 User Guide — Chronic Care Management
User Guide — Chronic Care Management
If your practice serves patients with two or more chronic conditions, Medicare reimbursement rules for chronic care management services allow you to be reimbursed for the non-face-to-face work that you perform to manage the care of these chronically ill patients.
The 2015 Medicare Physician Fee Schedule Final Rule allows providers that see patients with two or more chronic conditions to be reimbursed for the non-face-to-face work that they perform to manage the care of these chronically ill patients. The following CPT procedure codes are used for chronic care management (CCM) services: 99490, 99487, and 99489.
If your practice serves patients with two or more chronic conditions and you want to take advantage of the Medicare reimbursement rules for chronic care management services, you can indicate whether a patient has agreed to receive these services using the Chronic Care Management field on the Quickview, Check-in, or Checkout page. You must manually update a patient's chronic care management status; athenaOne does not automatically determine this status.
To begin configuring athenaOne for chronic care management, practices can activate the Chronic Care Management program on the Care Program Configuration page.
Note: The Chronic Care Management field appears only if the patient has Medicare Part B or Medicare Advantage (Medicare Part B requires that patient consent be documented in the EHR). However, payers other than Medicare pay for CCM services.
To begin configuring athenaOne for chronic care management, practices should activate the Chronic Care Management global program on the Care Program Configuration page. This page allows you to activate and deactivate global and local care programs to control which programs appear in your care team's downstream workflows.
-
For step-by-step instructions on activating a care program, see Quick Reference — To make a care program active or inactive.
-
For more details on configuring care programs in athenaOne, see Care Program Configuration.
After you activate CCM on the Care Program Configuration page, your practice has access to encounter plans and templates designed specifically to support CCM workflows. For more details on the items available for CCM encounters, see Encounter plan and templates for CCM.
For instructions on the recommended configurations available for CCM, see the following sections:
After your practice activates CCM on the Care Program Configuration page, the following items are available for CCM encounters.
Care Management encounter plan
The Care Management encounter plan is listed on the Manage My Encounter Plans page (On the Main Menu, click Settings![]() > Encounter Plans).
> Encounter Plans).
The encounter reason (Reasons for visit field) is set to "chronic care management," and the encounter plan action (Structured Templates field) is set to SH: Care Management.
The text macro "ASMT: caremanagementAP" is associated with the Care Management encounter plan.
Social History template for Care Management encounters
The Care Management social history template is available after your practice activates CCM on the Care Program Configuration page.
.
To see the Care Management social history template: On the Main Menu, click Settings![]() > Clinicals. In the left menu,under Practice Links — History/Intake, click Social
History Local Templates.
> Clinicals. In the left menu,under Practice Links — History/Intake, click Social
History Local Templates.
History of Present Illness templates for Care Management encounters
When your practice activates CCM, the following HPI templates are available.
- Care Management – Acquired Hypothyroidism
- Care Management – Anxiety/Depression
- Care Management – Asthma
- Care Management – Atrial Fibrillation
- Care Management – Chronic Obstructive Pulmonary Disease (COPD)
- Care Management – Congestive Heart Failure (CHF)
- Care Management – Coronary Artery Disease (CAD)
- Care Management – Diabetes
- Care Management – Esophageal Reflux
- Care Management – General
- Care Management – Hyperlipidemia
- Care Management – Hypertension
- Care Management – Pressure Ulcer
- Care Management – Valvular Heart Disease
- Care Management – Vitamin D Deficiency/Osteoporosis
To see the Care Management HPI templates: On the Main Menu, click Settings![]() > Clinicals. In the left menu,under Practice Links — Exam, click History
of Present Illness Templates.
> Clinicals. In the left menu,under Practice Links — Exam, click History
of Present Illness Templates.
Chronic Care Management Consent
When your practice activates CCM, the Chronic Care Management field on the Quickview, Check-in, and Checkout pages is enabled for every patient with Medicare (both Medicare Part B and Medicare Advantage). You use this field to document the CCM enrollment status of these patients.
For more information, see the Chronic Care Management History page.
We highly recommend that practices create a new appointment type exclusively for CCM (non-face-to-face) encounters. This CCM appointment type can be used to build reports that identify patients who are part of the CCM program. At the end of every calendar month, you can run reports to identify patients who were scheduled for the CCM appointment type (see the "Reports for chronic care management services" section).
- Display the Appointment Types page: On the Main Menu, click Settings
 >Schedule. In the left menu,under Practice Links — Scheduling, click Appointment
Types.
>Schedule. In the left menu,under Practice Links — Scheduling, click Appointment
Types. - Click Add new.
- Name — Enter a name for the appointment type, for example, Chronic Care Management.
- Short name — Enter a unique short name that is four characters or fewer, for example, CCM. This short name appears in the Today's Appointments worklist and in the schedule.
Note: Choose this name carefully: after you create the appointment type, you cannot edit the Short name. - Duration — Enter the duration of the appointment type, in minutes.
Tip: Set the duration to 5 minutes in order to schedule as many CCM appointments on the first day of the month as possible. - Notes — You can enter notes for the CCM appointment type. These notes appear on the confirmation page after you schedule an appointment.
Scheduling
- Accept the default values for these fields:
- Patient time — Yes
- Generic slot — No
- Restrict search results — No
- Template only — No
- Billing slip required — Yes
- Click Save.
The Exam-Only Visit layout is used for appointments that will be documented only by the provider and includes the Check-in, Exam, Sign-off, and Checkout stages.
- Display the
Assign
Appointment Types to Layouts page: On the Main Menu, click Settings
 > Clinicals. In the left menu, under Practice Links — Chart/Encounter, click Assign
Appointment Types to Layouts.
> Clinicals. In the left menu, under Practice Links — Chart/Encounter, click Assign
Appointment Types to Layouts. - Layout — Select Exam-Only Visit from the menu.
- Specialty — You can select a specialty.
- Assign appointment types to encounter layout — Select CCM - CHRONIC CARE MANAGEMENT.
- Click Add.
We recommend that you create a non-person provider for each department that provides CCM services. Use this non-person provider exclusively for CCM encounters. The designated CCM non-person provider has these advantages:
- Organizing your schedule: When documenting CCM services, your practice will add many encounters to your daily queue. Using a non-person provider, all CCM appointments will appear in the schedule under a single heading (CCM). Your practice can quickly see which patients have appointments for CCM, thus allowing providers and care managers to better track CCM services.
- Organizing the Clinical Inbox: Any provider offering CCM services can send all care management encounters to a single work queue in the Clinical Inbox.
- Updating encounters: Any provider who needs to review or update a care management encounter can quickly locate it in the Chronic Care Management queue of the Clinical Inbox.
- Deactivating reminder calls: For practices using athenaCommunicator, reminder calls can be deactivated at the provider level. In this way, CCM patients will not receive reminder calls for in-office appointments that they do not have.
Note: Reminder calls can also be deactivated for CCM appointment types (see the ReminderCall Settings page).
Important: The non-person CCM provider is intended to serve as a scheduling resource and is not credentialed to bill for services. Your practice must change the rendering provider at Check-In.
Creating a CCM department
For practices with dedicated care management resources, adding an entire Care Management department designated exclusively for CCM encounters may be preferable to adding individual, non-person providers to each department.
Before you create the CCM non-person provider, you need to create a new practice role.
- Display the Practice
Roles page: On the Main Menu, click Settings
 > Clinicals. In the left menu,under Practice Links — Other, click Practice
Roles.
> Clinicals. In the left menu,under Practice Links — Other, click Practice
Roles. - Name
— Enter a name for the practice role, for example, caremanagement.
Names must be in lowercase letters with no spaces or punctuation. - Users — Select the users to assign to this practice role, that is, any users who will provide care management services.
- Department — Click All to use this role in all departments, or click Selected and then select the departments that will use the role.
Note: This option appears only if the Department Login Permissions feature is enabled for your practice. - Click Save.
These instructions provide guidance for creating a non-person provider for CCM. For complete instructions on creating a non-person provider, see To add a non-person scheduling resource provider — athenaCollector.
- Display the Providers
page: On the Main Menu, click Settings
 >Billing. In the left menu, under Practice Links — Providers, click Providers.
>Billing. In the left menu, under Practice Links — Providers, click Providers. - Click Add Without Guided Setup.
- Click Add provider. Additional fields appear.
- Entity Type — Select Non-person.
Basic information
- Name 1 — Enter a descriptive name such as CHRONIC CARE MANAGEMENT or CCM.
Billing
- Billed name — Enter the provider's name as it should appear on paper claims and statements (typically this name matches the Name 1 field).
- Credentials — Leave this box unchecked.
Note: Make sure this option is deselected; billing cannot be done using this non-person provider name. - Missing Slips Worklist — Select this option to track CCM services on the Missing Slips worklist in the Workflow Dashboard.
Workflow
- Scheduling name — Enter the scheduling name for this resource, for example, Care Management. This name appears in menus and on appointment and scheduling pages to identify the provider.
- Practice role — Select the practice role that you created for CCM services.
Patient Communication
- Patient Portal — Deselect the Display this provider in the Patient Portal option to exclude the CCM non-person provider name from the Patient Portal.
Note: This field appears only if you have the athenaCommunicator functionality. - Click Save.
If your practice uses the athenaCommunicator service and you create a CCM non-person provider, we strongly recommend that you deactivate ReminderCall phone calls, emails, and text messages for the CCM non-person provider.
To deactivate ReminderCall for the CCM non-person provider, follow these instructions.
- Display the ReminderCall Settings page: On the Main Menu, click Settings
 >Communicator. In the left menu,under Practice Links — ReminderCall, click ReminderCall Settings.
>Communicator. In the left menu,under Practice Links — ReminderCall, click ReminderCall Settings. - Filter by — Select Provider from the menu.
The list of providers appears on the right side of the page. - Select the CCM non-person provider from the list, and then click Filter.
- Click Edit.
Note: If the CCM provider appears in more than one department, click Bulk Edit to deactivate ReminderCall messages for the CCM provider in all departments. - Under the Calls heading, select Use custom settings and disable the Enable phone calls field (uncheck the box).
- Under the Emails heading, select Use custom settings and disable the Enable emails field (uncheck the box).
- Under the Text Messages heading, select Use custom settings and disable the Enable text messages field (uncheck the box).
- Click Save.
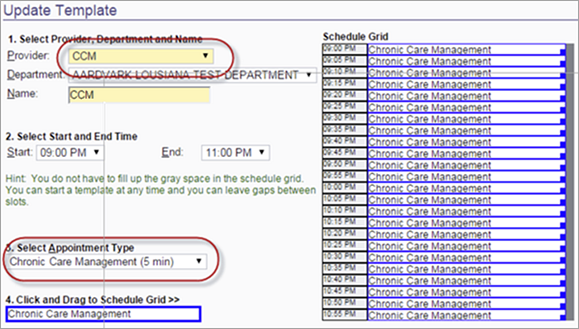
You need to create a schedule for daily appointments for the CCM non-person provider.
Consider scheduling your CCM appointments outside normal office appointment hours in 5‑minute slots that are essentially "dummy appointments." In this way, you can schedule as many appointments on the first day of the month as possible without affecting your regular schedule.
Patients scheduled for CCM appointments can be checked in for the appointment at any time during the day on which an encounter is scheduled, so you can document CCM services at any time thereafter.
On the Build & Apply Templates page, you can select the CCM non-person provider and the Chronic Care Management appointment, or you can add a new schedule template and configure it to resemble this one.
Procedure codes 99490, 99487, and 99489 should be added to the practice's fee schedule per the practice's usual and customary rate. For more information about these CPT codes, see the Guide to Success: CCM with athenahealth on the Success Community.
- CPT code 99490 is the code for CCM services (20 minutes spent and documented for care coordination services in a calendar month).
- CPT code 99487 is available for complex CCM lasting 60+ minutes.
- CPT code 99489 is available for complex CCM that extends an additional 30 minutes beyond the 60 minutes covered by CPT code 99487.
For information about how to add a procedure fee entry to a fee schedule, see To add a procedure fee to a fee schedule.
Patient-facing description field
CCM services are subject to the Medicare Part B 20% coinsurance. Use the Patient-facing description field (which appears on patient statements) to describe the non-face-to-face care coordination included in the claim, so that patients understand why they are receiving a statement when they may not have visited the office.
You can use existing athenaOne workflows for chronic care management. The high-level workflow for chronic care management follows these basic steps.
- Schedule CCM eligible patients for a CCM appointment at the beginning of every calendar month.
- Document and record any CCM services in this encounter; leave the encounter open for the duration of the month.
- At the end of the month, close the encounter and submit a claim if the monthly CCM criteria have been met (otherwise, close the encounter but do not submit a claim).
Note: athenahealth Marketplace partners offer enhanced automation of the CCM process. For more information, please visit the athenahealth Marketplace and select the Chronic Care Management filter.
To access resources on athenaOne features and workflows related to chronic care management, see Additional resources.
Two reports support chronic care management services. You can find these reports on the Other tab in the Report Library.
- Chronic Care Management Eligible Patients — This report identifies all Medicare patients who may be eligible to receive chronic care management services. Eligible patients have two or more chronic conditions identified by the Department of Health and Human Services on historical claims. You can filter the report by Insurance Reporting Category to display patients potentially eligible for CCM by payer.
- Medicare Chronic Care Management Claims Eligible to be Created — This report identifies Medicare patients who can be billed for chronic care management services.
Activate these reports using the Activate Reports page (On the Main Menu, click Settings![]() >Implementation. In the left menu, under Practice Links — Reports, click Activate
Reports).
>Implementation. In the left menu, under Practice Links — Reports, click Activate
Reports).
To ensure that as many eligible Medicare patients as possible receive CCM services, athenahealth recommends that you automate report delivery on a monthly basis to the appropriate practice users.
In addition to the standard CCM reports, we also recommend that you create a report using the Report Builder to quickly identify closed CCM encounters that do not yet have a claim associated with them.
- Display the Report Builder page: On the Main Menu, click Reports. Under General, click Report Builder.
- Select the Clinicals report type.
- Click the Choose Display Columns tab.
- Select these display columns to include in the report:
- Patient > Patient ID
- Patient > Patient Name
- Clinical Encounter > Chief Complaint
- Clinical Encounter > Clinical Encounter Created
- Appointment > Appointment Type
- Click the Choose & Set Filters tab.
- Select the filters to use in the report:
- Appointment > Appointment Type.
Select Chronic Care Management (20 min) from the Filter Criteria menu. - Clinical Encounter > Clinical Encounter Created.
Specify the date range for the current month. - Save the report.
- Report Name — Enter a name such as "Chronic Care Management Encounter List."
- Report Category — Accept the default report category (Other).
- Report Section — Accept the default value (Practice Report).
- Click Save.
- To run the report, display the Report Library, locate the report on the Other tab, and run it.
7 Hills Medical Center plans to submit claims to Medicare and other payers for chronic care management services provided to their patients.
- Dr. Christa Jones, a provider at 7 Hills Medical Center, runs the Chronic Care Management Eligible Patients report to identify all patients who may be eligible to receive chronic care management services. Eligible patients have two or more chronic conditions.
- When Dr. Jones next sees one of the identified patients, Robert Hall, she explains to him how he can benefit from the covered CCM services, which include better care coordination and 20 minutes
of remote care management every 30 days. She asks Robert whether he wants to receive these services.
Note: CCM services are described in the 2015 CMS Physician Fee Schedule (PFS) Final Rule. - Robert agrees to participate in the chronic care management program and signs the required consent form.
- Andi Ames, a receptionist for the practice, updates Robert's CCM status.
- On Robert's Quickview page, Andi clicks Update status/view history to the right of the Chronic Care Management field.
- On the Chronic Care Management History page, she clicks the Enrollment status menu and selects Enrolled.
- She clicks Change Status and then clicks back to return to the Quickview.
- Once a month, Jesse Leroux, a billing specialist, runs the Medicare Chronic Care Management Claims Eligible to be Created report to identify patients who should be billed for CCM services.
- For each patient in the report results, Jesse confirms that the required 20 minutes of work were completed to satisfy the CCM requirements outlined in the 2015 CMS PFS Final Rule.
- Jesse creates claims using the new procedure code (99490), along with the diagnosis codes that describe the patient's chronic conditions.
Following are some common questions about the CCM workflow.
No. The athenahealth recommended workflow is exactly that — a recommendation. Practices can use as much of our workflow as they choose; however, our recommended workflow was designed to ensure that users capture the information required by CMS.
Note: athenahealth Marketplace partners offer enhanced automation of the CCM process. For more information, visit the athenahealth Marketplace and select the Chronic Care Management filter.
The CCM consent field appears only for patients enrolled in Medicare (Medicare Part B or Medicare Advantage). You can suggest enhancements to CCM functionality on the Ideas page of the Success Community.
CPT codes cannot be tied to appointment types, but they can be tied to procedure templates. If your practice wants to automate billing, you can create a dummy procedure template, tie it to code 99490, and add it to the Care Management encounter plan such that the procedure template and code are automatically included when the care management encounter reason is selected.
athenaClinicals requires that the rendering provider for an encounter be an actual person. For this reason, users cannot select the CCM non-person provider as the rendering provider. We recommend that you select the patient's primary provider as the rendering provider and the CCM non-person provider as the scheduling provider. The encounter should still be left in review to the care management practice role so that the encounter can be easily located by any provider who might need to make updates.
For more details on athenaOne features and workflows related to chronic care management, see the following resources in O-help:
- athenaClinicals Care Plan
- Care Plan Report
- Care Program Configuration
- Care Programs Panel
- Care Section