is required for benefit determination and provides reporting capability for data elements that are used routinely but not available in a specific FL. Corresponds to FL 39-41 of the UB-92 claim form. |
| Charge Entry Batch Fields (Appear only if charge entry batch is open) |
|
|---|---|
| CURRENT CLAIM BATCH# |
The system-assigned charge entry batch number. |
| # claims target |
The target number of claims for the charge entry batch. |
| # claims entered |
The number of claims created in the charge entry batch. |
| charge amount |
The total amount of charges entered in the charge entry batch so far. |
| Service | |
| Service date |
The date of service for the claim. The Date of service field must be populated before you can enter procedure and diagnosis information on the Charge Entry page. Note: If you arrive at the Charge Entry page through the appointment workflow, this field is pre-populated based on the appointment date. |
| Patient department |
The patient's current department of care, usually the department where the patient's chart resides. The default value is the patient's primary department as shown on the Quickview. This field is sometimes used to determine the contents of the 33A (PIN) (currently used only for Medi-Cal). |
| Service department |
The department where the service was performed. |
| Insurance | |
| Primary payer |
Determines which policy this claim should be billed under. By default, the patient's current primary policy is displayed. Note: Deactivated payment plans do not appear in this menu unless the charge is currently assigned to that plan. You cannot assign the primary charge to a cancelled plan using this page.
For anesthesia claims generated from time sheets:
|
| Secondary payer |
Determines which secondary policy this claim should be billed under. By default, the patient's secondary policy is displayed. If the patient has no secondary policy, defaults to No Insurance/Self Pay. |
| Authorization |
The authorization or referral number used for the services. Typically, this number is assigned by the payer or utilization management organization to authorize a service prior to its being rendered. |
| Add new authorization | |
| Notes |
Enter any notes about the authorization. These notes appear on the Insurance Authorization page. |
| Type |
Select Pre-cert or Referral. |
| Insurance authorization number |
Enter the insurance authorization number. |
| Effective date |
Enter or select the effective dates for this authorization or referral. |
| Authorized visits/units |
Select Visits or Units from the menu, and then enter the number of approved units or visits in both fields. athenaOne automatically decrements the number of authorized visits or units.
If you select units, a procedure code is required. The count of remaining units decreases by the number of units associated with the procedure codes listed in the authorization, regardless of any other charge on the claim. For example, you first create an authorization using units = 10 and a procedure code of 99215. You then create a claim using this authorization where procedure code 99215 bills for 3 units. The authorization decreases by 3, and the remaining units on that authorization are now 7. |
| Referred-to provider |
Select the provider to whom the patient is being referred.This field automatically displays the name of the provider with whom you are scheduling the appointment. |
| Specialty |
Select the specialty of the provider to whom the patient is being referred. |
| Diagnosis code |
Enter or select the diagnosis code associated with the authorization. You can type a period to access the Diagnosis Lookup tool in the ICD-9 or ICD-10 fields. After you enter a diagnosis code, a description of the code is displayed to the right of it. Note: If the diagnosis code that you entered is not coded to the highest level of specificity, a warning to this effect appears next to the code. |
| Procedure code |
Enter or select the procedure codes associated with the referral. You can type a period to access the Procedure Lookup tool. After you enter a procedure code, a description of the code is displayed to the right of it. Note: The exact procedure code is required if you select Units from the Authorized visits/units menu. The procedure is validated against your fee schedule. |
| Additional information |
Enter any additional information that you want to record about this incoming authorization. |
| Provider | |
| Rendering provider |
The provider who renders services to the patient. This field is typically used for internal tracking and reporting purposes; the selected provider will generally not appear as the rendering provider on the claim. |
| Supervising provider |
The provider whose credentials you intend to submit on the claim. This can be the provider who supervised the services or an individual who was supervised by another provider. In either case, use this field to identify the provider that you want to submit on the claim. The provider you select using the Supervising provider field typically appears as the rendering provider on the claim. For example, on a CMS-1500 claim form, the provider you select using the Supervising provider field typically appears in Box 24J, and the provider's name appears in Box 31. Note: If the selected Rendering provider has a supervising provider, a note appears next to the Supervising provider field.
If you arrive at the Charge Entry page through the appointment or missing slips workflow, the default selection in the Supervising provider - Required field is as follows:
Important: Any provider whose credentials you intend to submit on claims must be configured as a supervisory provider type on the Providers page so that you can select that provider using the Supervising provider field. For example, you cannot select a physician's assistant with a provider type of PA, but you can select a physician's assistant with a provider type of PASUP.
The provider selected as the Rendering provider appears by default as the Supervising provider if the Rendering provider is one of the following provider types:
See the Providers page for more information about rendering and supervising providers.
Note: If the supervising provider is non-participating with a payer listed on the claim, their non-participation status is indicated. |
| Scheduling provider |
The provider or resource that was originally scheduled for this appointment. Principally recorded for reporting purposes, this provider does not generally appear on claims.
|
| Referring provider |
The provider who referred this patient for services. You can click Find a provider to display the referring provider lookup tool. |
| Illness/Injury | |
| Current illness date |
The date of onset of the current illness.LMP = Date of last menstrual period. ED = Estimated date of delivery. If the EDD is given, the LMP is automatically calculated using the OB feature. |
| Procedures |
Procedure code best identifying each medical service or medical supply provided. Note: If you enter more than six procedure codes on one claim, athenaOne generates an additional claim (or claims) to accommodate the charges. |
|---|---|
| Diagnosis codes | Enter the ICD-10 diagnosis code reference number justifying the procedure listed. (Enter only one code per text box.) |
| FP | Indicates that this line item is for family planning. |
| Other Diagnoses |
Use this section to record additional diagnosis codes that may be required by a payer to support value-based reimbursement but are not tied to a specific charge line or CPT code (for example, codes for pre-existing conditions). This section records any diagnoses entered on charge integration (Billing tab in athenaClinicals) that you have not associated with a procedure code. Also, you can manually enter diagnosis codes in this section to submit these codes on the claim without tying them to a specific charge line.
You can enter up to 12 diagnosis codes per claim. If the total number of diagnosis codes exceeds 12, athenaOne does not send all the diagnosis codes entered in this section on the claim. After you click Create Claim, athenaOne creates a new claim note to indicate which codes it was not able to add to the claim, and these codes move to the Internal Use - Other Diagnoses section, so that you can review them on the Claim Action or Claim Edit page.
You can enter up to 12 diagnosis codes per claim. If the total number of diagnosis codes exceeds 12, athenaOne automatically generates additional claims to accommodate the excess diagnoses which are not associated with a procedure billed on the claim, and links the diagnoses to placeholder procedure code 99499. After you click Create Claim, athenaOne automatically splits the claim and you can see a note automatically appear on Claim Edit.
When this feature creates a claim with related claims, the athenaOne system holds all claims together (and releases them together as well).
Ask athenahealth to enable the Automatically Split Claims with Excess Diagnoses Codes setting. Contact the CSC or your onboarding project team. On the Main Menu, click Support > Success Community > Contact Client Support Center.
Before you can use this feature, you must add placeholder procedure code 99499 in your fee schedule with a cost value greater than $0.00 and less than $1.00. For more information about Fee Schedules, see Fee Schedules in O-help.
Important If the placeholder procedure code 99499 is not in your fee schedule with a cost value greater than $0.00 and less than $1.00:
|
|
|
|
| Mark Appointments As Not Requiring Charge Entry | |
|
|
Checkboxes appear for any appointments scheduled for the patient on the same day and department, listed chronologically, including multi-resource slots.
These checkboxes reflect any selections made on the Check-in page. On the Charge Entry page, you need to select a reason for not requiring charge entry for any checked appointments (see below). |
| Reason |
Before you click the Mark Appointment As Not Requiring Charge Entry link, enter the reason why this claim does not require charge entry.
Tip: You can create custom "no charge entry reasons" via the No Charge Entry Reasons page. |
To enable service type add-ons, you must contact the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Note: Some service type add-ons are available only on the Claim Edit page (not on the Charge Entry page).
| Service Type Add-On — Abortion | |
|---|---|
| Special Program Code |
Select the reason the abortion services were performed. Compliant use of this field is applicable according to the state laws of each client, and may be provider-driven. Please consult your legal advisor or state healthcare agency for compliance guidelines. |
| Service Type Add-On — Anesthesia | |
| Surgeon |
Select the primary surgeon from the menu. This menu is populated from the Referring provider table. |
| Concurrency |
A claim level field typically populated by the value calculated in the anesthesia time sheet. When entering charges outside the anesthesia workflow, however, the practice user can enter the concurrency level, calculated manually, in this numeric field. |
| Anesthesia Type |
This value is typically populated from the anesthesia time sheet. But, the practice user can complete this field on the charge entry page. Further, rules can be conditioned on the anesthesia type selected. For example, if the practice user identifies the services as a monitored anesthesia case (MAC), a rule could be created to require the user to modify the anesthesia services with a MAC modifier. |
| Start Time |
The start time of an anesthesia case is entered in 24-hour format. Minutes are exclusive. A start time of 08:00 and end time of 08:30 returns total minutes of 30. |
| End Time |
The end time of an anesthesia case is entered in 24-hour format. Minutes are exclusive. A start time of 08:00 and end time of 08:30 returns total minutes of 30. |
| CPT Code |
Users entering anesthesia services using the Charge Entry page generally complete the Procedure code field with an ASA code. Practice users have the option of recording the surgical CPT code describing the patients surgery. Note: Although athenaOne does not systematically map CPT codes to ASA codes on the Charge Entry page, rules have been created to compare the two values when entered to ensure that they are appropriate. |
| Service Type Add-On — Breast Care | |
| TPL Denial Date |
The date the primary insurance denied the claim. (Note: TPL = Third Party Liability). |
| Result Code (Breast) |
Result code for breast or cervical procedures. Select from the menu of acceptable values provided by the Program. |
| Recommendation Code (Breast) |
Recommendation Code for breast or cervical procedures. Select from the menu of acceptable values provided by the Program. |
| Result Code (Cervical) |
Result code for breast or cervical procedure(s). Select from the menu of acceptable values provided by the Program. |
| Recommendation Code (Cervical) |
Recommendation Code for breast or cervical procedures. Select from the menu of acceptable values provided by the Program. |
| Months for Short-Term Follow-Up |
Required if recommendation code is 2. |
| Tumor Size (cm) |
Size of Tumor. Required for procedures 19160, 19162, 19180, 19240. |
| Tumor Stage |
Required if tumor size is present. |
| Treatment Started? |
Select Yes if surgery, chemotherapy, or radiation has been started; otherwise, select No. |
| Reason Code for No Treatment |
Select if treatment has not started. |
| Pap Smear Adequacy Code |
Select an acceptable value provided by the Program from the menu. |
| Service Type Add-On — Consultation | |
| Ordering Provider |
Enter the provider ordering services or supplies, if different from the rendering provider (Referring Provider Lookup tool available). This is required for HCPCS procedure codes that describe consultative services. Medicare claims require a referring provider and/or an ordering provider. |
| Second Opinion for Surgery |
Select Yes if the claim is for a second opinion for surgery; otherwise select No. |
| Service Type Add-On — Corporate Billing | |
| Test/Specimen Number |
Enter the test/specimen number in the field provided. Note: To enter additional notes in the Line note field, click edit (upper right corner of the charge line) and then click Add next to Line note. |
| Service Type Add-On — COVID-19 | |
| Was the patient suspected of having, diagnosed with, or tested for COVID-19 at the time of the encounter? |
Select Yes or No to indicate whether the claim is for services related to COVID‑19 care. If you select No, you cannot select answers in the remaining fields.
The athenahealth rules engine uses the answers to these questions to determine which COVID-19 related rules should fire on the claim, particularly when the patient is COVID-19 presumptive positive. You may notice a change in hold volume for claims related to COVID-19 care as rules adapt to changing payer requirements and as athenahealth gains more information about COVID-19 federal grant requirements. Note: You can use the Report Builder to report on the answers to this question in the COVID-19 service type add-on. The COVID-19 Suspected display column and filter are available in the Claim category of these report types in the Report Builder: Appointment, Claim, FCC Activity, Transaction Activity, and Transaction Aging. |
| Does this claim include services related to COVID‑19 testing? |
Select Yes or No.
The COVID-19 service type add-on appears on claims created with or without an appointment. Note: You can use the Report Builder to report on the answers to this question in the COVID-19 service type add-on. The COVID-19 Testing display column and filter are available in the Claim category of these report types in the Report Builder: Appointment, Claim, FCC Activity, Transaction Activity, and Transaction Aging. |
| Is the provider or medical group out-of-network with the patient's insurance? |
Select Yes or No.
You can use the answer to this question in conjunction with the COVID‑19 related patient balance hold to help you meet the CARES Act Provider Relief Fund grant requirements. For information about the COVID-19 related patient balance rule, see COVID-19 Management: Patient Balance Hold Rules Request on the Success Community. Note: You can use the Report Builder to report on the answers to this question in the COVID-19 service type add-on. The COVID-19 Out of Network display column and filter are available in the Claim category of these report types in the Report Builder: Appointment, Claim, FCC Activity, Transaction Activity, and Transaction Aging. |
| Service Type Add-On — Diagnostic Services | |
| Purchased Services? |
Select Yes for claims with modifier -90 (Reference (Outside) Laboratory). This indicates your practice has purchased testing kits from an outside party (CMS-1500 line 20 or equivalent). |
| Purchased Services Provider |
Select the provider supplying purchased services. For example, a physician may purchase a diagnostic exam from an outside entity. (Referring Provider Lookup tool available.) Required if Purchased Services? is set to Yes. |
| Ordering Provider |
Select the provider who ordered the services this is required if Purchased Services? is set to Yes. You can type a period to access the (Referring Provider Lookup tool. |
| Purchased Services Amount |
Enter the total cost (dollar amount) or the purchased services included on the claim. This is required if Purchased Services? is set to Yes. |
| Service Type Add-On — Dialysis | |
| Patient's Weight (pounds) |
Enter the patient's weight in pounds. This is required for EPO claims for patients on dialysis. |
| Service Type Add-On — DME | |
|
|
DME Section — This section of the add-on is used to report the length of need and certification type for DMERC CMNs excluding O2.
Complete the DME section fields only for procedures where a certificate of medical necessity (CMN) from the provider is required. For oxygen therapy claims, however, do not complete these fields. |
| DME Certification Type |
Code indicating the type of certification. |
| DME Certification Revision Date |
The date the last certification was obtained from the Provider. The DME Certification Revision date must be provided if you have indicated a DME Certification Type of Renewal or Revised. |
| DME CMN Quantity (months) |
Used to report the length of need for this CMN. Quantity is reported in months. Note: For the DME information to be submitted with a DME claim, you must complete both the DME certification type as well as the DME CMN quantity. |
| DME Therapy Begin Date |
The date DME therapy began. |
|
|
Oxygen Therapy — Used to report O2 CMN information. Required for all home oxygen therapy claims. |
| Oxygen Therapy Certification Type |
Code used to specify the type of certification. |
| Oxygen Therapy Certification Revision Date |
The date the last certification was obtained from the Provider. The Oxygen Therapy Certification Revision date must be provided if you have indicated an Oxygen Therapy Certification Type of Renewal or Revised. |
| Oxygen CMN Quantity (months) |
Used to report length of need for this CMN. Quantity is reported in months. Note: For the Oxygen therapy information to be submitted with a DME claim, you must complete both the Oxygen therapy certification type as well as the Oxygen CMN quantity. |
| ABG Test Results |
Used to report arterial blood gas result. |
| ABG Test Date |
The date of the arterial blood gas test. |
| Oxygen Test Condition |
Used to report condition under which test occurred. |
| Oxygen Saturation Test Results |
Used to report oxygen saturation blood result. |
| Oxygen Saturation Test Date |
The date of the oxygen saturation test. |
| Oxygen Flow Rate |
Valid values are 1 — 999 liters per minute and X for less than 1 liter per minute. |
| Oxygen Test Findings |
Used to answer questions 8, 9, and 10 of the Oxygen CMN. User can select multiple findings from the list. |
| Oxygen Therapy Begin Date |
The date oxygen therapy began. |
|
|
CRC DMERC Condition Indicators — Used to report conditions related to all DMERC CMNs. If either the DME section or the Oxygen therapy section is completed, this section of the add-on is required. |
| Type of Condition Indicator |
Qualifier specifying the use of this section of the add-on. |
| Conditions Apply? |
The "Condition Apply Y/N" flag is the ANSI Certification Condition Code applies indicator. A "Y" response indicates the condition codes in Condition Indicators Codes apply; an "N" response indicates the condition codes in do not apply. |
| Condition Indicators |
Condition Code describing either patient or equipment status. |
| Date Certification Signed by the Physician |
If you have indicated with a condition code that the 38-Certification signed by the physician is on file at the supplier's office, you must provide the date that the certification was signed by the physician. |
| Patient's Weight (pounds) |
Patients weight is required when submitting claims to Medicare Durable Medical Equipment Regional Carriers with certificates of medical necessity. |
|
|
Supporting Documentation — This section of the add-on is used to report responses to CMN questions. |
| Form Identifier |
Used to report the CMN form number. Must be a valid OMB approved CMN form number excluding alpha characters. |
| Question Number/Letter |
Used to report CMN question number. For multi-part questions that are not numbered individually, assign letters left to right, top to bottom, keeping question numbers constant. Must include both numbers and letters together in this field. |
| Response Code |
Used to report responses to any CMN question that requires a Y/N response. |
| Date |
Used to answer CMN questions that require a date response format. |
| Percent |
Used to answer CMN questions that require a percent response. |
| Additional Information |
Used to answer CMN questions that use a text or uncodified response format. Note: These information fields do not appear until a number is provided in the question number/letter field. |
| Service Type Add-On — Drug/Injectables | |
| Patient's Weight (pounds) |
Enter the patient's weight in pounds. |
| Service Type Add-On — EPSDT | |
| Complete EPSDT screen? | Select Yes to indicate that the physician completed the EPSDT screening. Select No to indicate that the physician did not complete the EPSDT screening. |
| Service Type Add-On — Family Planning | |
| Purpose of visit | Select the purpose of this visit from the menu. |
| Interpreter needed | Select Yes if the patient requires an interpreter. |
| Number of pregnancies | Enter the number of pregnancies the patient has had. |
| Number of births |
Enter the number of times the patient has given birth. |
| Last pregnancy ended | Select the date when the patient's last pregnancy ended. |
| Contraceptive (prior to visit) | Select the type of contraception (if any) used by the patient before the visit. |
| Contraceptive (after visit) | Select the type of contraception (if any) that the patient will use after the visit. |
| Give reason for "none" | If you selected none from the Contraceptive (after visit) menu, select the reason for this option from the menu. |
| Pregnancy test | Select the result of the administered pregnancy test (negative or positive). If no test was given, select not tested. |
| Pregnancy desirability |
Select the appropriate option for pregnancy desirability. |
| Routine medical services provided |
Select all routine medical services provided. |
| Other medical services provided | Select all other medical services provided. |
| Lab services provided |
Select all lab services provided. |
| Referring for non-family planning services | Select all referred non-family planning services. |
| STD tests/diagnoses |
Select all STD tests and diagnoses administered. |
| STD treatments | Select all STD treatments given. |
| HIV pre-test counseling |
Select Yes if HIV pre-test counseling was provided. |
| HIV test | Select Yes if an HIV test was administered. |
| HIV test result |
Select the result of an administered HIV test (negative or positive). If no test was given, select not tested. |
| HIV post-test counseling | Select Yes if HIV post-test counseling was provided. |
| Provider of medical services |
Select all providers of medical services. |
| Counseling services provided | Select all counseling services provided. |
| Provider of counseling services | Select all providers of counseling services. |
| Service Type Add-On — Foreign System Identifier | |
| Client System identifier |
By default, the value of this field is hidden unless the + is clicked. The values populating the Foreign System Identifier fields are controlled by the interface; however, users can manually modify these values.
Additional values can be stored at the charge level in addition to the claim level (see Foreign System Identifier field below). |
| Foreign System identifier |
This appears on the charge level so you can store a Foreign System Identifier for an individual charge. |
| Service Type Add-On — Hearing/Vision | |
| Prescription Date |
Enter the prescription date. Required if it was required in the Reserved(19) (remarks). |
| Service Type Add-On — Hospice/HHA | |
| Patient is Home Bound? |
Select Yes if the patient is homebound, otherwise select No. |
| Hospice/Home Health Agency |
Hospice or Home Health Agency name — click choose/view to select from a list.
Note: A claim rule assigns HOLD status to all claims billed with procedure codes 99374, 99375, 99377, 99378, G0179, G0180, G0181, and G0182 that do not contain the complete name and address of the Hospice/HHA facility and Medicare ID number. |
| Hospice ID Number |
Enter the 6-digit facility ID of the patient's hospice or home health agency.
Note: A new scrub rule assigns HOLD status to all claims billed with procedure codes 99374-99375, 99377-99378, G0179, G0180, G0181, and G0182 that do not contain the complete name and address of the Hospice/HHA facility and Medicare ID number. |
| Provider is a Hospice Employee? |
Select Yes if the provider is an employee of the hospice. This flag is necessary for all Medicare claims involving physician services to hospice patients. |
| Ordering Provider |
Select the provider ordering services or supplies; if different from the rendering provider, click choose/view to select from the Referring Provider Lookup tool. |
| Service Type Add-On — Immunization | |
| Immunization Lot Number |
Enter the serum lot number if required by state law for health data reporting. Note: You can report only one serum lot (or batch) number per claim. You must create an additional claim if you need to report a second serum batch number. |
| Service Type Add-On — Maternity | |
| Pregnant? |
This field is automatically populated with the information from the OB episode. Required in some states. Required for Indiana Medicaid. Required if LMP is entered. |
| Estimated Delivery Date |
This field is automatically populated with the date from the OB episode. |
| Last Menstrual Period |
This field is automatically populated with the date from the OB episode. |
| Delivering Provider |
Select Yes to indicate that the rendering provider on the claim is also the delivering provider. Select No to indicate that the rendering provider on the claim is not the delivering provider.
Note: When the provider of antepartum care is the same as the delivering provider, denials are common because of global coverage for pregnancies. For antepartum care, it is important to indicate when this is provided by the delivering provider. |
| Service Type Add-On — Medicaid TX | |
| Benefit code | Enter the benefit code specific to Medicaid TX. The code is required for certain types of claims only. |
| Service Type Add-On — Miscellaneous Fields | |
| Service Auth Exception Code |
Select the reason why a provider did not obtain a service authorization for a service that state law (for example, New York State Medicaid) requires an authorization. |
| Delay Reason Code |
Select the reason why a claim was filed past the filing date or the reason why a claim transmitted in response to a request for information was delayed. |
| Special Program Code |
Select the program under which services provided to the patient were performed. |
| Service Type Add-On — NDC | |
| NDC number |
NDC information is copied from your practice's fee schedule, unless you enter it manually.
When you enter a valid number in the NDC Number field, athenaOne displays the corresponding athenaCodesource trade name to the right of the field. This allows you to confirm that the NDC number entered is correct for the procedure code.
Note: NDC is an 11-digit number with the format "xxxxx-xxxx-xx." If one segment is not formatted correctly, add a leading "0" to that segment (for example, 12345-123-12 becomes 12345-0123-12). For more information, see NDC number formatting.
Note: To edit the NDC number or dosage for a procedure code, click the edit procedure fees link on the Fee Schedules page. |
| Drug name | The name of the drug. Unless entered manually, this field is populated automatically from your practice's fee schedule. |
| Unit price | The unit price that your practice paid for this drug. Unless entered manually, this field is populated automatically from your practice's fee schedule. |
| Dosage | The total amount dispensed, measured in the units selected in the menu to the right of the field. |
| Service Type Add-On — Newborn Care | |
| Patient's Weight (pounds) |
Enter the patient weight in pounds. |
| Service Type Add-On — No Surprises Act Consent | |
| Consented Amount ($) |
If a patient’s Out-of-Network Billing consented amount was entered in the appointment AND a signed consent form was attached, you’ll see that amount in this field.
Note: If no signed consent form was uploaded, the cost estimate will NOT carry over to the consented amount in Charge Entry, as it is assumed that the patient did not consent to paying Out-of-Network rates.
If a patient’s consented amount is missing at Charge Entry or Claim Edit: you can check the patient’s appointment to see if a signed consent form was attached, and then enter the consented amount.
For details, see the O-help topic: To view and edit patient's Out-of-Network Billing consented amount at Charge Entry or Claim Edit |
| Service Type Add-On — Ordering Provider | |
| Ordering Provider |
Provider ordering services or supplies if different from the rendering provider. You can type a period to access the Referring Provider Lookup tool. |
| Service Type Add-On — Paperwork | |
| Paper work |
Select Yes to indicate that additional documentation is required. |
| Attachment Control Number |
Enter a control number for the required attachment. |
| Attachment Type |
Select the type of paperwork attachment from the menu. |
| Attachment Transmission |
Select the means for transmitting the attachment paperwork. |
| Service Type Add-On — Podiatry | |
| Last Seen Date |
Enter the date last seen by the physician supervising care for the underlying condition. |
| Service Type Add-On — Post-Operative Care | |
| Assumed Care Date |
Enter the date care was assumed by another provider during post-operative care if the claim has Modifier 54 (for Surgical care only) or Modifier 55 (for post-operative care only). Required on Medicare claims involving shared post-operative care. See Relinquished Care Date (below). |
| Relinquished Care Date |
Enter the date that the provider filing the claim ceased post-operative care — (i.e., the last day of care by this provider) if the claim uses Modifier 54 (for Surgical care only) or Modifier 56 (for Pre-op management only). Required on Medicare claims involving shared post-operative care. See Assumed Care Date (above). |
| Service Type Add-On — Programs | |
| Program | Select the appropriate program from the menu. |
| Service Type Add-On — PT/OT | |
| Ordering Provider |
Select the provider ordering services or supplies if different from the rendering provider (Referring Provider Lookup tool available). |
| Date Last Seen |
Enter the date when patient was last seen by the ordering provider (above) who is supervising care for the underlying condition. |
| Service Type Add-On — Radiation Therapy | |
| Number of treatment sessions | Enter the number of radiation treatment sessions for the patient. |
| Supervising provider | Select the name of the supervising provider. |
| Interpreting provider | Select the name of the interpreting provider. |
| Number of patients served | Select the number of patients served from the menu. |
| Service Type Add-On — Reference Lab | |
| Reference Lab |
Select click the choose/view link in the Reference Lab service type add-on. Search by lab name or by CLIA number. If not found, click the add new referring provider link. |
| Service Type Add-On — Rehabilitation Services | |
| Ordering Provider |
Select the provider ordering services or supplies if different from the rendering provider (Referring Provider Lookup tool available). Required for procedure codes (HCPCS) that describe:
Medicare claims are placed in HOLD status if you have not entered either a referring provider and/or an ordering provider for the types of service described above. |
| Service Type Add-On — Spinal Manipulation | |
| Initial Treatment Date |
Date spinal manipulation services were initiated. |
| Last X-Ray Date |
Date last X-ray was taken (for example, to demonstrate a subluxation of the spine). |
| Spinal Man. Patient Condition |
Describes the nature of the patient's condition necessitating spinal manipulation.
CODE NAME A Acute Condition C Chronic Condition D Non-acute E Non-Life Threatening F Routine G Symptomatic M Acute Manifestation of a Chronic Condition |
| Spinal Man. Patient Condition Description |
Free-form description to clarify patient's spinal manipulation condition. |
| Acute Manifestation Date |
Date the patient's condition became acute. |
| Service Type Add-On — Telehealth | |
| Were services rendered via a live telehealth distant site visit? |
Select Yes or No. The Telehealth service type add-on appears only when the claim is created without an appointment. If an appointment is associated with the claim, the appointment should have the Telehealth Distant Site Visit appointment type class applied (see To add Telehealth Distant Site Visit to your available appointment types). Note: The athenahealth rules engine uses the Telehealth Distant Site Visit appointment type class or the Telehealth service type add-on information to identify the claim as telehealth and apply the appropriate billing rules per payer guidelines. |
| Service Type Add-On — Title X Family Planning | |
| English proficiency | Select Yes if an interpreter is needed. |
| Primary method of family planning | Select the patient's primary method of family planning. |
| Clinical breast exam (CBE) |
Select the Received option if the patient received a clinical breast exam during the visit. |
| Credited family planning encounter provider | Select the provider credited for the family planning encounter. |
| Service Type Add-On — UDS Reporting | |
| UDS Visit Type | Visit type selected by athenaOne based on procedure code and provider. |
| UDS Visit Type Override |
Select the override type from the menu. To exclude the visit from UDS reporting, select Non-UDS Visit from the menu. Note: The UDS STAO works only on claims. If you create a clinical encounter with no associated claim, athenaOne automatically flags the encounter as a UDS visit type for reporting, and you cannot change the visit type in athenaOne. Your UDS report details (filtered and raw files) will include all encounters, in addition to claims. |
| Clinic or Virtual |
Visit type (Clinic or Virtual) selected by athenaOne based on the department's place of service code (POS 02 - Telehealth), certain modifiers on procedure codes on the claim or encounter (.GT, .G0, or .95), or certain procedure codes. Virtual visits are reported on UDS Table 5 - Staffing and Utilization. Note: You can find the list of virtual-only procedure codes on the 2019 CPT inclusion and exclusion list on the Success Community. |
| Clinic or Virtual Override |
To override the value in the Clinic or Virtual field of the UDS STAO, select Clinic or Virtual from the menu. |
| Internal note | Enter a note to document the UDS visit override. |
| Service Type Add-On — Well Child Care | |
| EPSDT Referral Given? |
Indicates whether an EPSDT referral was given to the patient. |
| EPSDT Referral Reason |
Indicate reason why an EPSDT referral was given. Required if an EPSDT referral was given. |
| EPSDT Referral Reason |
Indicate second reason why an EPSDT referral was given. |
| EPSDT Referral Reason |
Indicate third reason why an EPSDT referral was given. |
| Internal Use (Information entered below will not be included on claim) | |
| Other diagnoses | Enter any other diagnosis related to this claim. |
| Note | Enter any notes about this claim (does not appear as a claim note). |
| Post date |
The post date of the charges. The default value is the current date.
Note: In athenaOne, a charge whose post date is in the month following the month of its service date (or any subsequent month following the service date). A charge is considered late even if the service was at the very end of a month and the post date is at the beginning of the next month.
You can choose to back-date the charge to either the earliest open date in the system or the charge's (from) date of service, whichever is later. |
| Claim note | Enter a claim note. |